Heart attack
Your health expert: Dr Tim Cripps, Consultant Cardiologist
Content editor review by Pippa Coulter, Freelance Health Editor, November 2022
Next review due November 2025
A heart attack is a serious medical condition which happens when the blood supply to part of your heart gets blocked. A heart attack can be life-threatening. The sooner you get treatment for a heart attack, the better your chances of survival.
How a heart attack occurs
Animation | Heart attack | Watch in 1:54 minutes
Discover what happens during a heart attack, and what can cause one.
What is a heart attack?
Heart attacks are usually caused by coronary heart disease (CHD). This is when your coronary arteries get clogged up with fatty deposits called plaques. This causes the coronary arteries to narrow. Your coronary arteries supply your heart muscle with blood and oxygen. A heart attack usually happens when a plaque splits, causing a blood clot to form over the top. The blood clot can block your coronary artery. This stops blood flow to your heart muscle.
The risk of having a heart attack increases as you get older. Heart attacks are more common in men than women, especially at a younger age. Women are more likely to have one once they have gone through the menopause.
Causes of a heart attack
Developing coronary heart disease puts you at risk of heart attack. Certain things that make you more likely to develop coronary heart disease are out of our control. These include having a family history of coronary heart disease at a young age, getting older and being male.
Other factors that increase your risk of coronary heart disease include:
- smoking
- having high cholesterol
- have diabetes
- having high blood pressure(hypertension)
- being inactive
- being overweight or obese
Having some of these risk factors together is sometimes called metabolic syndrome. These include diabetes, high cholesterol, high blood pressure and obesity.
Many of these risk factors, such as your weight and whether you smoke, are things you can control. It’s important to take measures to reduce your risk where you can. This is especially important if you have other risk factors that are out of your control, such as family history. See our section on the prevention of heart attack to find out more.
Symptoms of a heart attack
The symptoms of a heart attack can vary from person to person. They can come on suddenly in some people, without any warning. But in others, symptoms can come on slowly, over days. It isn’t always obvious that you’re having a heart attack.
Heart attack symptoms include:
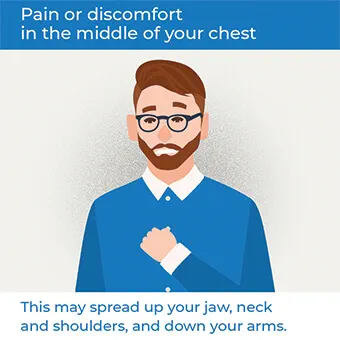
- pain or a sensation of heaviness, pressure, tightness, aching or burning in the middle of your chest
- pain or discomfort spreading up to your jaw, neck and shoulders, and then down to your arms (usually your left arm)
- pain or discomfort in your abdomen, like indigestion
- feeling breathless
- feeling sweaty, light-headed or dizzy
- feeling sick or vomiting
- palpitations (feeling your heart beating)
- feeling anxious
Heart attack symptoms in women and heart attack symptoms in men are the same. But women may be more likely to get less typical symptoms, such as indigestion, feeling sick and vomiting. Older people and people with diabetes are more likely to have these symptoms too.

What to do if someone is having a heart attack
Heart attack symptoms can be similar to those of other conditions. Gastro-oesophageal reflux disease (GORD) can cause a burning pain or discomfort in your chest. Your symptoms may also be due to other heart or lung conditions, panic attacks or muscle pain in your chest.
If you’re having heart attack symptoms like chest pain and you’re unsure what’s causing it, it’s always better to get it checked out. If it is a heart attack, certain treatments work much better if you have them quickly (within two hours). So, it’s important to seek help as soon as possible.
If you think you or someone you’re with might be having a heart attack, call 999 for emergency medical help immediately. While waiting for an ambulance, the affected person should:
- sit and rest in a comfortable position
- chew a single 300mg aspirin tablet, if there is one available and they’re not allergic
When you call 999, the call handler should advise you how long the ambulance will take. You may want to consider whether it will be quicker to make your own way to the hospital. You should only do this if you have someone who can take you. Never drive yourself if you think you may be having a heart attack. The 999 call handler can advise you about this.
