Irritable bowel syndrome (IBS)
Your health expert: Dr Sukh Chatu, Consultant Gastroenterologist
Content editor review by Pippa Coulter, August 2023
Next review due August 2026
Irritable bowel syndrome (IBS) is a common disorder of the digestive system. It causes symptoms like tummy pain or discomfort and a change in your bowel habits. IBS is often something you have for years or sometimes for life. But there are ways to manage your symptoms.
About irritable bowel syndrome
In irritable bowel syndrome (IBS), several changes seem to happen to your bowel. These can include the following.
- Your bowel may become more sensitive than normal. It might over-react to certain foods or other factors such as emotional stress.
- Your brain may process pain from your bowel differently.
- Changes to the bacteria and viruses living in your bowel.
- Changes in how food moves through your digestive tract.
These changes cause IBS symptoms. IBS disrupts how your brain and your bowel interact. This is sometimes known as the brain–gut axis, or brain–gut connection. It can explain why things like stress may trigger IBS symptoms.
IBS is something you’re likely to live with for years, often for life. Your symptoms will usually come and go over this time. Some people’s symptoms improve over time while others get worse. Sometimes, IBS goes away on its own.
Around 1 in 5 adults in the UK are thought to have IBS. It may be even more common than this, because not everyone seeks medical advice for their symptoms. Women are more likely than men to have IBS. You can develop it at any age, but it’s most common for symptoms to start in your 20s or 30s. It’s less common for IBS to start later in life.
It’s also possible for children to develop IBS. Around 1 in 6 children of secondary school age report IBS-like symptoms. Young children may not be able to accurately describe their symptoms, which makes it harder to identify IBS.
Causes of irritable bowel syndrome
It’s not fully understood why some people develop irritable bowel syndrome (IBS). No single cause has been identified. But it often seems to be triggered by one of the following.
- An infection of your stomach or bowels (gastroenteritis).
- Inflammation resulting from another condition such as inflammatory bowel disease.
- Taking medicines that affect your bowel, including antibiotics.
You may be more likely to develop IBS if someone else in your family has it. But no genetic link has been identified yet.
If you have IBS, you might find certain foods or drinks trigger your symptoms. These often include fatty or spicy foods, alcohol, and caffeine. Feelings of stress, anxiety, and depression can also worsen symptoms.
Irritable bowel syndrome symptoms
Irritable bowel syndrome (IBS) symptoms vary from one person to another. Some people only get mild symptoms, while others have symptoms severe enough to affect their daily life. The main symptoms of IBS include the following.
- Pain or discomfort in your tummy (abdomen). You may feel this as cramps low down or in the middle of your tummy. The pain may be worse after eating and may get better after you’ve had a poo. In some people, the pain may get worse when they have a poo.
- Changes in bowel habits, meaning how often you need to go for a poo and whether it’s hard or less firm. Around a third of people with IBS have constipation, a third have diarrhoea, and a third have a mix of both. You may also pass small amounts of mucus.
- Your abdomen may look and feel bloated. This can get worse during the day and may improve when you go for a poo or pass wind. This symptom is less common in children.
You’ll often find your symptoms get worse during times of stress and after eating certain foods. These can include fatty and spicy foods.
IBS can cause other symptoms too. These are common in adults with IBS, but rare in children. They include:
- feeling like you have no energy (lethargy)
- indigestion
- feeling sick
- backache
- headaches
- bladder symptoms, such as needing to pee more often and urgently
When to see a GP
If you’ve been getting symptoms like those described above for several weeks, you should see your GP. They may want to do some tests to rule out other causes of your symptoms.
Several other conditions can cause symptoms like those in IBS. These include coeliac disease and inflammatory bowel disease (IBD). IBD includes Crohn’s disease and ulcerative colitis. Like IBS, coeliac disease and IBD can cause tummy pain and a change in bowel habits. But they are caused by different things. In IBD, it's inflammation in your bowel that causes symptoms. People with coeliac disease have an immune reaction to gluten in the diet. IBD can also cause other symptoms, like bleeding from your back passage.
