Colonoscopy
Your health expert: Mrs Sara Badvie, Consultant Laparoscopic, Colorectal and General Surgeon
Content editor review by Rachael Mayfield-Blake, March 2022
Next review due March 2025
A colonoscopy is a procedure that uses a narrow, flexible, telescopic camera called a colonoscope to look inside your large bowel. The large bowel is also known as the colon or large intestine. A colonoscopy is used to investigate symptoms that affect your bowel, and to check for signs of bowel cancer.
Why do I need a colonoscopy?
Screening
You may be offered a colonoscopy as part of the national bowel cancer screening programme in England, Wales and Northern Ireland. Bowel cancer screening is offered to everyone over the age of 60, every two years. The programme is gradually expanding to people younger than this in England. If you live in Scotland and are aged 50 to 74, you’ll be offered screening every two years.
The first stage of the screening programme is a kit that you complete at home, called the faecal immunochemical test (FIT). You use this to collect a sample of poo, which is tested in a laboratory for traces of blood that you wouldn’t usually notice by looking at it. If blood is found in your poo, you’ll be offered a colonoscopy. This happens to about 2 in every 100 people who take the FIT test.
Other reasons for a colonoscopy
Your doctor may recommend you have a colonoscopy for one of the following reasons.
- To investigate symptoms that could indicate bowel cancer, such as bleeding from your bottom or a change in your bowel habits. A change in bowel habits could be needing to poo more often, having diarrhoea or being constipated.
- Having a strong family history of bowel cancer. Examples of a strong family history include two or more first-degree relatives with bowel cancer or one relative under the age of 45 who had it. A first-degree relative is a parent, brother or sister.
- To investigate symptoms of inflammatory bowel disease (for example, ulcerative colitis or Crohn’s disease). Also, to monitor your bowel if you’ve been diagnosed with these conditions.
- To monitor your bowel if you’ve previously had a polyp or cancer removed. Also, to monitor your bowel if you have a family history of an inherited polyp syndrome.
- As a follow-up to another test – such as a CT scan or virtual colonography – if you need further assessment or treatment.
Your doctor or nurse can also perform a biopsy (remove a sample of tissue) or remove polyps during a colonoscopy, if necessary.
Preparation for a colonoscopy
You’ll usually have a colonoscopy in the endoscopy unit at a hospital and will be able to go home the same day. Ask a friend or family member to drive you home because you’ll usually have sedation. Sedation can make you feel drowsy for a while afterwards, so you won’t be able to drive until the day after.
Your hospital will give you detailed instructions about what else you need to do to prepare for your colonoscopy.
A specially trained nurse or doctor, called an endoscopist, will carry out your colonoscopy. You’ll meet them beforehand, so they can explain what will happen during the procedure and what to expect afterwards. They’ll also discuss the potential complications.
Your endoscopist will assess whether or not you’re fit enough to have a colonoscopy. So, remember tell them if you’re pregnant, breastfeeding or have any health conditions.
If you’re invited for a colonoscopy as part of the screening programme, you’ll have an appointment with a specialised screening practitioner to discuss everything.
Be sure to ask any questions you have and ask for more time to make a decision if you need to. If you’re happy to go ahead with the procedure, you’ll be asked to sign a consent form.
Some hospitals are JAG accredited. JAG stands for the Joint Advisory Group on Gastrointestinal Endoscopy. A unit with JAG accreditation will have been assessed as having high quality services that meet certain criteria for performing endoscopy procedures.
Medicines
There are certain medicines that you need to stop taking before you have a colonoscopy. These include:
- iron tablets –stop taking these one week before your colonoscopy
- anti-diarrhoea medicines or any medicines that may cause constipation – stop taking these one to two days before your colonoscopy
- medicines that affect the way your blood clots (for example, warfarin or clopidogrel) – you usually need to stop taking these five days before your colonoscopy
If you take any of these medicines (or any others), let your hospital know before you have the colonoscopy. They can check if you need to stop taking them and for how long.
Clearing your bowel
Your bowel needs to be completely empty for the procedure so that your endoscopist can see everything clearly. Your hospital will give you a strong laxative to take before your colonoscopy. It usually comes as a powder that you mix with water. Let your hospital know if you’re pregnant or breastfeeding as you may not be able to take the laxative.
The laxative can quickly give you diarrhoea, so make sure you stay close to a toilet after you take it. You might feel some discomfort or bloating in your tummy (abdomen).
The laxative can taste unpleasant. It may help to drink it slowly, and it might taste better if you put the mixture in the fridge before you drink it. Although the laxative can be unpleasant, it is really important to clear your bowel so your endoscopist can see your bowel and identify anything abnormal.
Your hospital will give you advice about what you can eat or drink before the procedure. They may ask you to eat only low-fibre foods or to fast for at least a day beforehand. This can vary between hospitals and if you have any health conditions such as diabetes. So, follow the instructions your hospital gives you, and ask if you’re not sure about anything. It’s important to keep drinking plenty of clear fluids like water, squash or black tea or coffee, to make sure you don’t get dehydrated.
