Breast cancer
- Mr Harun Thomas, Consultant Oncoplastic Breast Surgeon
Breast cancer is cancer that starts in your breast. It may cause a lump in your breast or change how your breast or nipples look or feel. Treatments for breast cancer may include surgery, radiotherapy, chemotherapy and specific targeted therapy.
About breast cancer
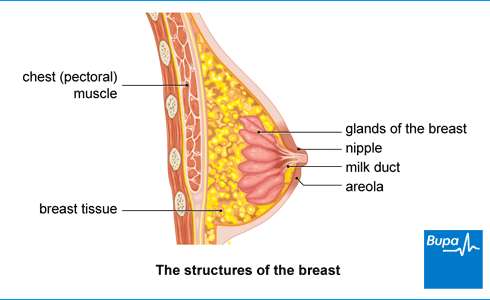
Breast cancer happens when cells in your breast tissue grow abnormally and out of control. Everyone has breast tissue. Breasts are made up of:
- fat
- connective tissue
- glandular tissue
The glandular tissue is divided into small parts called lobules. The lobules are connected to your nipple by milk ducts. Breast cancer may start in the lobules or milk ducts – see our Types of breast cancer section.
Each year in the UK, 55,000 women are diagnosed with breast cancer. Around 400 men are also diagnosed with breast cancer each year. The risk of breast cancer in transgender people isn’t yet fully understood.
How cancer develops
Cancer explained | Watch in 1:48 minutes
In this video, we explain how, when cells divide uncontrollably, this leads to cancer.
Types of breast cancer
There are several different types of breast cancer, depending on where the cancer starts. Breast cancer can start in the:
- lining of your milk ducts (ductal breast cancer)
- lobules of your breast (lobular breast cancer)
Breast cancer can also be:
- non-invasive – staying in the ducts or lobules (carcinoma in situ)
- invasive – spreading outside the ducts or lobules
The three most common breast cancer types are:
- invasive ductal breast cancer – this is also called invasive breast cancer (no special type, NST)
- invasive lobular carcinoma (ILC)
- ductal carcinoma in situ (DCIS) – in some people, this can become invasive cancer if it isn’t treated
If cancer cells spread to other parts of your body (other than your armpit lymph nodes), this is called metastatic cancer or secondary cancer.
Breast cancer can also be grouped by how sensitive it is to different hormones and chemical substances in your body.
- Oestrogen receptor-positive breast cancer means the cancer is sensitive to the hormone oestrogen.
- HER2-positive breast cancer means the cancer is sensitive to a protein called HER2.
- Triple negative breast cancer isn’t sensitive to oestrogen, progesterone or HER2.
Causes of breast cancer
We don’t know for sure why some people get breast cancer. But breast cancer causes are likely to be a combination of genetic, hormonal and lifestyle factors.
You’re more likely to develop breast cancer if you:
- are over 50
- have a parent or sister who’s had breast cancer or ovarian cancer
- have certain genes that are linked to an increased family history of breast cancer, such as BRCA1 and BRCA2
- started your periods early or the menopause late
- have never had children or didn't have children until after age 30
- take a contraceptive pill that contains oestrogen
- take hormone replacement therapy (HRT), depending on the type of HRT and how long you take it
- are overweight once you've passed the menopause
- drink alcohol – the more you drink, the greater your risk
The risk of breast cancer in transgender people isn’t yet fully understood. We know that HRT increases the risk of breast cancer in post-menopausal women. But doctors don’t know if trans women taking hormone therapy will experience the same increase in risk, so more research is needed.
More research is needed to see if trans men who take hormone treatment may have a reduced risk of developing breast cancer. If you’ve had a mastectomy (removal of both breasts) as part of gender affirming surgery, your risk of getting breast cancer is reduced by around 95 percent.
Symptoms of breast cancer
Most people with breast cancer notice a lump in their breast. But breast cancer doesn’t always cause symptoms at first. You may not get any pain or discomfort. Some people are diagnosed with breast cancer during a routine mammogram.
It’s important to be familiar with how your breasts normally look and feel. This may help you notice any early signs of breast cancer. Your breasts may change at different times of the month. If you notice a change that isn’t normal for you, contact your GP. The pictures below show you what to look out for.
These are the most common breast cancer symptoms.
- A lump or thickening in your breast that feels different from the rest of your breast tissue.
- Discharge or bleeding from your nipple. The discharge is new and isn’t milky..
- A change in the look or texture of your skin. Your skin may be red, puckered or look dimpled like the skin of an orange.