Bowel symptoms like tummy pain and a change in bowel habits can also be symptoms of bowel cancer. The risk of bowel cancer becomes greater as you get older. This means it’s particularly important to see your GP if you develop bowel symptoms for the first time and you’re over the age of 40. If you have bleeding from your back passage in addition to other bowel symptoms, always get it checked with your GP, whatever your age.
What should I do if I'm embarrassed to talk to my doctor?
Seeing a doctor when you're embarrassed | Watch in 2:08 minutes
Dr Naveen Puri talks about how to make it easier to see a doctor about a health issue when you are feeling embarrassed.
Hello, I am Dr Naveen Puri, I am one of the GPs within Bupa Health Clinics.
Today I want to speak to you about embarrassing problems you might have and what we can do if you attend one of our clinics.
I want you to know that many people feel embarrassed or concerned about speaking about certain things with their doctors, but I'm here to reassure you these are the kinds of things we deal with every day.
For me, looking at someone's bottom or their breasts or their genitalia is no different to looking at their nose or elbow.
And that's true for all doctors as we train for many years in these parts of the body and are very used to having these conversations with people just like you.
So what I would encourage you to do if you have any concerns from your perspective, be it a change in your bowel habit, be it a lump, a rash, a swelling. Something on your genitalia or a part of your body you're not particularly familiar with or feel uncomfortable discussing.
Please be assured your doctor has done it all before.
Some of the ways we find patients find it easier to speak to a doctor is to either tell the doctor you feel embarrassed up front. That way a doctor can make extra effort to make sure you feel comfortable.
Or some patients come to us with pieces of paper and will write the problem down and hand it to us. That way we can help with whatever is going on for you as well.
You may also find it helpful to ask for a specific doctor, someone you're familiar with in your practice. Or you might want to ask for a doctor of a specific gender, or background to your liking as well.
I'd also say, doctors do this every day so don't be alarmed if we ask you certain questions around your symptoms. It is purely so we can help you get the best outcome for your enquiry.
And then finally, feel free to use language that suits you as well. We don't expect you to know the medical words for things, or a name for your diagnosis. That's our job to find out for you.
So, take your time, see a doctor, and hopefully we can help put your mind at ease.
Diagnosis of irritable bowel syndrome
Your GP will usually be able to diagnose irritable bowel syndrome (IBS) by asking you about your symptoms. They will ask you questions about your medical and family history too. Sometimes they may need to do some tests to rule out other conditions. Your doctor may diagnose IBS if you’ve had IBS symptoms for six months or more, and there are no signs to suggest any other condition.
