Cervical screening (Smear test)
Your health experts: Dr Karin Hellner, Consultant in Gynaecology and Lead Colposcopist and Dr Sarah White, Associate Clinical Director at Bupa
Content editor review by Rachael Mayfield-Blake,May 2022
Next review due May 2025
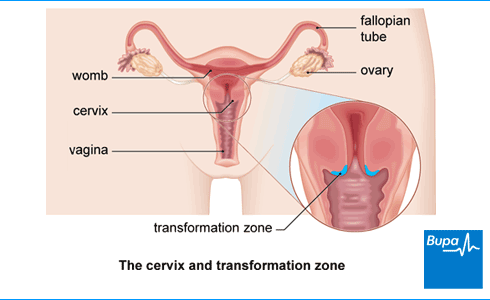
Cervical screening checks your cervix, which is the neck of your womb, to see if it’s healthy. The test involves collecting a sample of cells, which are tested for an infection with a virus called the human papilloma virus (HPV). If you have HPV, the sample will be tested for any changes in your cells. These changes could develop into cervical cancer.
About cervical screening
Cervical screening is commonly known as a smear test. This is because of the way the test used to be done. Cells were smeared on a glass slide, which was sent to a lab to be tested. You might also have heard the term Pap smear, which is what people call it in the USA and in many European countries.
Screening means testing for early signs of an illness before you have symptoms. Cervical screening works really well to prevent cervical cancer – it saves thousands of lives every year. So it’s important to attend regular screening when you’re invited.
In cervical screening (a smear test), a nurse or doctor will take a sample of your cells and test this for high-risk types of the human papillomavirus (HPV). HPV infection is the main cause of cervical cancer. HPV infections are really common and most people get HPV at some point in their lives. Usually, your body will get rid of the infection and you won't know that you have the virus.
If you don’t have HPV, you’re very unlikely to have abnormal cells or to develop cervical cancer. This means the cells in the sample won’t be examined further.
If you’re found to have HPV, your cell sample will be checked for any abnormal changes that could potentially develop into cancer in the future.
Any abnormal cells can be either monitored or treated to stop cancer developing.
NHS cervical screening programme
The NHS runs a national cervical screening programme in the UK for all women aged 25 to 64. If you have a cervix and are registered as female, your GP surgery will invite you for cervical screening. If you’re a trans man (with a cervix), you can also have screening. But if you’re registered as a man with your GP, you won’t be invited automatically. You can ask your GP or a local sexual health or family planning clinic to add you to the cervical screening list.
If you’re aged between 25 and 64 and registered with a GP, you’ll be invited for screening every three or five years. This will depend on your age and where you live. Check what’s available to you.
You don’t have to have the test at a GP surgery. You can also have one at a family planning or sexual health clinic or at a private clinic.
At the moment, doctors don’t think it’s helpful to screen women under 25. Cervical screening doesn’t work as well in women aged 20 to 24 compared to women over this age. It’s common to have changes in the cells of your cervix when you’re younger and most of these go away by themselves. Treating these changes unnecessarily could lead to issues later on.
If you’re 65 or over, you’re very unlikely to develop cervical cancer if your last screening results were normal. But if you’ve never had cervical screening, you’re entitled to a test.
Cancer awareness: cervical cancer
Cervical cancer awareness| Screening | Watch in 1:20 minutes
This animation explains the importance of attending cervial cancer screening so that if you have cervical cancer it can be detected early.
Who needs to have cervical screening?
If you have a cervix and have had any type of sexual contact with men or women (including touching or using sex toys), you should have cervical screening. Screening will pick up human papilloma virus (HPV) infection, which causes the cell changes that could lead to cervical cancer. Even if you haven’t had sex for years, you should still attend screening because you may have come into contact with HPV from a previous partner, months or even years ago. The virus can be inactive and cause abnormal cells later on.
If you’ve had the HPV vaccine, it’s still best to go for your screening appointments. The HPV vaccine protects against the two types of HPV that cause most cases of cervical cancer. But it doesn't protect against other types of HPV that are linked with cervical cancer.
If you’ve never had any sexual contact, your risk of HPV is small but you may decide to still have regular screening. And if you have any unusual bleeding or discharge, see your GP.
If you’ve had a hysterectomy, you won’t need screening unless your cervix wasn’t removed. Ask your GP for more information.
At any age, if you get symptoms such as bleeding after sex or have an unusual discharge, see a GP. You should also see your GP if you get bleeding after menopause. Your doctor might do a cervical screening test as part of their investigations.
Cervical screening and pregnancy
If you're pregnant and have previously had normal screening tests, you can delay routine screening until three months after your baby is born. But check with your doctor or midwife.
If you’ve had an abnormal test before you became pregnant, you may need to have a colposcopy. A colposcopy is a test that uses a magnifying instrument called a colposcope to examine your cervix. Ask your doctor or midwife what’s best for you.
