Lymph node removal (lymphadenectomy)
Your health expert: Mr Christian Macutkiewicz, Consultant General and Hepato-Pancreatico-Biliary Surgeon
Content editor review by Pippa Coulter, July 2022
Next review due July 2025
Lymph node removal is a surgical procedure to take out one or more of your lymph nodes. Your doctor may recommend you have this procedure if you’ve been diagnosed with cancer. It can help to check whether cancer has spread, or reduce the chance of it coming back.
About lymph node removal
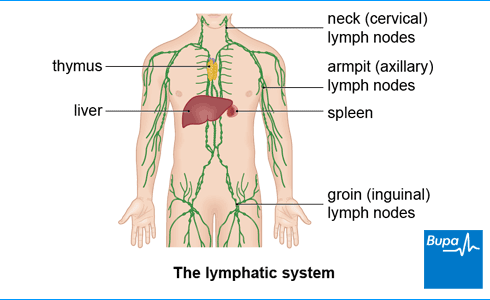
Lymph nodes are small, kidney bean-shaped organs found throughout your body, including in your armpits, neck and groin. They are part of the lymphatic system. This is a network of thin tubes that carries a clear fluid called lymph, containing waste from cells around your body, back to your bloodstream.
Your lymph nodes help to fight infection and filter lymph fluid. They trap any bacteria and waste products in lymph and destroy old or abnormal cells, such as cancer cells.
Why are lymph nodes removed?
Many types of cancer spread through the lymphatic system and nearby lymph nodes are one of the first places they spread to. If you have cancer, there are two main reasons why your doctor may suggest removing lymph nodes.
- One or more lymph nodes may be removed to check whether your cancer has spread. Knowing this helps your doctor plan the best treatment for you.
- If tests have shown that the cancer has reached your lymph nodes, you may have them taken out to remove the cancer. This helps to reduce the chance of your cancer coming back.
Lymph nodes can often become swollen due to infection, as well as autoimmune diseases, and more rarely, cancer. Having swollen lymph nodes doesn’t mean that you’ll necessarily need your lymph nodes removed. Swollen lymph nodes often get better on their own. But if they don’t after a few weeks, contact your GP.
Where are lymph nodes removed from?
Where your lymph nodes will be removed from depends on the type of cancer you have. Common areas for lymph node removal include your:
- armpit, for breast cancer
- neck, for head and neck, and thyroid cancers
- groin, for cancers of the penis, anus and vulva
- abdomen, for testicular or ovarian cancers
- back passage, for bowel cancer
Surgery to remove lymph nodes may be done at the same time as your main surgery for cancer. Or, it may be done as a separate procedure.
Medical terms used in lymph node removal
You may hear a number of different medical terms used when describing lymph node removal. Here are some of the most common ones and what they mean.
- Lymphadenectomy – the medical term for lymph node removal.
- Lymph node biopsy – just one or two nodes are removed to check for cancer cells.
- Sentinel lymph node – this is the first lymph node your cancer is likely to spread to.
- Sentinel lymph node biopsy – removal of the sentinel lymph node. It’s usually done if you have breast cancer or melanoma (skin cancer).
- Lymph node dissection (or clearance) – this is when all the lymph nodes in a particular area are removed. An example is axillary lymph node dissection for breast cancer. In this procedure, your surgeon removes a number of lymph nodes from your armpit (axilla).
Preparing for lymph node removal
Your doctor will talk to you about why they’re recommending lymph node removal, including the benefits and risks involved. They’ll explain exactly what will happen before, during and after your procedure. Be sure to ask your doctor any questions you have. It’s important that you feel fully informed, as you’ll need to give your consent for the procedure to go ahead.
Getting healthy for surgery
Your doctor or nurse will explain how to prepare for your procedure. They might advise you on things you can do before surgery to improve your general health and make your recovery easier and faster. This might include aiming to get to a healthy weight, being active, and if you smoke, stopping smoking. Smoking increases your risk of getting a chest and wound infection, and slows healing time.
