Antihistamines
Your health expert: Madeeha Waheed, Oncology Pharmacist at Bupa, Clinical and Operational Improvement
Content editor review by Dr Kristina Routh, November 2021
Next review due November 2024
Antihistamines are medicines that you usually take to stop the symptoms of an allergic reaction like hay fever. You may also take them for insect bites and stings, or travel sickness.
Uses of antihistamines
Antihistamines help to ease allergy symptoms, such as sneezing, a runny nose, a skin rash or itching. You can buy some antihistamines over the counter from a pharmacy. Some are only available on prescription.
Antihistamines may be helpful for allergic conditions such as:
- hives (urticaria)
- drug allergies
- itchy eczema or dermatitis
- allergic conjunctivitis (sore, itchy eyes)
- allergic asthma
Antihistamines may also help to ease:
- nausea and sickness (including travel sickness)
- vertigo (feeling like everything around you is spinning)
- insect bites and stings
Not everyone can take antihistamines. So talk to a pharmacist or GP if you’re taking these medicines for the first time. And read the patient information leaflet that comes with your medicine carefully.
If you’re pregnant or breastfeeding, it’s important to speak to your GP or pharmacist before taking an antihistamine. They can say whether it’s safe to take. Some antihistamines can affect your baby.
Very young children shouldn’t be given antihistamines without a doctor’s advice.
Anaphylaxis
Antihistamines should not be used for anaphylaxis.
Antihistamines help ease symptoms of allergies. But they aren’t the right treatment for a very bad allergic reaction called anaphylaxis. This can cause:
- difficulty breathing
- difficulty swallowing
- a swollen throat and tongue
- a fast heartbeat and pulse
- feeling faint and dizzy
- you to be sick
Anaphylaxis can be very dangerous. So, get medical help straightaway if you have these symptoms.
How do antihistamines work?
Antihistamines work by blocking the effects of a chemical called histamine. Histamine is made and released by your immune system to help protect you from infections. It makes small blood vessels more ‘leaky’ around an area of damaged tissue. This lets immune cells and fluid go into the damaged area to fight infection and heal the tissues.
If you have an allergy, your immune system reacts to something that isn’t harmful like pollen. Your body then releases too much histamine. This can cause inflammation in your lungs, throat, nose, sinuses, digestive system and skin.
Types of antihistamines
If you have mild-to-moderate allergies, antihistamines bought over the counter may help. These may also help with bites and stings and travel sickness. If your allergy symptoms are very bad, your GP may offer you other antihistamines on prescription.
Antihistamines come in different forms including:
- tablets and capsules
- liquids and syrups
- eye drops
- skin creams
- nasal sprays
There are two main types of antihistamines:
- sedating antihistamines (which may make you feel sleepy)
- non-sedating antihistamines (which don’t usually make you feel sleepy)
Sedating antihistamines
These are the older or ‘first generation’ antihistamines. They can make you feel sleepy, because the medicines move easily from your blood to your brain. This can slow down your thinking and movement and affect your concentration. If you get these effects, do not drive, cycle or operate machinery.
Your doctor may suggest that you take a sedating antihistamine if itching from an allergy is affecting your sleep. Some of these medicines may help with travel sickness and vertigo. Sedating antihistamines that are available from pharmacies for allergies include:
- chlorphenamine maleate (eg Piriton)
- clemastine (eg Tavegil)
- cyproheptadine hydrochloride (eg Periactin)
- promethazine hydrochloride (eg Phenergan)
You may also be able to buy these antihistamines in a generic (unbranded) pack from a pharmacy.
There are some sedating antihistamines for allergies that can only be prescribed by your GP. These include a medicine called alimemazine.
If you have travel sickness or vertigo (dizziness) you can buy the following sedating antihistamines from your pharmacy.
- Cinnarizine (eg Stugeron)
- Promethazine teoclate (eg Avomine)
- Cyclizine
Non-sedating antihistamines
These are the newer ‘second generation’ antihistamines. They’re less likely to make you feel sleepy. But this varies from person to person, so be aware that you might still be affected by drowsiness.