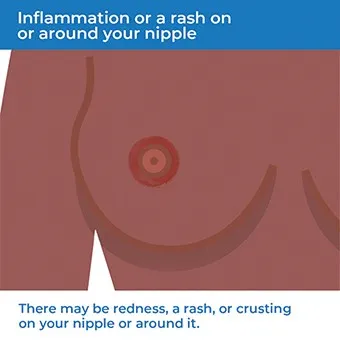
- Inflammation, a rash, redness or crusting on or around your nipple.
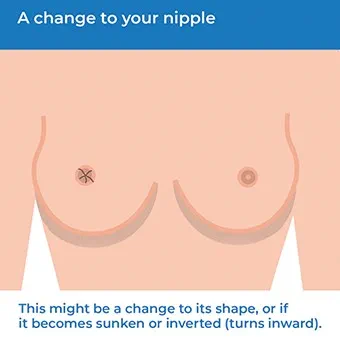
- A change to your nipple’s shape. Or it may become sunken or inverted (turns inward).
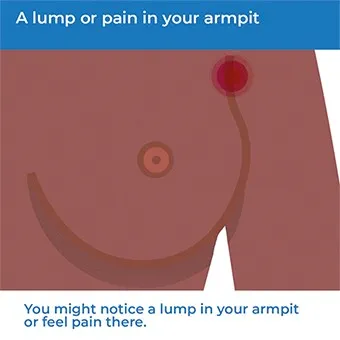
- A lump or pain in your armpit.
- A change in the size or shape of your breast, especially noticeable when you move your arms.

Having these symptoms doesn’t necessarily mean you have breast cancer. Breast lumps are often benign (non-cancerous) and there are many causes of breast changes. But it’s always important to get any changes checked out.
How to check your breasts
Check breasts for cancer signs | Watch in 1:45 minutes
Checking your breasts regularly helps you know what’s normal for you and spot any changes. Our animation shows you how to do it and what to look for.
How to check your breasts
Checking your breasts regularly helps you know what’s normal for you. Choose a time and place to check your breasts when it suits you.
- Begin by looking at your breasts in the mirror.
- Keep your shoulders straight and put your hands on your hips.
- Look at each breast and nipple to check for any changes in size or shape. This includes whether your nipple has sunken or become inverted (turns inwards), or if there is any fluid (discharge) coming from one or both nipples.
- Check your skin for any redness, rashes, dimpling or puckering.
- Now, raise your arms and look for the same changes.
- Next, feel for any lumps or painful areas. Use the flat part of your fingers to gently work around each breast, pressing in small, circular motions. Vary your pressure to check the tissue just under your skin, but also deeper tissue too.
- Be sure to check the whole of your breast area. This includes under your armpits, all around each breast and up to your collarbone. Do this step laying down, perhaps in bed, and then standing up, maybe while taking a shower.
Your breasts might feel different at different times during the month, so getting to know what’s normal for you is key.
Always contact your GP if you notice any unusual changes.
Diagnosis of breast cancer
Seeing your GP
Your GP will ask you about any symptoms and your medical and family history. They’ll also check both of your breasts for lumps and other signs, such as changes to your skin or nipples.
If your GP thinks you need further assessment, they'll refer you to a specialist breast clinic. How quickly you'll be seen will depend on your symptoms and your age.
You may also be asked to go to a breast clinic after having a screening mammogram. This doesn’t necessarily mean that a cancer has been seen. Most people who are recalled following screening don’t have breast cancer.
Triple assessment
At the specialist breast clinic, you’ll be offered triple assessment. This includes:
- an examination of your breasts by the doctor
- a scan (if needed) – this may be a mammogram (X-ray of your breasts) or an ultrasound or both
- a biopsy – if the examination or scan has found something that may not be normal
You may also have an ultrasound scan of your armpit. This looks for cancer that may have spread from your breast to the lymph nodes in your armpit.
You should be able to have all these tests, including the biopsy, during a single clinic visit. If you have a biopsy, you’ll have a follow-up appointment to discuss the results. The results can help your doctor decide if you need any more investigations or treatment.
Further tests
If cancer cells are found, these will be tested further in the laboratory. These tests will show whether or not your breast cancer is sensitive to certain hormones and chemical substances. You may also be offered genetic testing for the BRCA1 and BRCA2 genes.
Your doctor can explain what the results of all the tests mean for you and your treatment.
Worried about breast health?
Book a breast check, which includes a mammogram† and get a picture of your current health with our breast health check.
To book or to make an enquiry, call us on 0345 600 3458∧
However, if you are concerned that you may have a lump, please book an urgent GP appointment for assessment, it may be more appropriate to refer you to a specialist.
Treatment options for breast cancer
If you have breast cancer, you’ll be under the care of a multidisciplinary team of breast cancer specialists. You should also have a specialist nurse to support you.