You’ll probably be invited to a pre-admission assessment clinic at the hospital a week or two before your operation. Here, a nurse will do some general checks and tests to make sure you’re well enough for surgery.
Preparing for your hospital stay
You will usually need a general anaesthetic, for lymph node removal, especially if you’re having many lymph nodes removed. This means you’ll be asleep during the procedure. With a general anaesthetic, you’ll need to stop eating and drinking for a period of time beforehand. Your hospital will give you clear instructions on when. It’s important to follow this advice.
Although some lymph node surgeries can be done as a day-case, you will often need to stay in hospital for one or more nights. Your healthcare team should let you know what to expect. If you need to, make arrangements for a stay in hospital and for help at home afterwards.
At the hospital
On the day of your procedure, your surgeon or nurse will check you’re feeling well and happy to go ahead. The staff at the hospital will do any final checks and get you ready for surgery. They may ask you to wear compression stockings, or have an injection of an anticlotting medicines, to help prevent deep vein thrombosis (DVT).
If you’re having a sentinel lymph node biopsy, you may need to have a scan before your operation, to help find the sentinel node. This involves having an injection of a tracer (a radioactive liquid) that can show up on a scan. The radiographer who performs the scan will be able to identify the sentinel node as the first lymph node that the radioactive liquid goes into. They may mark its position on your skin for your surgeon to see.
Looking for cancer cover that supports you every step of the way?
If you develop new conditions in the future, you can rest assured that our health insurance comes with full cancer cover as standard.
To get a quote or to make an enquiry, call us on 0808 273 6216∧
What happens during lymph node removal?
Exactly what happens during your surgery will depend on a number of things, including how many lymph nodes are being removed and where they are. If you’re having a sentinel lymph node removed, your surgeon may inject a special blue dye into the area of your cancer. This travels to the sentinel lymph node and dyes it blue, which makes it easier for your surgeon to find it.
Lymph node removal can be carried out via open or keyhole surgery. Which you have will depend on the area of the body being operated on.
In open surgery, your surgeon will make a cut in the affected area and identify the lymph nodes they’re going to remove. They’ll then carefully remove them and possibly some other tissue nearby that may have cancer cells. Your surgeon may put a fine tube (called a drain) in place, to drain fluid from your wound. This will be taken out after a few days. At the end of the operation, your surgeon will close the cut with dissolvable stitches, non-dissolvable stitches, staples or skin glue.
In keyhole surgery, your surgeon will make a small cut (or cuts) in the affected area. They’ll use surgical instruments (including a camera) passed through the cuts to view your lymph nodes and remove them.
What to expect after lymph node removal
How long you need to stay in hospital depends on the type of surgery you’ve had. For some procedures, you might be able to go home on the same day, while for others you may need to stay for one or more nights. Your healthcare team will let you know how long you should expect to stay in hospital for.
Recovering from the anaesthetic
How long you need to stay in hospital depends on the type of lymph node removal operation you had. You might be able to go home the same day or you may need to stay longer. Ask your surgeon how long you’ll need to stay in hospital for.
If you’ve had a general anaesthetic, you’ll need to rest until the effects wear off. You might have some discomfort as the anaesthetic wears off, but you’ll be offered pain relief if you need it. .
You might find that you’re not so co-ordinated or that it’s difficult to think clearly after a general anaesthetic. This should pass within 24 hours. In the meantime, don’t drive, drink alcohol, operate machinery or sign anything important. If you’re going home the same day as your general anaesthetic, you’ll need to arrange for someone to drive you. This is a good idea even if you had a local anaesthetic. You should also have an adult stay with you for the first 24 hours.
Taking care of your wound
You’ll be given advice about caring for a surgical wound before you go home, as well as a date for a follow-up appointment. If you have a drain from your wound, you’ll usually have it removed after a few days. You’ll have a dressing covering your wound. Your nurse or surgeon will tell you when you can remove this.