Diagnosis of a heart attack
You will usually have an ECG (electrocardiogram) if you have signs of a heart attack. This will happen whenever you first see a doctor or health professional. It might be at a GP surgery, in an ambulance or at hospital. An ECG checks the electrical activity of your heart. It can often show whether or not you’re having a heart attack. If the ECG confirms a heart attack, you will start treatment straight away, before waiting for the results of any other tests.
Your doctor may recommend other tests, either immediately or over the next few days in hospital. These include the following.
- Blood tests, including tests for a protein called troponin. Your heart produces troponin when your heart muscle is damaged. Levels in your blood increase within hours of a heart attack and then fall again.
- A chest X-ray. This will help your doctor see whether there might be a cause for your chest pain other than a heart attack. It also checks for fluid in your lungs, which might happen if your heart isn’t working well after a heart attack.
- A coronary angiogram. This is a type of X-ray that uses a special dye to show up your coronary arteries. It can show where there are blockages or narrowings in your coronary arteries.
- An echocardiogram. This uses ultrasound (sound waves) to check the structure and function of your heart.
Types of heart attack
Doctors will use the results from your ECG to work out exactly what type of heart attack you’ve had. It may be an ST-elevation myocardial infarction (STEMI) or a non-ST-elevation myocardial infarction (NSTEMI). The two types get their names from how they look on the ECG.
- An ST-elevation myocardial infarction (STEMI) is caused by a complete blockage of your coronary artery. It’s often the more serious of the two types.
- An NSTEMI is when you have a partial blockage of a coronary artery. It’s not always as serious as a STEMI.
STEMI and NSTEMI heart attacks have the same symptoms. But the treatment you receive may be different.
Treatment of a heart attack
Initial treatment
How you are treated in hospital will depend on the type of heart attack you’ve had. It will also depend on how long it is since your symptoms started.
If you have a STEMI heart attack (the most serious type), your doctor may recommend treatment to unblock your coronary arteries. There are two main ways to do this.
- A coronary angioplasty. This is also known as a primary percutaneous coronary intervention (PCI). It involves passing a catheter (a long thin tube) into your coronary artery. Your doctor then inflates a tiny balloon at the end, to widen or unblock the artery. They’ll also usually insert a wire mesh tube called a stent to hold your coronary artery open. This is usually the best treatment to have for STEMI, if it’s available quickly.
- Thrombolysis or fibrinolysis. This is an injection of medicines that break down the clot in your coronary artery. The medicine is given through an injection into a vein in your arm. You may have this if a coronary angioplasty isn’t available quickly.
You may also have other medicines to help stop your blood clotting.
If you have an NSTEMI heart attack, you’re more likely to just have treatment with medicines. You may have a coronary angioplasty later on if your doctor thinks you could be at risk of another heart attack.
Long-term treatment
Your doctor will prescribe you medicines to reduce your risk of another heart attack. You’ll usually start taking these in hospital and will need to continue taking them long-term. These may include:
- antiplatelet medicines, which help prevent more clots forming
- statins to help keep your cholesterol low, which can clog up your arteries
- angiotensin-converting enzyme (ACE) inhibitors to improve blood flow to your heart muscle
- beta-blockers, which slow down your heart rate, reducing strain on your heart
Your doctor or pharmacist will explain how to take your medicines. If you need any more information, you can read the patient information leaflet in the box.
Sometimes you may need surgery once you’ve recovered from a heart attack. This might include angioplasty or a coronary artery bypass graft (CABG). CABG is an operation to divert blood around your narrowed or blocked coronary artery. Your surgeon uses a blood vessel from your chest, leg or arm to do this. You might have a CABG if you had an angioplasty first and it didn’t work, or if you couldn’t have an angioplasty.
Recovering from a heart attack
You’ll usually stay in hospital for between two and five days after a heart attack. Before you go home, your doctor will talk to you about measures to reduce your risk of having another heart attack. These include taking the medicines you’re prescribed and making some lifestyle changes. See the prevention section for more information.