Your breast cancer treatment will depend on several things. These include the type of breast cancer, if it's spread and if it’s sensitive to certain medicines. Your wishes and preferences will be taken into account.
Surgery
Surgery may be the first treatment offered for breast cancer.
- Breast conserving surgery means you keep your breast. This involves removing the cancer with a healthy rim of normal breast tissue (a wide local excision). Talk to your surgeon about what to expect.
- A mastectomy removes the whole of your affected breast. You should be offered breast reconstruction surgery if it’s right for you. If you decide to have a reconstruction, you may be able to have it at the same time as the mastectomy or wait until later.
Sentinel lymph node biopsy
Your doctor will usually recommend you have a sentinel lymph node biopsy. The sentinel nodes are the first nodes that a cancer may spread to. These can be removed during your breast surgery and checked for cancer cells.
If your sentinel nodes contain cancer cells, your surgeon may recommend you have a further operation to remove more lymph nodes. This is called axillary clearance.
Radiotherapy
Radiotherapy is a treatment to destroy cancer cells with radiation. You’ll usually be offered it after surgery to destroy any remaining cancer cells. This aims to reduce the risk of your cancer coming back.
Medicines
- You may be offered some medicines before or after surgery. Your doctor will talk to you about the benefits and risks of the different medicines. Chemotherapy uses medicines to destroy cancer cells. You may have two or three different chemotherapy medicines as part of your treatment.
- Hormone (endocrine) medicines may be suitable for breast cancer that’s sensitive to oestrogen. Tamoxifen blocks the effects of oestrogen on your cancer. Aromatase inhibitors stop your body from making oestrogen.
- Biological therapy (targeted therapy) targets cancer cells and affects their growth. These medicines include trastuzumab (Herceptin) and pertuzumab (Perjeta). Your doctor will only offer these if your breast cancer is sensitive to the protein HER2.
- Bisphosphonates are medicines that prevent bone thinning. They may be prescribed if your breast cancer has spread and is causing bone pain. Bisphosphonates may also help to stop breast cancer spreading or coming back. You may be offered these medicines if you’ve gone through the menopause.
Treating advanced cancer
If breast cancer has spread to other areas of your body, treatment won’t be able to cure your cancer. But it can reduce your symptoms, help you feel better and may help you to survive your cancer for longer.
Your doctor may offer you treatment with hormone therapy, chemotherapy and biological therapy. You may be offered other treatments as well to ease bone pain, breathlessness and tiredness. Your healthcare team will support you and advise you on the best ways to manage your symptoms.
Prevention of breast cancer
Healthy lifestyle
You can’t change some risk factors for breast cancer, such as getting older or having a family history of breast cancer. But breast cancer may also be linked to some lifestyle factors.
You may help to reduce your risk of breast cancer by:
- losing any excess weight you have, then keeping to a healthy weight
- being active
- stopping smoking
- only drinking alcohol in moderation
Breastfeeding is known to help protect against breast cancer.
Higher risk of breast cancer
You may have a higher risk of getting breast cancer if members of your close family have had breast or ovarian cancer. If you're concerned about your risk, talk to your GP. They may refer you to a breast clinic, family history clinic or specialist genetics clinic.
The healthcare professionals at the clinic will talk to you about your risk and exactly what this means for you. You may be offered a genetic test to see if you carry a gene for breast cancer. You won’t be offered this until you’ve talked it all through with a genetic counsellor first.
Depending on how high your risk of breast cancer is, your doctor will give you advice on how to lower this risk. This may include:
- being especially aware of any changes in your breasts – called breast cancer awareness
- making lifestyle changes, such as losing weight, being active and reducing alcohol
- having breast screening from an earlier age or more frequently than usual
- having yearly MRI scans of your breasts
- taking medicines such as tamoxifen
- considering surgery (mastectomy)
Living with breast cancer
Follow-up after treatment
After your breast cancer treatment, you'll have regular check-ups with the breast care team. At your appointments, your doctor or nurse will ask how you are and may examine you. They’ll ask if you have problems with any ongoing treatment. This is a good time for you to share any problems or concerns you have.
You'll be asked to return for a mammogram every year for five years. If you’re under 50, you’ll have yearly mammograms until you’re called for routine breast screening.
Help and support
Being diagnosed with breast cancer and facing treatment can be distressing for you and your loved ones. An important part of cancer treatment is having support to deal with the emotional aspects and practical issues, as well as the physical symptoms. Specialist cancer doctors and nurses are experts in providing the support you need. Make sure you talk to them if you have any concerns.
Talking to people close to you can help them to understand what you’re going through and how you’re feeling. Organisations and support groups that specialise in breast cancer can also be a great source of information and support. For more information, see our Other helpful websites section.
