Skin cancer (non-melanoma)
Your health expert: Dr Veronique Bataille, Consultant Dermatologist
Content editor review by Rachael Mayfield-Blake, April 2022
Next review due April 2025
Non-melanoma skin cancer is cancer that starts in the top layers of your skin. It usually develops on areas of your body that are regularly exposed to the sun, such as your face. But you can also get skin cancer on other areas, for example your neck, hands, back lower legs and forearms.
About non-melanoma skin cancer
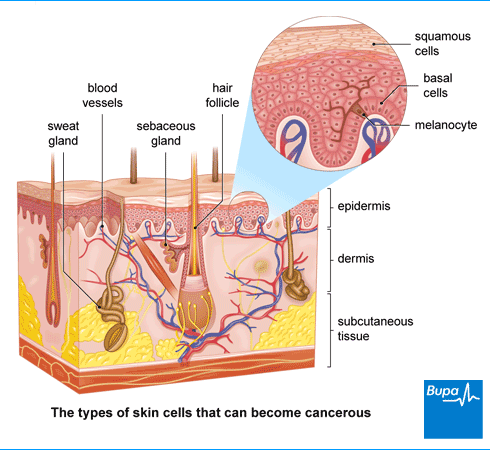
If you have non-melanoma skin cancer, the cells that form the upper layers of your skin grow out of control and form cancerous areas or lumps. These cells are known as basal cells and squamous cells.
Non-melanoma skin cancers can usually be cured, often with a small surgical procedure.
You might sometimes hear of another type of skin cancer called melanoma. Melanoma skin cancer is a less common, but more serious type of skin cancer, which starts in skin cells called melanocytes.
Types of non-melanoma skin cancer
The two main types of non-melanoma skin cancer form in cells in the top layer of your skin (the epidermis).
Basal cell carcinoma
Basal cell carcinoma (BCC) is a type of skin cancer that starts in the basal cells, which form the bottom layer of your epidermis. It’s the most common form of skin cancer. Around 75,000 people are diagnosed with BCCs each year in the UK.
BCCs grow slowly and don’t usually spread to other parts of your body, but they can grow into the healthy tissues surrounding the site of the cancer. These types of cancer are most common in middle-aged and elderly people, although they are becoming more common in younger people.
Squamous cell carcinoma
Squamous cell carcinoma (SCC) is a type of skin cancer that starts in the squamous cells, which form the upper layer of your epidermis. About 25,000 SCCs are diagnosed in the UK every year.
Squamous cell carcinomas (SCCs) usually grow more quickly than basal cell carcinomas (BCCs) and may spread into other parts of your body. You’re also more likely to get an SCC as you get older.
Causes of non-melanoma skin cancer
Too much exposure to ultraviolet (UV) radiation from the sun or sunbeds is one of the main ‘environmental’ causes of all types of skin cancer.
Having a lot of exposure to the sun over time puts you at greater risk of developing non-melanoma cancer.
You’re at greater risk of non-melanoma skin cancer if you.
- Burn easily. Usually if you have pale skin and fair hair.
- Have had a lot of exposure to the sun. For instance, if you work outdoors, have outdoor hobbies, regularly sunbathe or you live in a country near the equator.
- Are older. If you’re older, you’ve had more exposure to the sun and are more likely to have damage to your cells over time from biological processes. You’re also more likely to have had exposure to things that increase your risk.
- Have a weakened immune system. This could be because you take medicines that suppress your immune system, or have a disease that affects your immune system.
Sometimes, squamous cell carcinoma (SCC) can develop if your skin has been damaged in other ways. For instance, damage from other forms of radiation, burns or persistent ulcers and wounds in your skin. Viruses, such as the human papillomavirus infection (HPV) may also increase your risk of SCC.
How cancer develops
Cancer explained | Watch in 1:48 minutes
In this video, we explain how, when cells divide uncontrollably, this leads to cancer.
Symptoms of non-melanoma skin cancer
Skin cancer symptoms vary a lot between people. If you have skin cancer, you’re likely to notice that an area of your skin looks different. You might have a new lump on your skin, a scaly, itchy or crusty raised area of skin or a scab that doesn’t heal, for example.
Basal cell carcinomas and squamous cell carcinomas look a bit different.