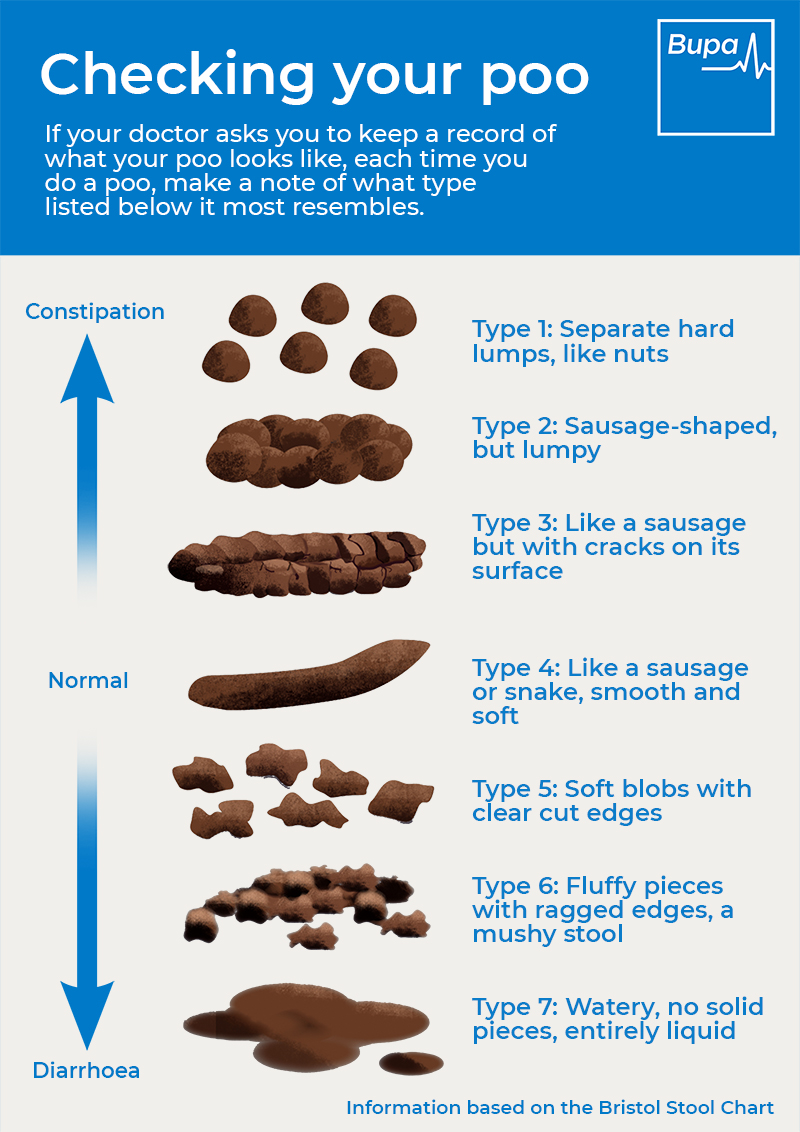
Your GP will ask you to describe your symptoms and how long you’ve had them, when you notice them, and what makes them better or worse. This might include any food or drinks linked to your symptoms. They’ll want to know about any changes in how often you need to go for a poo and what it looks like. For help describing your poo, you can use our 'checking your poo' infographic.
Infographic: Checking your poo
Bupa's 'Checking your poo' infographic (PDF, 1.8MB), helps you understand what’s normal, and what is constipation or diarrhoea.
Normal poo is smooth and sausage shaped. If your poo is very hard and lumpy this might be a sign of constipation. If your poo is watery and loose this might be diarrhoea.
Your GP will want to know how your symptoms affect your daily life. They may also ask you how you’ve been feeling recently – including if you have any stress or anxiety. It can be useful to keep a record of your symptoms and any possible triggers for a few weeks to share with your GP. There are online and app-based food diaries available or you can try our downloadable symptoms diary (PDF, 1MB).
Your GP may also want to examine you to rule out other possible causes. This may involve feeling your tummy and checking your weight . They may also ask to do an examination of your back passage. They’ll explain what this involves and ask for your consent beforehand.
Your GP may ask you to have blood tests and to provide a poo sample to check for other conditions, like coeliac disease and inflammatory bowel disease (IBD). They may refer you to a specialist doctor for more tests if your symptoms need further investigation. Further tests might include a colonoscopy to check for IBD.
Need a GP appointment? Telephone or Video GP service
With our GP services, we aim to give you an appointment the same day, subject to availability.
To book or to make an enquiry, call us on 0343 253 8381∧
Diet and lifestyle changes for IBS
There’s no cure for irritable bowel syndrome (IBS), but you can make changes to your diet and lifestyle which may improve your symptoms. Your GP is likely to talk you through some of these before suggesting any other treatments.
Diet advice
You may find some of the following dietary measures help. What works for you may depend on your main symptoms, particularly whether you mostly get constipation or diarrhoea.- Eat regular meals and give yourself plenty of time to eat them. Avoid missing meals or leaving long gaps between eating.
- Make sure you’re drinking enough fluid to keep hydrated. Cut back on fizzy drinks, alcohol and drinks containing caffeine – for example, tea and coffee.
- If you mainly have diarrhoea and bloating, it may help to reduce the amount of fibre you eat. This includes cutting back on high-fibre foods such as brown rice and wholemeal bread.