Considerations for a cervical screening test
Screening is the best way to find out if you have HPV, which is the single biggest risk for developing cervical cancer. Screening can pick up changes in the cells of your cervix that could lead to cervical cancer in the future. Detecting these early can help you to get treatment and can be life-saving.
It’s possible some abnormal cells could be missed, so it’s important to go for regular smear tests. This means any abnormal cells can be picked up next time. And very occasionally, screening can show you have abnormal cells when you don’t actually have them. This is rare, but may happen sometimes because no test is perfect.
It's your choice whether or not to have a cervical screening test if you’re offered one. If you’re unsure, talk it over with a nurse at your GP practice.
Preparing for a cervical screening test
It’s best to have your cervical screening test when you’re not on your period. If you’re bleeding, the sample probably won’t be clear and you may need to have the test again.
For two days before your test, don’t use any spermicide (including condoms coated with spermicide), lubricating jelly or vaginal creams. This is because chemicals in these products can affect the test.
What happens during a cervical screening test?
When you go for your cervical screening test (smear test), your appointment will usually last about 10 minutes. But the actual test only takes a minute or two. Usually, a female nurse or doctor will do your test, but if you want to make sure, ask when you make your appointment.
Your nurse or doctor will ask you to take off your clothes (just your bottom half) but if you’re wearing a skirt you can just take your underwear off. They’ll then ask you to lie on your back on an examination couch with your knees bent and apart. If you can’t manage this easily, tell your nurse – you may be able to lie on your side instead.
Your nurse or doctor will use an instrument called a speculum (pronounced speck-you-lum) to gently open your vagina, so they can see your cervix (neck of your womb). They’ll then use a small, soft brush to take a sample of cells from your cervix. They’ll send this sample to a lab to be tested.
Some people find the test uncomfortable but it doesn’t usually hurt. If it does hurt, let your nurse know so they can try and make you more comfortable. Try to relax – the more relaxed you are, the less discomfort you’ll feel. You might find it helps to take some deep breaths, listen to music or watch something on your phone.
What to expect afterwards
You can usually carry on as normal straight away after your screening test. You might bleed a bit afterwards so you may want to use a sanitary pad. Your cervix is a sensitive area so even though a soft brush is used to take the sample, it can bleed even if it’s touched lightly. If you have heavy bleeding or pain, see your GP.
How healthy are you?
With our health assessments you get an action plan that’s tailor-made for you.
To book or to make an enquiry, call us on 0370 218 8122∧
Getting your results
Your nurse or doctor will let you know when you can expect your cervical screening results. They’re usually sent to the surgery or clinic where you had the screening test, as well as to your home address. Your results should be ready within four weeks, but sometimes it can take longer. If you get an abnormal result, it doesn’t mean you have cancer.
Your result will fall into one of the following categories.
You don’t have HPV
If you don’t have HPV, you’re extremely unlikely to have abnormal cells or to develop cervical cancer. This means the cells from your sample won’t be examined further. You’ll be invited back for screening in three or five years’ time, depending on your age and where you live.
You have HPV but no abnormal cells
If your screening test shows you have HPV but normal cervical cells, you’ll be asked to have another test (usually a year later but your results letter will say when). This is to see if the infection has gone. Your HPV will usually clear up with the help of your immune system. If the infection hasn’t gone, your risk of developing abnormal cervical cells increases. So, you’ll be called back again in another year’s time to repeat the test again. If cervical screening shows that you have HPV but no abnormal cells three times in a row, your doctor will refer you to have a colposcopy for more tests.
You have HPV and borderline or mild changes
If your test result says that you have cells with ‘borderline’ or ‘mild’ changes, you’ll have more tests. Although these mild changes rarely develop into cancer and may well return to normal by themselves, they need to be checked. You’ll be offered a further test called a colposcopy to look at your cervix more closely. This is usually within six weeks.
You have HPV and moderate or severe changes
If your test result says that you have cells with ‘moderate’ or ‘severe’ changes, it still means you don’t have cancer. But cells with these changes are less likely to return to normal on their own so you may need treatment. You’ll be offered a colposcopy to examine your cervix, usually within two weeks, to see if you do need treatment.
An inadequate result
Sometimes the result may be 'inadequate' or 'unsatisfactory' because there weren’t enough cells in the sample or the cells couldn’t be seen clearly. If this happens, you’ll be asked to have another test after three months.
It may worry you if you have high-risk HPV and/or abnormal cells. If you’re concerned about your results or don’t understand the wording in your results letter, arrange to speak to your GP who can explain them.
Treatment of abnormal cervical cells
If your screening test shows abnormal cells, you’ll be asked to have a more detailed test called a colposcopy. If your colposcopy shows an area of your cervix that looks abnormal, the doctor will take a biopsy. This is a small sample of the abnormal tissue that is sent to a lab to be examined.