Basal cell carcinomas may look like:
- small, pale, slow-growing lumps or ulcers
- a scaly, red plaque (bumpy patch of skin)
Squamous cell carcinomas may look like:
- a lump with hard, scaling or crusting skin on top
- a small, red lump which quickly gets bigger
With either type of non-melanoma skin cancer, you may notice the lump or area of skin breaks your skin (ulcerates) and crusts or bleeds. This may heal, and then break again repeatedly.
A new mole or change in an existing mole (for example, a change in size, shape or colour) can be the first sign of a different type of cancer called melanoma. This is a more serious type of skin cancer.
If you notice anything unusual on your skin, it’s important to get it checked out with a doctor, particularly if it doesn’t heal, or gets worse over time.
Inside health: myth busting skin cancer
Skin cancer | Myths | Watch in 13:03 minutes
Dr Zoe Williams talks to Dr Petra Simic about symptoms, causes and common myths about skin cancer.
Looking for fast access to quality care?
If you’re worried you might have cancer, you can call us directly, and as long as your symptoms are covered under your policy we can often authorise a consultation without the need for a GP referral.
To get a quote or to make an enquiry, call us on 0808 273 6216∧
Diagnosis of non-melanoma skin cancer
A GP will ask you about your symptoms and examine you. They may ask you questions about your medical history, and about how much exposure you’ve had to the sun or sunbeds in the past.
The GP may suspect you have a non-melanoma skin cancer just from how it looks. But you’ll need to have a biopsy to confirm the diagnosis. This involves taking a sample of tissue (your skin), which will be sent to a laboratory to be tested for cancer cells. Your GP will refer you to see a specialist doctor for a biopsy.
Excision biopsy
If the area is small and easy to access, you may be able to have what’s called an excision biopsy. Your doctor may remove the whole area of skin that looks cancerous in a biopsy, along with some healthy skin. This may be all you need – so diagnosis and treatment can be done at the same time.
Punch or shave biopsy
Sometimes, your doctor may remove just a sample of the affected skin in either a punch biopsy or a shave biopsy.
- In a punch biopsy, your doctor will remove a small circle of the full thickness of your skin.
- In a shave biopsy, your doctor will shave (slice) off the top layer of your skin or lesion.
You’ll then need further treatment once your diagnosis is confirmed.
Scans
You won’t usually need any further tests if you’ve been diagnosed with a non-melanoma skin cancer. But sometimes, you may need tests to check if it has spread.
Treatment of non-melanoma skin cancer
Non-melanoma skin cancer treatment is often with minor surgery. But there are alternatives to surgery that may be a better option for you. The treatment you have will depend on:
- the type of skin cancer you have
- your general health
- the position and size of your cancer, and how deeply it has grown into your skin and surrounding tissues
Your doctor will discuss your treatment options with you.
Surgery
Excision
An excision is a procedure to remove the cancer, along with some of the surrounding healthy skin to make sure it’s completely removed. This is the most common treatment both for basal skin carcinoma and squamous cell carcinoma, and often it’s the only treatment you’ll need. A small wound can be closed with stitches, but if you have a large area of skin removed, you may need a skin graft or flap. See our FAQs below for more information about skin grafts and skin flaps.
Mohs surgery
This is a more specialised type of surgery. You may have it for a basal cell carcinoma or squamous cell carcinoma in an area that’s difficult to treat, such as your head or neck. You may also have Mohs surgery if your cancer has come back.
In Mohs surgery, your surgeon will remove layers of the affected skin in stages. They’ll look at the layer they’ve removed under a microscope straightaway to check if all the cancer has gone. They’ll repeat this until they’ve taken away all the cancer.
Curettage and electrocautery
You may have this treatment if you have basal cell carcinoma or a small squamous cell carcinoma. It involves scraping away the affected part of your skin, layer by layer, using either a small spoon shaped tool or ring shaped blade (curette). Your surgeon will then use an electric probe to destroy any cancer cells left behind.
Non-surgical treatments
Non-surgical treatments may be an option if you have low-risk non-melanoma skin cancer, and these include the following.
- Cryotherapy – this treatment uses liquid nitrogen to freeze the affected area of your skin and destroy the cancerous cells.
- Creams that you put on your skin – this could either be a medicine that stimulates your immune system), or a type of chemotherapy.
- Photodynamic therapy – this is light therapy to kill cancer cells, in combination with a medicine to make your skin more sensitive to the light.