If your surgeon used dissolvable stitches to close your cut, these won’t need to be removed. They’ll usually dissolve completely within a few weeks, depending on which type your surgeon used. If you had non-dissolvable stitches or staples, you’ll need to have these removed after a week or so. If you have skin glue, this should flake off on its own over two to three weeks.
Getting your results
After surgery, your lymph nodes will be sent to a laboratory to test for cancer cells. Results are usually sent to the doctor who requested your procedure. Your doctor will talk to you about your results at your follow-up appointment – this might be about two weeks after your surgery.
Recovering from lymph node removal
You are likely to have some pain and discomfort for a while after your operation. Your wound may be sore and swollen. If you need pain relief, you can take over-the-counter painkillers such as paracetamol or ibuprofen. Always read the patient information that comes with your medicine and if you have any questions, ask your pharmacist for advice.
Any other effects that you may have after your operation will depend on where your lymph nodes were removed from. For instance, side-effects of lymph node removal in your armpit may include stiffness in your shoulder. You can do exercises to help with this. After lymph node removal from your neck, you may have some weakness on one side of your mouth. This usually returns to normal in a few months.
How long it takes to recover after lymph node removal surgery will depend on your circumstances and type of surgery you’ve had. It might just take a couple of weeks after lymph node surgery for melanoma, for example. But it may be several months for more major surgery, like lymph node removal for testicular or breast cancer. Ask your surgeon when you’re likely to be able to get back to your usual activities, including returning to work. Check if there are any restrictions on what you can do while you’re recovering like strenuous exercise or heavy lifting.
Complications of lymph node removal
Complications are when problems occur during or after the operation. Complications of having your lymph nodes removed can include the following.
- An infection in your wound. You may need antibiotics to treat this.
- A build-up of fluid in the area around the lymph node area (seroma). This usually goes within a few weeks but your surgeon may need to drain it.
- Injury to nerves near the site of your operation. This may make your skin feel numb or cause problems with movement, such as stiffness.
- Persistent pain. This may be due to damage to the tissues, a nerve or scar tissue forming. Pain can sometimes continue to be a problem for months or even years after your surgery. Your doctor or nurse can advise on exercises to help manage pain, or prescribe painkillers if necessary.
- Lymphoedema. This is a build-up of lymph fluid in an area of your body – often an arm or leg. It can be a long-term side-effect of lymph node removal. It happens because lymph fluid can’t drain away as well once your lymph nodes are removed.
You’re more likely to develop lymphoedema if you have several lymph nodes removed and if you have radiotherapy. You’ll continue to be at risk of developing lymphoedema for the rest of your life after having lymph nodes removed. But there are many things you can do to keep this risk as low as possible. These include keeping to a healthy weight and being active.
Sepsis (adults)
Sepsis is a life-threatening complication that can develop if you get an infection. Sepsis is a medical emergency. Call 999 or go to A&E immediately if you have any of the following symptoms.
- Slurred speech, confusion, difficulty making sense.
- Extreme shivering or muscle pain.
- Passing no pee (urine) during a day.
- Severe difficulty breathing, feeling breathless, or breathing very fast.
- It feels like you’re going to die.
- Skin changes such as your skin looking blue, pale or blotchy, or a rash that does not fade when you roll a glass over it.
In a sentinel node biopsy, your surgeon may use a radioactive tracer or dye to show up the lymph node nearest to your cancer. This is the sentinel node. Your surgeon will remove the sentinel lymph node, and send it to a laboratory to test for cancer cells. Read more in our section, What happens during lymph node removal?
Having swollen lymph nodes doesn’t necessarily mean that you need to have them removed. It depends on what’s causing them. Swollen lymph nodes are most commonly caused by infection and usually get better on their own. If the swelling hasn’t gone away within a few weeks, speak to your GP. Read more in our About section.