Non-sedating antihistamines that you can buy from a pharmacy include:
- acrivastine (eg Benadryl Allergy Relief)
- cetirizine hydrochloride (eg Piriteze Allergy)
- loratadine (eg Clarityn Allergy)
You can also buy these antihistamines in a generic (unbranded) pack from a pharmacy.
Your GP can also prescribe other non-sedating antihistamines, such as fexofenadine.
Taking antihistamines
You can use antihistamines in different ways, depending on what’s causing your symptoms. For hay fever, you may need to take antihistamines throughout the spring and/or summer. If the allergen can be removed, you may only need to take antihistamines for a short time.
If you’re allergic to something that’s often around, you may need longer treatment. Some people take antihistamines every day, but usually under medical guidance. If you find you’re needing to take antihistamines long term, talk to your GP about this.
How you take your medicine will also depend on the form of antihistamine. So taking an oral antihistamine will be different from using a nasal spray or eyedrops. For information on how to take your medicine, read the patient information leaflet that comes with it. For further advice, speak to your pharmacist.
Interactions of antihistamines
Antihistamines can react with other medicines. Different antihistamines have different interactions. If you’re already taking other medicines, check with your pharmacist or GP before you take an antihistamine. And read the patient information leaflet that comes with your medicine carefully. This will tell you which medicines could cause a problem when taken together.
Side-effects of antihistamines
Like all medicines, antihistamines can cause some side-effects. But they are generally thought to be safe medicines.
Sedating antihistamines may well make you feel sleepy. In fact you may even still feel sleepy the following day. They may also affect your co-ordination, movement and concentration. Some types of sedating antihistamines may affect you more than others. Non-sedating antihistamines may still make you feel sleepy, but this is less likely. If you feel sleepy while taking any antihistamines, don’t drive, cycle or operate machines.
If you use an antihistamine nose spray, you may find it leaves a bitter taste in your mouth. This may be because you’re not using it properly, so speak to your pharmacist.
Children and older people may be more likely to get side-effects with some antihistamines. The patient leaflet that comes with your medicine will tell you about possible side-effects. These may be different for different antihistamines. If you have any questions, ask your pharmacist for advice.
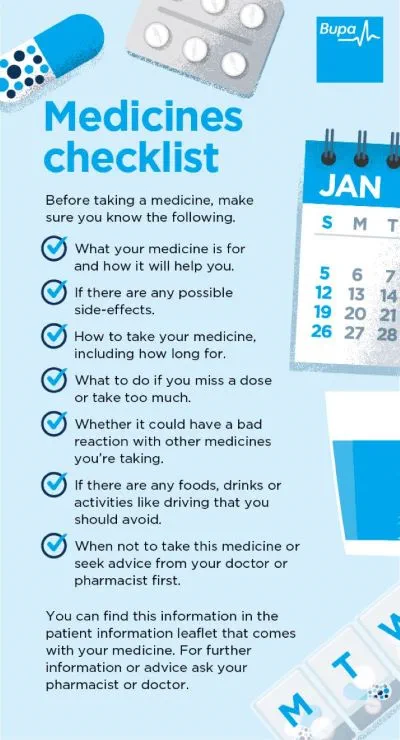
Medicines checklist
Our handy medicines checklist helps you see what to check for before taking a medicine.
Bupa's medicines checklist PDF opens in a new window (0.8MB)
It’s best not to drink alcohol while taking any type of antihistamine. Alcohol can increase the sedative side-effects of antihistamines, so you’re even more likely to feel sleepy.
If you take antihistamines to ease symptoms of an allergy, you’ll need to keep taking them while you have contact with the allergen. So, if you have hay fever, you may need antihistamines every day during the spring and/or summer. Some people do have to take antihistamines every day (for instance some people with asthma). This is usually done under guidance from their doctor. You should seek medical help if you find yourself needing an antihistamine long term (outside of hay fever season).
If you think you’ve taken too much of any antihistamine, you should get medical help straightaway. Take the medicine packet(s) with you, so the doctor can see exactly which type of antihistamine you’ve taken and how many. It’s best to take someone with you just in case you need some support.