You may notice changes in your breast that aren’t normal for you. This includes a lump in your breast or armpit, or your breast or nipple looking or feeling different. See our symptoms of breast cancer section for more information.
There are many different types of breast cancer. Breast cancer is named according to the type of cell it starts in and whether or not it has grown into the surrounding tissues. For more information, see our types of breast cancer section.
Lymphoedema is swelling in your arm caused by fluid not draining away properly. This can happen after surgery to remove lymph nodes or radiotherapy on your lymph nodes. Tell your doctor or breast care nurse right away if you notice swelling. They may suggest you have massage, exercise and bandaging.
Chemotherapy
Radiotherapy
Tools and calculators
BMI calculator
BMI, or body mass index, is one way of measuring whether you’re a healthy weight for your height.
Simply enter your details into our calculator and the result will give you an indication of whether you're a healthy weight.
Calories calculator
If you want to lose weight, you need to increase your physical activity and watch your calorie intake. Bupa's calorie calculator will help you to work out how many calories you're burning in a day.
Other helpful websites
Discover other helpful health information websites.
Did our Breast cancer information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Breast cancer. Patient. patient.info, last edited June 2023
- Breast cancer. Medscape. emedicine.medscape.com, updated May 2023
- Breast cancer – recognition and referral. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised August 2020
- Primary invasive breast cancer. BMJ Best practice. bestpractice.bmj.com, last reviewed August 2023
- Breast cancer. Medscape. emedicine.medscape.com, updated May 2023
- Breast cancer facts and statistics. Breast Cancer Now. breastcancernow.org, accessed October 2023
- Metastatic breast cancer. BMJ Best practice. bestpractice.bmj.com, last reviewed August 2023
- Breast cancer in situ. BMJ Best Practice. bestpractice.bmj.com, last reviewed August 2023
- Triple negative breast cancer. Cancer Research UK. about-cancer.cancerresearchuk.org, last reviewed June 2023
- Familial breast cancer: classification, care and managing breast cancer and related risks in people with a family history of breast cancer. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, updated November 2019
- Berliere M, Coche M, Lacroix C, et al. Effects of Hormones on Breast Development and Breast Cancer Risk in Transgender Women. Cancers (Basel) 2022 Dec 30; 15(1):245. doi: 10.3390/cancers15010245. PMID: 36612241; PMCID: PMC9818520.
- Risk-reducing breast surgery. Macmillan Cancer Support. www.macmillan.org.uk, reviewed November 2022
- Breast disease. Oxford Handbook of General Practice. 5th ed. Oxford Academic (online). academic.oup.com, published online June 2020
- Haematology and immunology. Breast awareness. Oxford Handbook of General Practice. 5th ed. Oxford Academic (online). academic.oup.com, published online June 2020
- NHS breast screening: helping you decide. Public Health England. www.gov.uk, last updated October 2021
- Breast surgery. Oxford Handbook of Clinical Surgery. 5th ed. Oxford Academic (online). academic.oup.com, published online November 2021
- Early and locally advanced breast cancer: diagnosis and management. Diagnostic assessment and adjuvant therapy planning. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated June 2023
- Breast cancer lymphoscintigraphy (sentinel lymph node mapping). Medscape. emedicine.medscape.com, updated November 2022
- Breast cancer. NICE British National Formulary. bnf.nice.org.uk, last updated July 2023
- General aspects of chemotherapy. Patient. patient.info, last updated, September 2023
- Tamoxifen. NICE British National Formulary. bnf.nice.org.uk, last updated July 2023
- Adjuvant therapy for breast cancer. Aromatase inhibitors. Medscape. emedicine.medscape.com, updated September 2023
- Adjuvant therapy for breast cancer. Monoclonal antibodies. Medscape. emedicine.medscape.com, updated September 2023
- Zolendronic acid. NICE British National Formulary. bnf.nice.org.uk, last updated July 2023
- Follow-up after breast cancer treatment. Cancer Research UK. about-cancer.cancerresearchuk.org, last reviewed July 2023
- Coping and support when you have breast cancer. Cancer Research UK. about-cancer.cancerresearchuk.org, last reviewed September 2023
- Clarke CN, Cortina CS, Fayanju OM, et al. Breast Cancer Risk and Screening in Transgender Persons: A Call for Inclusive Care. Ann Surg Oncol 2022; 29:2176–80. https://doi.org/10.1245/s10434-021-10217-5
- Personal communication Mr Harun Thomas, Consultant Oncoplastic Breast Surgeon, December 2023
- Victoria Goldman, Freelance Health Editor