Your doctor will also refer you for cardiac rehabilitation. Cardiac rehabilitation programmes help you to get back to as full a life as possible after your heart attack. They can reduce your risk of having another heart attack or needing further treatment. The sessions normally last around 10 to 12 weeks. They include:
- an exercise component with a range of different activities
- education and information sessions about your condition
- support with things like giving up smoking, stress management and healthy eating
Cardiac rehabilitation may start while you’re still in hospital. You should be invited to a session soon after you’re discharged.
Complications of a heart attack
Many people these days survive a heart attack and go on to make a good recovery. But if a heart attack isn’t treated promptly, some of the heart muscle can start to die. This causes serious problems that can be life-threatening.
Complications may include the following
- Arrhythmia (abnormal heart rhythms). Your heart may beat too fast, or too slowly, or the rhythm may become irregular. Arrhythmias can be life-threatening.
- Ongoing Angina, pain or discomfort in your chest. This may be a particular problem when you’re active or exercising.
- Having another heart attack. This may be due to another plaque splitting and causing a blood clot.
- Heart failure. A heart attack can damage your heart muscle and make it weaker. This makes it more difficult to pump blood and oxygen around your body.
- Depression or feeling low. Many people feel depressed after having a heart attack. Seek help from your doctor if you need it.
Treatments are available to help manage all of these complications.
After treatment of a heart attack
Once you’ve recovered from a heart attack, your doctor will recommend a range of measures to try to reduce your risk of having another one. These may include medicines, lifestyle changes and taking part in a cardiac rehabilitation programme. See Prevention section below for more information on lifestyle changes you can make.
Medicines
Your doctor will prescribe you medicines to start taking in hospital. You’ll usually need to continue taking these long term. These may include:
- antiplatelet medicines (usually aspirin with another antiplatelet medicine), which help prevent clots forming
- statins to help keep your cholesterol low, which can clog up your arteries
- angiotensin-converting enzyme (ACE) inhibitors to improve blood flow to your heart muscle
- beta-blockers, which slow down your heart rate, reducing the work it has to do
Always make sure you’ve spoken to your doctor or pharmacist about how to take your medicines, and read the patient information leaflet if you need any more information.
Cardiac rehabilitation
Cardiac rehabilitation programmes aim to help you recover from your heart attack and get back to as full a life as possible afterwards. The programmes can reduce your risk of dying after a heart attack so it’s an important part of your treatment.
Cardiac rehabilitation programmes include an exercise component with a range of different activities, which will be tailored to you. They may also include education and information sessions about your condition and support with things like giving up smoking, stress management and changing your diet. Cardiac rehabilitation may start while you’re still in hospital, and you should be invited to a session soon after you’re discharged.
Heart attack prevention
You can reduce your risk of coronary heart disease and heart attack by making some changes to your lifestyle. These include the following.
- If you smoke, giving up. Your GP or pharmacist can offer support with this.
- Losing excess weight if you’re overweight or obese.
- Doing regular physical activity. Try to build up to at least 150 minutes of moderate-intensity exercise over a week, or 75 minutes of vigorous activity. If you’ve had a heart attack, speak to your doctor about what level of exercise is appropriate for you.
- Eating a healthy, balanced diet This includes cutting down on saturated fat and salt, and having at least five portions of fruit and vegetables a day. Aim to have two portions of fish (one oily) a week too.
- Cutting down on alcohol. Guidelines recommend not to drink more than 14 units of alcohol a week on a regular basis.
- Taking any medication you’re prescribed to control high blood pressure, high cholesterol and diabetes.
If you’ve previously had a heart attack, these measures can reduce your risk of having another one. Your doctor will also prescribe medicines to reduce your risk of further heart attacks. It’s important that you take these as prescribed. If you have a family history of heart disease, your GP may be able to arrange for you to have a health check. This is to assess your risk of a heart attack.
Worried about your heart health?
Get a picture of your current health and potential future health risks with one of our health assessments.