Depending on the result, you may need to have treatment to either remove or destroy the abnormal cells. The usual way to do this is with a large-loop excision, also known as loop excision or loop diathermy. In this procedure, your doctor uses a wire loop with an electric current to remove the abnormal cells from your cervix.
You’ll usually have this treatment under local anaesthesia so you’ll be awake but won’t feel any pain. General anaesthesia (where you are asleep) may also be an option under some circumstances – ask your nurse or doctor for advice.
Other treatments that can destroy abnormal cells include:
- laser therapy
- cryotherapy (freezing)
- cold coagulation (which actually uses heat to destroy the cells)
Ask your nurse or doctor for more information about these.
Cervical screening (smear test) tests a sample of cells from your cervix for an infection with a virus called the human papilloma virus (HPV). If you have a certain high-risk type of HPV, you’ll then be tested for any changes in the cells. These changes could later develop into cervical cancer.
For more information, see our section: About cervical screening above.
If you’re aged between 25 and 64 and registered with a GP, you’ll be invited for screening every three or five years. It depends on your age and where you live in the UK because the different UK nations have slightly different screening programmes. Check what’s available to you. You might get invited earlier if your previous smear showed HPV or abnormal cells.
For more information, see our section: NHS cervical screening programme above.
Age limits are based on the latest evidence. In people under 25, cervical cancer is very rare, and screening doesn’t reduce cervical cancer rates but might increase side-effects from treatment . People over 64 who have had regular screening are highly unlikely to develop cervical cancer beyond this age.
For more information, see our section: NHS cervical screening programme above.
Cervical cancer
Colposcopy
Did our Cervical screening (Smear test) information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Cervical screening: helping you decide. Public Health England. www.gov.uk, updated 31 October 2021
- Guidance. NHS population screening explained. Public Health England. www.gov.uk, last updated 17 March 2021
- Cervical screening. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised December 2021
- The Pap (Papanicolaou) test. American Cancer Society. www.cancer.org, last revised 3 January 2020
- Chrysostomou AC, Stylianou DC, Constantinidou A, et al. Cervical cancer screening programs in Europe: the transition towards HPV vaccination and population-based HPV testing. Viruses 2018; 10(12):729. doi: 10.3390/v10120729
- Cervical cancer. BMJ Best Practice. bestpractice.bmj.com, last reviewed 18 February 2022
- Abnormal pap smear. BMJ Best Practice. bestpractice.bmj.com, last reviewed 18 February 2022
- What is cervical cancer? Cancer Research UK. www.cancerresearchuk.org, last reviewed 27 January 2020
- Guide to sexual health services. NHS. www.nhs.uk, last reviewed 21 November 2018
- NHS population screening: information for trans and non-binary people. Public Health England. www.gov.uk, updated 20 October 2021
- About cervical screening. Cancer Research UK. www.cancerresearchuk.org, last reviewed 18 January 2022
- Adult screening programme. Cervical cancer. UK National Screening Committee. www.gov.uk, accessed 18 March 2022
- Cervical screening aged 65 or over. Jo's Cervical Cancer Trust. www.jostrust.org.uk, last updated 23 October 2018
- Cervical screening: having a colposcopy. Public Health England. www.gov.uk, updated 31 October 2021
- What happens at cervical screening? Jo's Cervical Cancer Trust. www.jostrust.org.uk, last updated 14 June 2020
- Cervical screening results. Jo's Cervical Cancer Trust. www.jostrust.org.uk, last updated 12 June 2020
- HPV and cervical cancer. Jo's Cervical Cancer Trust. www.jostrust.org.uk, last updated 17 August 2018
- Cervical screening. Patient. patient.info, last edited 24 May 2021
- Management and referral guidelines for colposcopy. Public Health England. www.gov.uk, updated 28 September 2021
- About cervical cell changes. Jo's Cervical Cancer Trust. www.jostrust.org.uk, last updated 14 January 2022
- Treatment if you have abnormal cervical cells. Cancer Research UK. www.cancerresearchuk.org, last reviewed 5 March 2020
- Cervical screening: programme and colposcopy management. Colposcopic diagnosis, treatment and follow up. Public Health England. www.gov.uk, last updated 28 September 2021
- Introduction and programme policy. Public Health England. www.gov.uk, last updated 28 September 2021
- About cervical screening. Jo's Cervical Cancer Trust. www.jostrust.org.uk, last updated 9 September 2020
- Cervical screening aged 24 or under. Jo's Cervical Cancer Trust. www.jostrust.org.uk, last updated 15 October 2019
- Personal communication, Dr Karin Hellner, Consultant in Obstetrics and Gynaecology, 27 April 2022
- Guidance. Cervical screening: programme overview. Public Health England. www.gov.uk, last updated 17 March 2021
- What happens at cervical screening? Jo's Cervical Cancer Trust. www.jostrust.org.uk, last updated 14 June 2020
- Guidance. HPV vaccination: guidance for healthcare practitioners. Public Health England. www.gov.uk, last updated 17 March 2022