- If you suffer more with constipation, try gradually increasing your intake of fibre. Aim to include wholegrains, oats, vegetables, and fruits. Don’t have more than three portions of fruit a day though. You can also try soluble fibre supplements such as ispaghula, although these may sometimes make symptoms worse.
- Try to limit the amount of processed food you eat. These foods often contain ‘resistant starch’ that’s difficult for your body to digest.
- If you have diarrhoea, avoid sorbitol. This is used in some sugar-free sweets, chewing gum, and drinks.
- If you have wind and bloating, try incorporating oats into your diet – for example, oat-based cereals. Linseeds (up to a tablespoon a day) can also help.
- You might want to try taking probiotics – for example, probiotic yoghurts and food supplements. Probiotics contain ‘good’ bacteria that improve the balance of bacteria in your gut. If you try them, do so for at least 12 weeks, and stop taking them after this if they aren’t helping.
Avoiding common triggers
If the advice above hasn’t helped, your GP may refer you to a dietitian for specialist advice. A dietitian may recommend you try an exclusion diet. This means cutting out certain foods to see if it helps.
One particular exclusion diet is known as the low FODMAP diet. FODMAP stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. These are all types of carbohydrate that can be hard to digest and may cause IBS symptoms. Examples include:
- fruits, including apples, cherries, peaches, and nectarines
- artificial sweeteners
- foods containing lactose – for example, milk and dairy products
- pulses such as beans and lentils
- vegetables such as broccoli and cabbage, onion, and garlic
- wheat
In the FODMAP diet, you cut out these foods and then gradually reintroduce them to see what you can tolerate. It should only be done under guidance from a health professional such as a dietitian.
Some people with IBS may find that a gluten-free diet helps. But it doesn’t work for everyone, so doctors don’t usually recommend it. Don’t cut out any foods until you’ve seen a GP or dietitian.
Lifestyle advice
Your GP may discuss other changes you can make to your lifestyle. These might include trying to be more active. Regular exercise may help to reduce your symptoms. Any exercise is beneficial but a good target to aim for is 150 minutes of moderate exercise over the course of a week.
Your GP may also encourage you to lose weight if you’re overweight or obese.
Think about ways that you can manage any stress, anxiety,, or depression if any these seem to be triggering your symptoms. You could try some relaxation techniques such as mindfulness, meditation, or yoga.
Irritable bowel syndrome treatment
If diet and lifestyle changes don’t help your irritable bowel syndrome (IBS) symptoms, your GP may suggest other treatments. These include medicines and talking therapies. The treatments you’re offered will depend on your symptoms and what’s causing them.
Medicines
Medicines that can help with IBS symptoms include the following.
- Laxatives such as polyethylene glycol (PEG) or linaclotide. These make it easier to pass a poo, helping with constipation.
- Antidiarrhoeal medicines such as loperamide.
- Antispasmodic medicines such as mebeverine hydrochloride, alverine citrate, and peppermint oil capsules. These can help with tummy pain and wind.
Many of these medicines are available over the counter (without a prescription). Ask your pharmacist for advice about what you need. In some cases, your GP may prescribe medicines.
If the medicines listed above don’t ease your symptoms, your GP may also offer you a low-dose antidepressant. Antidepressant medicines don’t just help with depression. They’re also known as neuromodulators. They can help with the pain you get in IBS by making the gut less sensitive. They can help with IBS even if you don’t have anxiety or depression. Your doctor will want to monitor you regularly.
Talking therapies
Sometimes, your GP or specialist may recommend trying a talking therapy. They may suggest this if you still have symptoms after trying the measures above.
Talking therapies include cognitive behavioural therapy (CBT), hypnotherapy, and psychotherapy. These therapies may look at how you deal with stress and how this triggers IBS symptoms. They may also help you to cope better with your IBS symptoms.
Yes, it’s possible for children to have IBS. It’s most common to develop IBS in your 20s or 30s, but it can start in childhood. Children experience tummy pain and constipation or diarrhoea, like adults. They may be less likely to have bloating and other symptoms though. If your child is getting regular symptoms, contact their GP.