To book or to make an enquiry, call us on 0333 920 7695∧
Heart attack symptoms are the same in men and women. But women may be more likely to have less typical symptoms too, such as indigestion, feeling sick and vomiting. You might not realise these are heart attack symptoms.
If you think you may be having a heart attack, call 999 for emergency medical attention. See our symptoms section for more information.
Chest pain and other symptoms, such as breathlessness and feeling dizzy aren’t always symptoms of a heart attack. They can also be symptoms of other things, such as panic attacks or gastro-oesophageal reflux disease (GORD). But, there’s no way to know for sure so don’t delay seeking help. To find out more, see our section on what to do if someone is having a heart attack.
The most common heart attack symptom is pain or discomfort in your chest. It can feel heavy, or like an aching or burning. This can spread to your jaw, neck, shoulders and arms. You may also feel short of breath, sweaty, dizzy, and sick. Find out more in our symptoms section.
Call 999 for an ambulance straight away if you think someone is having a heart attack. While you’re waiting, help them to get comfortable and rest. If there is an aspirin tablet available, they should chew this. See our what to do section for more information.
Angiogram
An angiogram is a test to find out more about your heart. It can show whether your heart is pumping properly.
Coronary angioplasty
A coronary angioplasty is a procedure to open up narrowed or blocked arteries that can be caused by coronary heart disease.
Coronary heart disease
Seven tips for a healthy and well-balanced diet
A healthy, well-balanced diet involves eating foods from a variety of food groups to get the nutrients that your body needs to function.
Tools and calculators
BMI calculator
BMI, or body mass index, is one way of measuring whether you’re a healthy weight for your height.
Simply enter your details into our calculator and the result will give you an indication of whether you're a healthy weight.
Calories calculator
If you want to lose weight, you need to increase your physical activity and watch your calorie intake. Bupa's calorie calculator will help you to work out how many calories you're burning in a day.
Other helpful websites
Discover other helpful health information websites.
Did our Heart attack information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Acute myocardial infarction. Patient. patient.info, last edited 15 December 2020
- ST-elevation myocardial infarction. BMJ Best Practice. bestpractice.bmj.com, last reviewed 4 October 2022
- Overview of coronary artery disease. MSD Manual. www.msdmanuals.com, last full review/revision June 2022
- Metabolic syndrome. Patient. patient.info, last edited 12 July 2022
- Heart attack symptoms. British Heart Foundation. www.bhf.org.uk, accessed 7 November 2022
- Women and heart attacks. British Heart Foundation. www.bhf.org.uk, accessed 7 November 2022
- Acute coronary syndromes. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 18 November 2020
- Heart attack. British Heart Foundation. www.bhf.org.uk, last reviewed October 2019
- Personal communication, Dr Tim Cripps, Consultant Cardiologist, 16 November 2022
- ECG. British Heart Foundation. www.bhf.org.uk, accessed 7 November 2022
- Ahmed I, Hajouli S. Left heart cardiac catheterization. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 1 July 2022
- Acute myocardial infarction (MI). MSD Manual. www.msdmanuals.com, last full review/revision June 2022
- Non-ST-elevation myocardial infarction. BMJ BestPractice. bestpractice.bmj.com, last reviewed 7 October 2022
- Ahmad M, Mehta P, Reddivari AKR, et al. Percutaneous coronary intervention. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 30 September 2022
- Acute myocardial infarction management. Patient. patient.info, last edited 21 December 2020
- Bachar BJ, Manna B. Coronary artery bypass graft. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 8 August 2022
- Cardiac rehabilitation. British Heart Foundation. www.bhf.org.uk, accessed 7 November 2022
- Complications of acute myocardial infarction. Patient. patient.info, last edited 21 December 2020
- Physical activity guidelines: UK Chief Medical Officers' report. gov.uk, published 7 September 2019
- The Eatwell Guide. Public Health England. gov.uk, published September 2018
- UK Chief Medical Officers’ low risk drinking guidelines. Department of Health. gov.uk, published August 2016

