Tonsillitis
Your health expert: Ade Adeniyi, Lead physician, Bupa
Content editor review by Rachael Mayfield-Blake, Freelance Health Editor, July 2023
Next review due July 2026
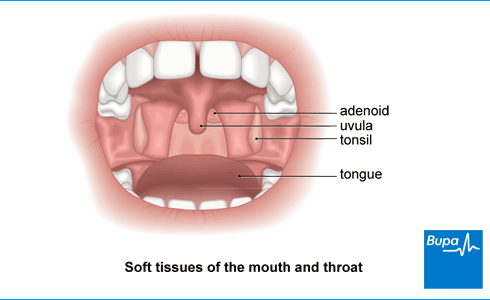
Tonsillitis is when you have swollen (inflamed) tonsils. Your tonsils are two small round lumps of tissue at the back of your throat. Tonsillitis is usually caused by an infection with a virus or bacteria. You may have a sore throat, swollen tonsils and pain when you swallow.
About tonsillitis
Your tonsils are two small round lumps of tissue at the back of your throat. They’re part of your immune system, helping your body to fight infections. Your tonsils tend to get smaller as you get older.
If you have tonsillitis, your tonsils are likely to be red, swollen and sore. Tonsillitis can affect people of all ages, but it’s more common in children and young adults.
Tonsillitis usually improves on its own after about a week. It’s most often caused by a virus, so antibiotics won’t help. Even if it’s a bacterial infection, it will often settle without antibiotics. You can ease your symptoms with self-help measures (see our section on self-help) and over-the-counter medicines.
Causes of tonsillitis
The main cause of tonsillitis is a viral infection. Viral tonsillitis is usually due to a common cold virus, but it may also be caused by other viruses, including the flu virus.
For around one in every three people, tonsillitis is caused by bacteria. Most bacterial tonsillitis is caused by streptococcus bacteria – specifically group A beta-haemolytic streptococcus bacteria. Streptococcal tonsillitis is sometimes called ‘strep throat’.
Symptoms of tonsillitis
If you have tonsillitis, you’ll probably have a sore throat. But having a sore throat doesn’t always mean you have tonsillitis.
Other symptoms of tonsillitis may include:
- pain when swallowing
- finding it hard to swallow
- earache
- high temperature (over 38°C)
- bad breath
- headache
- feeling generally unwell
- feeling sick or vomiting
- tummy pain
You may also notice that you have swollen tonsils and swollen glands in your neck. Your tonsils may be covered with a white coating or white flecks of pus.
Your symptoms may last for about a week. If they’re getting worse or are very bad, contact your GP surgery for advice.
The symptoms of tonsillitis are similar to those of another viral infection, glandular fever. Glandular fever is most likely to affect teenagers and young adults. It can cause a very bad sore throat, slightly raised temperature and swollen glands in your neck. If you have glandular fever, tiredness may last longer. If your GP thinks you may have glandular fever, they may ask you to have a blood test.
Diagnosis of tonsillitis
Your GP will usually diagnose tonsillitis by asking about your symptoms and examining you to see how your throat and tonsils look. They’ll look inside your mouth and may use a bright torch to see better. They won’t usually need to do any other tests.
Your GP may also use a flat wooden stick (tongue depressor) to push your tongue down gently and get a better view of your tonsils. They may feel around your neck to see if you have swollen glands.
If you think you have tonsillitis, you don’t usually need to see a GP unless your symptoms aren’t getting any better while treating it at home., Most people find things improve within a week. But if they don’t, your GP may want to check your throat for another cause.
Under 18 GP Appointments
We now offer GP appointments for children aged between 1 and 18 via our remote video service (UK wide) and face to face appointments at selected centres. Please note that these appointments cannot be booked online so please call 0330 822 3072 for more information or to book. Lines are open Monday to Friday 8am to 8pm, Saturday and Sunday 9am to 5pm. We may record and monitor our calls. Available from £49.
To book or to make an enquiry, call us on 0343 253 8381∧
Self-help for tonsillitis
Tonsillitis usually improves on its own within a week without any antibiotics. You can use self-help measures and over-the-counter medicines to ease your symptoms.