If you take the contraceptive pill, laxatives will prevent it being absorbed. Follow the instructions in the patient information leaflet for your contraceptive pills. You may need to use another form of contraception, such as a condom, for a while.
If you have diabetes or if you’re having another procedure such as a gastroscopy on the same day, the preparation for a colonoscopy may be different for you. Follow the instructions your hospital gives you and, if you’re unsure, ask.
At the hospital
When you arrive at the hospital, you’ll see a nurse or doctor and can ask them any final questions. They’ll give you a hospital gown to wear and sometimes a pair of paper shorts that open at the back
Colonoscopy procedure
A colonoscopy usually takes around 30 to 45 minutes, although the appointment itself will last longer than this. Make sure you allow plenty of time for getting there, parking and going home.
You won’t need an anaesthetic for a colonoscopy but your hospital may offer you a painkiller and sedation. This is because the procedure can be uncomfortable, A sedative will make you feel more relaxed and a bit drowsy, but you’ll stay awake during the procedure. The sedative is given as an injection into a vein in your hand at the start of the procedure. At some hospitals, you might be offered gas and air (Entonox) for pain relief instead of a sedative.
Your endoscopist (doctor or nurse) will ask you to lie on your left-hand side and bend your knees. First, they’ll gently examine your bottom with their finger. They’ll then carefully insert the colonoscope, using lubricating gel to make it as comfortable as possible.
Your endoscopist will pump air into your bowel through the colonoscope to inflate it slightly and give a better view of your bowel. This can make you feel a little bloated. Your endoscopist will gently guide the colonoscope through your bowel.
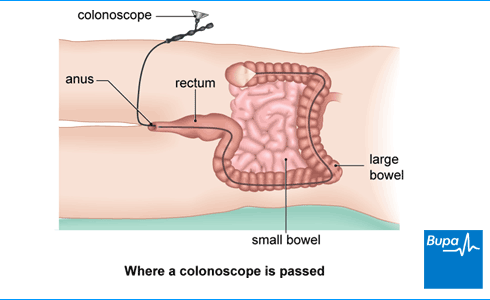
The images from the camera at the end of the colonoscope will appear on a monitor. Your endoscopist might ask you to change position during the procedure to help them to look at different areas of your bowel. They may ask an assistant to press on your tummy to help move the colonoscope in the right direction.
Your endoscopist may take a small sample of cells (a biopsy) if needed. They may remove any growths (polyps) they find. They’ll pass instruments through the colonoscope to do this.
If you find the procedure particularly uncomfortable at any stage, tell your endoscopist and they’ll stop or change what they’re doing.
Aftercare for colonoscopy
If you’ve had sedation for your colonoscopy, you’ll be monitored for an hour or so until the immediate effects of the sedative have passed. After that, you should be fine to go home when you feel ready. Ask someone to take you home and stay with you overnight while the sedative wears off.
Before you leave, your doctor or nurse may talk to you about the colonoscopy and if they removed any polyps or took any biopsies. You may be given a copy of the colonoscopy report. If you’ve had a biopsy or polyps removed, they’ll tell you how and when you can expect to receive your results. It’s usually within two weeks.
Recovery for colonoscopy
You may feel bloated and have some cramping pain after a colonoscopy. This is caused by the gas used during the procedure and usually settles down within a few hours. If you need pain relief, you can take over-the-counter medicines, such as paracetamol or ibuprofen. You may also bleed a little from your bottom if you’ve had a biopsy or a polyp removed. This should stop within a couple of days – contact your GP or the hospital if it doesn’t.
Having sedation can be very tiring. You might find that you’re not as co-ordinated as usual or that it's difficult to think clearly. This should pass within 24 hours. In the meantime, don't drive, drink alcohol, operate machinery or make any important decisions.
Complications of colonoscopy
Complications are when problems occur during or after the procedure. The main complications of a colonoscopy are listed below.
- Breathing problems. You may have a reaction to the sedation, which can affect your breathing or your heart rate. But your healthcare team will monitor you throughout the procedure, and you can have treatment if this does happen.
- A tear in your bowel (bowel perforation), caused by the colonoscope. This is rare. If a tear does happen, you’ll probably need an operation to repair it.
- Bleeding. This is most likely to happen after having biopsies or polyps removed, and usually stops on its own. But sometimes it can become more serious and you may need a blood transfusion, but this rarely happens.
Contact the hospital department where you had your procedure if you continue to bleed from your bottom or have severe pain in your tummy that doesn’t get better within a couple of days.
Alternatives to colonoscopy
A colonoscopy is usually the best investigation to see inside your bowel because it can examine the whole of your large bowel. At the same time, it can detect very small changes. But it isn’t suitable for everyone so your doctor might suggest other tests. Other options include the following.
- Virtual colonoscopy. This involves having a CT scan of your large bowel after gas is passed into your bowel to expand it.