You should only take more than one antihistamine at a time if your doctor recommends this.
Be aware that a range of medicines you can buy at a pharmacy may contain antihistamines. This includes medicines for allergies, travel sickness, and coughs and colds. So it’s possible to take more than one antihistamine without realising it. It’s important to ask your pharmacist for advice if you plan on taking more than one of these medicines.
Antihistamines can ease the symptoms of an allergy, but they won’t stop your allergy. So, if you’re allergic to something, you should try to avoid it. If your symptoms are very bad, see your GP because there may be other treatments that work. They may also suggest you see an allergy specialist. You may need to have a ‘skin prick test’ to check exactly what’s triggering your allergic reaction. If so, you’ll need to stop taking antihistamines several days before the test.
How long antihistamines take to work depends on the type you’re taking and what you’re taking them for. Antihistamines come in different forms which will also affect how quickly they work. Antihistamine tablets typically start to work within 30 minutes. They may reach their maximum effect in about two hours. Antihistamine nasal sprays work faster, but only affect your nose.
Did our Antihistamines information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Farzam K, Sabir S, O'Rourke MC. Antihistamines. [Updated 2021 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. ncbi.nlm.nih.gov/books
- Antihistamines, allergen immunotherapy and allergic emergencies. NICE British National Formulary. Bnf.nice.org.uk, accessed November 2021
- Nausea and labyrinth disorders. NICE British National Formulary. Bnf.nice.org.uk, accessed November 2021
- Promethazine hydrochloride. NICE British National Formulary. Bnf.nice.org.uk, accessed November 2021
- Cetirizine hydrochloride. NICE British National Formulary. Bnf.nice.org.uk, accessed November 2021
- Chlorphenamine maleate. NICE British National Formulary. Bnf.nice.org.uk, accessed November 2021
- Clemastine. NICE British National Formulary. Bnf.nice.org.uk, accessed November 2021
- Cyproheptadine hydrochloride. NICE British National Formulary. bnf.nice.org.uk, accessed November 2021
- Promethazine hydrochloride. NICE British National Formulary. Bnf.nice.org.uk, accessed November 2021
- Alimemazine. NICE British National Formulary. Bnf.nice.org.uk, accessed November 2021
- Cyclizine. NICE British National Formulary. Bnf.nice.org.uk, accessed November 2021
- Promethazine teoclate. NICE British National Formulary. Bnf.nice.org.uk, accessed November 2021
- Cinnarizine. NICE British National Formulary. Bnf.nice.org.uk, accessed November 2021
- Acrivastine. NICE British National Formulary. Bnf.nice.org.uk, accessed November 2021
- Loratadine. NICE British National Formulary. Bnf.nice.org.uk, accessed November 2021
- Fexofenadine hydrochloride. NICE British National Formulary. Bnf.nice.org.uk, accessed November 2021
- Interactions. NICE British National Formulary. Bnf.nice.org.uk, accessed November 2021
- Allergic rhinitis. BMJ Best practice. bestpractice.bmj.com, last reviewed October 2021
- Allergic rhinitis. Medscape. www.emedicine.medscape.com, updated August 2021
- Antihistamines. Patient. patient.info/doctor, last edited June 2014
- Overview of allergic and atopic disorders. The MSD Manuals. www.msdmanuals.com, last full review/revision October 2020
- Eczema. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised July 2021
- Angio-oedema and anaphylaxis. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised September 2021
- Allergic rhinitis. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised August 2021
- Conjunctivitis – allergic. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised October 2020
- Insect bites and stings. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised September 2020
- Eczema. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised July 2021
- Urticaria. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised August 2021
- Antihistamines. NHS. www.nhs.uk, last reviewed February 2020
- Phenergan tablets. Electronic Medicines Compendium – eMC. www.medicines.org.uk, last updated March 2021
- Cetirizide hydrochloride tablets. Electronic Medicines Compendium – eMC. www.medicines.org.uk, last updated January 2020
- Personal communication, Madeeha Waheed, Oncology Pharmacist at Bupa, Clinical and Operational Improvement, November 2021