- Rest and take it easy for a few days.
- Drink plenty of fluids to stop you getting dehydrated. This is particularly important if you have a temperature.
- Hot drinks can make your sore throat worse, but some people find warm tea with honey helps. Cold or iced drinks may also help.
- Gargling with a simple mouthwash (such as warm salt water) may help to ease the pain in your throat.
- Throat lozenges may ease your sore throat.
- A throat spray such as benzydamine hydrochloride (eg Difflam) may help to ease pain in your throat.
Over-the-counter medicines can help if your throat is very sore or you have a temperature. These include paracetamol or non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen. Always read the patient information leaflet that comes with your medicine. If you have any questions, ask your pharmacist for advice.
If your symptoms don’t improve after a week or get worse, contact your GP surgery.
Treatment of tonsillitis
Tonsillitis treatment is mainly with self-help measures (see our section on self-help). If you see your GP for tonsillitis, they probably won’t offer you antibiotics because antibiotics aren’t likely to help your symptoms. Antibiotics don’t work against viral infections, which most often cause tonsillitis. Most people with tonsillitis find their symptoms improve after about a week, whether they take antibiotics or not.
Your GP may recommend antibiotics if they think you:
- have very bad symptoms, which could suggest a more severe bacterial infection
- could be prone to serious complications (see our section on complications)
If you do need an antibiotic, your GP will usually prescribe a five- to 10-day course of penicillin. It’s important to tell your GP if you’re allergic to penicillin. If you are, they’ll give you a different antibiotic.
If your GP prescribes antibiotics for your tonsillitis, it’s important to take them properly. Complete the full course, even if you start to feel better. This helps to get rid of all the harmful bacteria and reduces the risk of antibiotic resistance (when antibiotics no longer work against the bacteria).
Always read the patient information leaflet that comes with your medicine. If you have any questions, ask a pharmacist.
Surgery for tonsillitis
Your GP may refer you to an ear, nose and throat (ENT) surgeon if they feel having your tonsils removed will help. This operation is called a tonsillectomy. This will prevent you from getting tonsillitis in the future.
Your doctor will usually suggest a tonsillectomy only if you have had tonsillitis:
- regularly and/or it affects your breathing
- more than seven times in the last year
- five times or more in each of the past two years
- three or more times in each of the past three years
Your doctor may recommend tonsil removal if you’ve had an abscess on your tonsil (a peritonsillar abscess or quinsy). This can be a complication of tonsillitis.
For children, your GP may recommend waiting to see if the tonsillitis gets better on its own before considering surgery. As children get older, they become less likely to have tonsillitis.
A tonsillectomy is a very common operation and can be successful, but it doesn’t mean you won’t get a sore throat in the future.
Although your tonsils are part of your immune system, having them removed doesn’t cause any problems fighting infections. This is because your tonsils are just the visible part of a wider ring of tissue at the back of your throat. When they’re removed, enough of this tissue is left behind to keep fighting infections.
Complications of tonsillitis
Tonsillitis usually improves within a week and doesn’t cause any long-term problems. You’re more likely to have a severe infection or complications if you have a weak immune system. Complications are also more common in young children and older people.
Some people who get tonsillitis keep getting it again and again. This is called recurrent tonsillitis. It may mean you take a lot of time off work or children take a lot of time off school. Recurrent tonsillitis may be a reason to consider having your tonsils removed.
Bacterial tonsillitis can sometimes lead to a build-up of pus on or around your tonsils. This is called a peritonsillar abscess or quinsy. If you have a peritonsillar abscess, you may have very bad pain in your throat, which is often worse on one side. You may also have other symptoms, which include:
- earache
- high temperature
- difficulty swallowing due to pain
- difficulty opening your mouth
Peritonsillar abscess is more common in teenagers and young adults. But children can get it too. The abscess is usually treated with antibiotics and surgery to drain the pus. Your doctor may suggest removing your tonsils if you’ve had a peritonsillar abscess.