- Flexible sigmoidoscopy. This is similar to a colonoscopy but uses a shorter instrument to look inside only the lower part of your large bowel.
- Barium enema. This involves taking X-ray images of your large bowel using a contrast or dye (barium) to show up the detail and give clearer X-ray images.
- Colon capsule endoscopy. In this procedure, you swallow a small capsule that contains a tiny video camera. As it passes through your bowel, the camera takes digital pictures that your doctor can see on a monitor. This is a new treatment that isn’t yet available in all hospitals.
If you have one of these tests, you may need a colonoscopy afterwards to take a closer look at your bowel. Or you may need some other procedure.
You may feel bloated and have some cramping pain for a few hours after a colonoscopy. This is because of the gas used during the procedure. You can take over-the-counter medicines such as paracetamol or ibuprofen to ease the pain. If you have a sedative, it can be very tiring but you should recover within 24 hours.
For more information, see our section: Recovery for colonoscopy.
A colonoscopy can check your large bowel for any signs of bowel cancer. It is used in bowel cancer screening programmes. It can also investigate any bowel-related symptoms to help your doctor diagnose conditions such as ulcerative colitis or Crohn’s disease. And it can be used to monitor your bowel if you’ve been diagnosed with these already.
For more information, see our section: Why do I need a colonoscopy?
Yes, you’ll be awake for a colonoscopy, but your hospital may offer you sedation. This will make you feel more relaxed and a bit drowsy. Some hospitals offer gas and air (Entonox) instead of a sedative.
For more information, see our section: Colonoscopy procedure.
The laxative can give you diarrhoea, so make sure you stay close to a toilet after you take it. How long you’ll have diarrhoea can vary. It’s best to stay at home for a few hours.
A standard colonoscope (for use in adults) is a long flexible tube that’s about 11 to 13mm wide. You won’t need an anaesthetic for a colonoscopy, but as the procedure can be uncomfortable, your hospital may offer you a painkiller and sedation.
Polyps are small lumps that can develop in the lining of your bowel. They don’t usually cause any problems but sometimes, over time, a type of polyp will grow into a cancer. If your doctor finds any polyps during your colonoscopy, they’ll remove them. Afterwards, you might need to have regular colonoscopies to check whether you’ve developed any more.
For more information, see our section: Why do I need a colonoscopy?
Bowel cancer
Bowel cancer (or colorectal cancer) is the name for any cancer that starts in your large bowel, rectum (back passage) or appendix.
Crohn's Disease
Crohn’s disease is an inflammatory condition that affects your gastrointestinal tract.
Ulcerative colitis
Ulcerative colitis is a condition that affects your large bowel and rectum (back passage).
Did our Colonoscopy information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- NHS bowel cancer screening: helping you decide. Public Health England. www.gov.uk, updated 31 October 2021
- Colorectal assessment. Colorectal Surgery. Oxford Medicine Online. oxfordmedicine.com, published online August 2021
- Guidance. Bowel cancer screening: Programme overview. Public Health England. www.gov.uk, last updated 17 March 2021
- Bowel screening. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised May 2019
- Colorectal cancer. BMJ Best Practice. bestpractice.bmj.com, last updated 18 January 2022
- Gastrointestinal medicine. Oxford Handbook of General Practice. Oxford Medicine Online. oxfordmedicine.com, published online June 2020
- Polyps of the colon and rectum. MSD Manuals. msdmanuals.com, last full review/revision March 2021
- Bowel cancer screening: having a colonoscopy. Public Health England. www.gov.uk, updated 31 October 2021
- Guidance on professional standards and ethics for doctors. Decision making and consent. General Medical Council. www.gmc-uk.org, published 30 September 2020
- Service accreditation. Joint Advisory Group on GI Endoscopy. www.thejag.org.uk, accessed 18 February 2022
- Moviprep. NICE British National Formulary. bnf.nice.org.uk, last updated 3 February 2022
- Macrogol 3350 with anhydrous sodium sulfate, potassium chloride, sodium bicarbonate and sodium chloride. NICE British National Formulary. bnf.nice.org.uk, last updated 3 February 2022
- Colonoscopy. Medscape. emedicine.medscape.com, updated 4 February 2022
- Colonoscopy. Cancer Research UK. www.cancerresearchuk.org, last reviewed 15 March 2019
- Microgynon 30 tablets. emc. www.medicines.org.uk, last updated 8 June 2020
- Personal communication, Mrs Sara Badvie, Consultant Laparoscopic, Colorectal and General Surgeon, 9 March 2022
- Anaesthesia explained. Royal College of Anaesthetists. www.rcoa.ac.uk, published 1 March 2021
- Flexible sigmoidoscopy. Medscape. emedicine.medscape.com, updated 27 October 2020
- Barium X-ray. Cancer Research UK. www.cancerresearchuk.org, last reviewed 5 March 2019
- Capsule endoscopy. Medscape. emedicine.medscape.com, updated 19 January 2022