- Radiotherapy – this uses radiation to destroy cancer cells.
Advanced skin cancer
Your doctor may offer you radiotherapy and/or chemotherapy alongside other treatments if you have a squamous cell carcinoma that has spread to other parts of your body. But it’s rare for SCC to spread.
Prevention of non-melanoma skin cancer
The following tips may help to protect your skin from burning and reduce your risk of developing skin cancer.
- Cover up in the sun with suitable clothing, including a wide-brimmed hat and ultraviolet-protective sunglasses.
- If you can, try not to spend long in in the midday sun when the sun is at its strongest – stay in the shade when you’re out.
- Use high-factor sun lotion if you’re out in strong sunlight, with a sun protection factor (SPF) of at least 30, and a star rating of 4 or 5.
- Don’t use sunbeds.
If you have patches of sun-damaged skin, known as an actinic keratosis, it’s important to get this treated to reduce the chance of it turning into a squamous cell carcinoma. Speak to a GP if you think you have this.
If you have skin cancer surgically removed, some healthy skin may be removed too. If this is a large area and can’t heal, your surgeon may need to replace the skin with a skin graft or skin flap. A skin graft is a thin layer of skin taken from another area of your body, and a skin flap is a thicker layer of skin than a graft, taken from a nearby area.
Yes, it’s usually possible to cure non-melanoma skin cancer – it’s very rarely life-threatening. Basal cell carcinomas (BCCs) can almost always be cured. Most squamous cell carcinomas (SCCs) can usually be cured too. But a very small number of SCCs can spread to other parts of the body and can be life-threatening. As they’re potentially more dangerous, your GP will give you an urgent referral to a specialist.
The two most common types of non-melanoma skin cancer are basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). Around 75,000 people are diagnosed with BCC each year in the UK, and about 25,000 people are diagnosed with SCC.
See our section: Types of non-melanoma skin cancer above for more information.
Non-melanoma skin cancer symptoms can vary in people, and there are also some differences in how basal cell carcinomas look in comparison to squamous cell carcinomas. But you might have a new lump on your skin, a scaly, itchy or crusty raised area of skin or a scab that doesn’t heal, for example.
See our section: Symptoms of non-melanoma skin cancer above for more information.
Chemotherapy
Radiotherapy
Did our Skin cancer (non-melanoma) information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Basal cell carcinoma. BMJ Best Practice. bestpractice.bmj.com, last reviewed 28 February 2022
- Squamous cell carcinoma of the skin. BMJ Best Practice. bestpractice.bmj.com, last reviewed 28 February 2022
- Basal cell carcinoma. Patient. patient.info/doctor, last edited 26 November 2021
- Squamous cell carcinoma of skin. Patient. patient.info/doctor, last edited 26 November 2021
- Overview of skin cancer. BMJ Best Practice. bestpractice.bmj.com, last reviewed 28 February 2022
- Types of skin cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 24 September 2019
- Basal cell carcinoma. Medscape. emedicine.medscape.com, updated 14 February 2022
- Skin cancers – recognition and referral. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised February 2021
- Squamous cell carcinoma overview. Skin Cancer Foundation. www.skincancer.org, last updated January 2022
- Skin cancers. Oxford handbook of oncology. Oxford Medicine Online. oxfordmedicine.com, published online October 2018
- Non-melanoma skin cancer incidence statistics. Cancer Research UK. www.cancerresearchuk.org, last reviewed 4 October 2019
- Risks and causes of skin cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 24 October 2019
- Skin cancer symptoms. Cancer Research UK. www.cancerresearchuk.org, last reviewed 16 September 2019
- Basal cell carcinoma. MSD Manual Professional Version. www.msdmanuals.com, last full review/revision December 2020
- Squamous cell carcinoma. MSD Manual Professional Version. www.msdmanuals.com, last full review/revision December 2020
- Tests to diagnose skin cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 20 September 2019
- Types of surgery for larger skin cancers. Cancer Research UK. www.cancerresearchuk.org, last reviewed 23 October 2020
- Surgery for small skin cancers. Cancer Research UK. www.cancerresearchuk.org, last reviewed 7 October 2019
- Personal communication, Dr Veronique Bataille, Consultant Dermatologist, 26 April 2022
- The sunscreen fact sheet. British Association of Dermatologists. www.skinhealthinfo.org.uk, accessed 31 March 2022