Common childhood viruses [podcast]
Why children pick up so many viruses | Podcast | Listen in 18:31 minutes
In this podcast, Bupa GP, Dr Samantha Wild, to discuss common childhood viruses. Find out why children pick up so many viruses and illnesses during childhood, how to manage them and when to seek medical advice. They also discuss how the pandemic has affected general immunity, and whether the vaccination programme will extend to children.
You don’t normally need to see a GP about a sore throat. Most people find their symptoms improve within a week. If your sore throat doesn’t get any better, contact your GP surgery. Also contact your GP if you have:
- difficulty breathing, swallowing saliva or opening your mouth
- persistent high temperature
- severe pain, especially if it’s worse on one side of your throat
- swelling on one side of your neck or throat
For more information, see our section on complications of tonsillitis.
Most people find their symptoms improve within a week by using self-help measures. Tonsilitis is most often caused by a virus, so antibiotics won’t help. It’s important to take the time to rest and take it easy for a few days.
For more information, see our sections on self-help for tonsillitis and treatment of tonsillitis.
Tonsillitis itself isn’t contagious but you can catch the infections that cause it. Tonsillitis is often caused by cold and flu viruses. You may also get tonsillitis if streptococcal bacteria affect your throat. You catch these infections in the same way you catch a cold. Tiny droplets can pass into the air when an infected person talks, coughs or sneezes. You can also catch infections if you touch a surface that’s contaminated with the virus or bacteria.
For more information, see our section on causes of tonsillitis.
Tonsillitis usually goes way on its own within a week. You can take over-the-counter medicines to ease your symptoms. Rest and take it easy for a few days and drink plenty of fluids to keep you hydrated.
For more information, see our sections on self-help for tonsillitis and treatment of tonsillitis.
You can catch tonsillitis most often from a viral infection. Viral tonsillitis is usually due to a common cold virus, but it may also be caused by other viruses, including the flu virus. For around one in three people, tonsillitis is caused by bacteria.
For more information, see our section on causes of tonsillitis.
One of the first signs of tonsillitis is a sore throat, although having a sore throat doesn’t always mean you have tonsillitis. Other tonsillitis symptoms may include a high temperature (over 38°C) and a headache, and you may generally feel unwell.
For more information, see our section on symptoms of tonsillitis.
Adenoid and tonsil removal
Adenoid and tonsil removal is a procedure that involves taking away small lumps of tissue at the back of your nose and throat.
Antibiotics
Over-the-counter painkillers
Did our Tonsillitis information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Sore throat – acute. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised January 2023
- Sore throat (acute): antimicrobial prescribing. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 26 January 2018
- Tonsillitis. Patient. patient.info, last updated 1 February 2023
- Tonsil and adenoid anatomy. Medscape. emedicine.medscape.com, updated 20 July 2015
- Sore throat (acute): antimicrobial prescribing. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 26 January 2018
- Tonsillitis. BMJ Best Practice. bestpractice.bmj.com, last reviewed 6 May 2023
- Infectious mononucleosis. BMJ Best Practice. bestpractice.bmj.com, last reviewed 6 May 2023
- Tonsillopharyngitis. MSD Manuals. msdmanuals.com, reviewed/revised March 2022
- Tonsillitis and peritonsillar abscess. Medscape. emedicine.medscape.com, updated 18 February 2022
- Ear, nose and throat examination. Patient. patient.info, last updated 21 July 2021
- Benzydamine hydrochloride. NICE British National Formulary. bnf.nice.org.uk, last updated 28 June 2023
- Antimicrobial stewardship: changing risk-related behaviours in the general population. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 25 January 2017
- Peritonsillar abscess. Patient. patient.info, last updated 21 July 2021
- Tonsillitis. Anderson J, Paterek E. StatPearls Publishing. www.ncbi.nlm.nih.gov, last updated 18 September 2022
- Tonsillectomy (taking out your tonsils) because of repeated infections. ENTUK. www.entuk.org, accessed 6 June 2023
- Common cold. Patient. patient.info, last updated 30 May 2022