See our About section to find out more.
There isn’t much good-quality evidence to confirm if probiotics can help with symptoms of IBS. But some research has shown that they may be helpful, especially with bloating.
If you decide to try probiotics for IBS, it’s recommended to take them for at least 12 weeks to see if they help. A dietitian may advise a stronger probiotic if they feel it would help.
You can find out more in our section on diet and lifestyle.
In inflammatory bowel disease (IBD), your symptoms are caused by inflammation in your bowel. In irritable bowel syndrome (IBS), a disruption between your brain and bowel leads to symptoms. IBD can cause certain symptoms that you don’t get with IBS – for example, bleeding from your back passage.
Our section on symptoms has more information on the different conditions that cause bowel symptoms
The three main symptoms doctors look for in irritable bowel syndrome (IBS) include:
- pain or discomfort in your tummy
- your tummy looking bloated
- a change in bowel habits – for example, constipation or diarrhoea
There can be other symptoms too. Read our section on symptoms to find out more.
Certain things have been associated with triggering irritable bowel syndrome (IBS). These include a stomach infection, inflammation due to another condition and taking certain medicines. If you have IBS, certain foods or feeling stressed or anxious may trigger a flare-up.
Our section on causes has more information.
Irritable bowel syndrome (IBS) is different for everyone. Some people may get mild symptoms. Others may have symptoms so severe that they interfere with everyday life. You may get diarrhoea or constipation or a mix of both. You may get tummy pains and bloating too.
For more information see our section on symptoms.
Why is fibre important?
Fibre is a plant-based carbohydrate found in foods such as wholegrains and vegetables, also described as roughage. Many of us don’t get enough fibre in our diets.
Gastroenteritis
Gastroenteritis is inflammation of your stomach or bowels (your gastrointestinal tract). It’s usually caused by an infection.
Did our Irritable bowel syndrome (IBS) information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Irritable bowel syndrome. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised September 2022
- Irritable bowel syndrome. Patient. patient.info, last updated 11 June 2021
- Irritable bowel syndrome. BMJ Best Practice. bestpractice.bmj.com, last reviewed 12 June 2023
- Irritable bowel syndrome and diet: food fact sheet. British Dietetic Association. www.bda.uk.com, last reviewed January 2022
- Irritable bowel syndrome. NICE British National Formulary for Children. bnfc.nice.org.uk, last updated 28 June 2023
- Pediatric irritable bowel syndrome (IBS). Medscape. emedicine.medscape.com, updated 6 June 2022
- Coeliac disease. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised May 2020
- Crohn's disease. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised August 2020
- Ulcerative colitis. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised April 2020
- Coeliac disease. Definition. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised May 2020
- Suspected cancer: recognition and referral. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 15 December 2021
- Bowel cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 3 December 2021
- Irritable bowel syndrome in adults: diagnosis and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 4 April 2017
- Vasant DH, Paine PA, Black CJ, et al. British Society of Gastroenterology guidelines on the management of irritable bowel syndrome. Gut 2021; 70(7):1214–40. doi: 10.1136/gutjnl-2021-324598
- Constipation. NICE British National Formulary. bnf.nice.org.uk, last updated 28 June 2023
- Probiotics and gut health: food fact sheet. British Dietetic Association. www.bda.uk.com, July 2022
- Usai-Satta P, Bassotti G, Bellini M, et al. Irritable bowel syndrome and gluten-related disorders. Nutrients. 2020; 12(4):1117. doi: 10.3390/nu12041117
- Physical activity guidelines: UK Chief Medical Officers' report. gov.uk, published 7 September 2019
- Irritable bowel syndrome. NICE British National Formulary. bnf.nice.org.uk, last updated 28 June 2023
- Ballou S, Keefer L. Psychological interventions for irritable bowel syndrome and inflammatory bowel diseases. Clin Transl Gastroenterol 2017; 8(1):e214. doi: 10.1038/ctg.2016.69