This depends on the area that’s been operated on and whether you’re having any other surgery. Some people feel back to normal within a couple of weeks. But it’s possible for pain to continue for weeks or even months. You can find out more in the section on Recovery, above
You’re likely to feel sore and have some discomfort after your lymph node removal. There’s a risk of complications such as infection and ongoing pain, too. You’ll also have a long-term risk of lymphoedema– a build-up of lymph fluid. Your doctor or nurse will give you advice on how to manage these problems.
Lymphoedema
Lymphoedema is the build-up of a fluid called lymph, which causes a body part to swell up.
Breast cancer
Did our Lymph node removal (lymphadenectomy) information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Mulita F, Mukkamalla SKR. Lymph node dissection. StatPearls Publishing.
www.ncbi.nlm.nih.gov/books, last updated 7 November 2021 - Sevensma KE, Lewis CR. Axillary sentinel lymph node biopsy. StatPearls Publishing.
www.ncbi.nlm.nih.gov/books, last updated 2 May 2022 - Toomey A, Lewis CR. Axillary lymphadenectomy. StatPearls Publishing.
www.ncbi.nlm.nih.gov/books, last updated 2 May 2022 - The lymphatic system and cancer. Cancer Research UK. www.cancerresearchuk.org last reviewed 29 July 2020
- Surgery to remove lymph nodes. Cancer Research UK. httwww.cancerresearchuk.org, last reviewed 10 July 2020
- Generalised lymphadenopathy. Patient.co.uk. patient.info/doctor, last edited 29 March 2019
- Maini R, Nagalli S. Lymphadenopathy. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 25 November 2021
- Delibegovic S. Introduction to total mesorectal excision. Med Arch 2017; 71(6):434–38. doi:10.5455/medarh.2017.71.434–38
- Surgery for head and neck cancer. Macmillan Cancer Support. www.macmillan.org.uk, last reviewed 31 July 2019
- Retroperitoneal lymph node dissection (RPLND). Macmillan Cancer Support.
www.macmillan.org.uk, last reviewed 31 August 2018 - Good surgical practice. 3.5.1 Consent. The Royal College of Surgeons, September 2014.
www.rcseng.ac.uk - Preparing for surgery. Macmillan Cancer Support. www.macmillan.org.uk, last reviewed 1 January 2020
- Anaesthesia explained. Royal College of Anaesthetists, January 2021. www.rcoa.ac.uk
- You and your anaesthetic. Royal College of Anaesthetists, February 2020. www.rcoa.ac.uk
- Personal communication. Mr Christian Macutkiewicz, Consultant General and Hepato-Pancreatico-Biliary Surgeon, 14 July 2022
- Laparoscopic pelvic lymph node dissection. Medscape. emedicine.medscape.com, last updated 26 February 2020
- Caring for someone recovering from a general anaesthetic or sedation. Royal College of Anaesthetists, November 2021. www.rcoa.ac.uk
- Surgical wounds – principles of wound management. Oxford handbook of adult nursing. Oxford Medicine Online. oxfordmedicine.com, published online June 2018
- Surgery to remove the lymph nodes for melanoma. Macmillan Cancer Support.
www.macmillan.org.uk, last reviewed 1 July 2019 - General surgery. Oxford handbook of operative surgery. Oxford Medicine Online, published online May 2017
- Mejdahl MK, Andersen KG, Gärtner R, et al. Persistent pain and sensory disturbances after treatment for breast cancer: six year nationwide follow-up study. BMJ 2013; 346:f1865. doi: 10.1136/bmj.f1865
- Lasting pain after breast surgery or lymph node removal. Breast Cancer Now.
breastcancernow.org, last reviewed June 2019 - Sleigh BC, Manna B. Lymphedema. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 4 June 2021
- For people at risk of lymphedema. American Cancer Society. www.cancer.org, last revised 25 May 2021

