Calcium-channel blockers
Your health expert: Madeeha Waheed, Oncology Pharmacist at Bupa, Clinical and Operational Improvement
Content editor review by Rachael Mayfield-Blake, Freelance Health Editor, November 2021.
Next review due November 2024.
Calcium-channel blockers are medicines that work on the cells of your heart and arteries (blood vessels). They can treat a number of different health conditions.
Uses of calcium-channel blockers
Your doctor may prescribe calcium-channel blockers if you have:
- angina
- high blood pressure
- a disturbance of your normal heart rhythm (arrhythmia)
- Raynaud's phenomenon (a health condition that affects your blood vessels in cold temperatures or when you’re stressed)
- cluster headaches (severe headaches that usually affect the area around one eye or temple)
These medicines aren’t suitable for everyone. If you’re pregnant or breastfeeding, you shouldn’t take some types of calcium-channel blockers, and others may cause problems. So, let your doctor know if you’re pregnant, breastfeeding or trying for a baby. Tell them if you have any other health conditions and about any medicines you take too. See Interactions below for more about this.
It’s your decision whether to take a medicine or not. Discuss your options with your doctor and ask them about the pros and cons of any medicines they suggest.
How calcium-channel blockers work
Calcium plays a key role in how the muscles in your heart and arteries contract to pump blood round your body. To do this, calcium flows into these cells through holes, or channels.
Effect on the heart
Calcium-channel blockers slow down the amount of calcium that can get into your heart muscle cells. This reduces how fast and strongly your heart can contract (pump). The medicines also act on cells that conduct the electrical flow in your heart and this affects the speed of this electrical flow through your heart. These effects can help with the symptoms of angina and irregular heart rhythms.
Effect on blood vessels
Calcium-channel blockers restrict how much calcium can enter the muscle cells in your blood vessels. These then relax, causing the arteries to widen (this is called vasodilation). This helps to lower your blood pressure. Calcium-channel blockers also prevent angina by widening the coronary arteries that supply your heart. This allows more oxygen to reach the heart muscle cells.
Types of calcium-channel blockers
There are two main groups of calcium-channel blocker.
- Dihydropyridine calcium-channel blockers widen your arteries. Examples include amlodipine, felodipine (eg Cardioplen XL and Felotens XL) and nifedipine (eg Adipine XL and Nifedipress MR). Dihydropyridines may be used to treat Raynaud’s phenomenon, angina and high blood pressure.
- Non-dihydropyridines, or ‘rate-limiting’ calcium-channel blockers widen your arteries and affect your heart. Examples include diltiazem (eg Dilzem SR and Zemtard) and verapamil (eg Securon SR and Vertab SR). These reduce how hard it has to work and how fast it beats. Your doctor may prescribe these medicines to treat angina, high blood pressure and arrhythmia.
Your doctor will offer you the calcium-channel blocker that’s most suitable for you. This will depend on what health condition you have, as well as your general health and other medicines that you take.
Worried about your heart health?
Get a picture of your current health and potential future health risks with one of our health assessments.
To book or to make an enquiry, call us on 0333 920 7695∧
Taking calcium-channel blockers
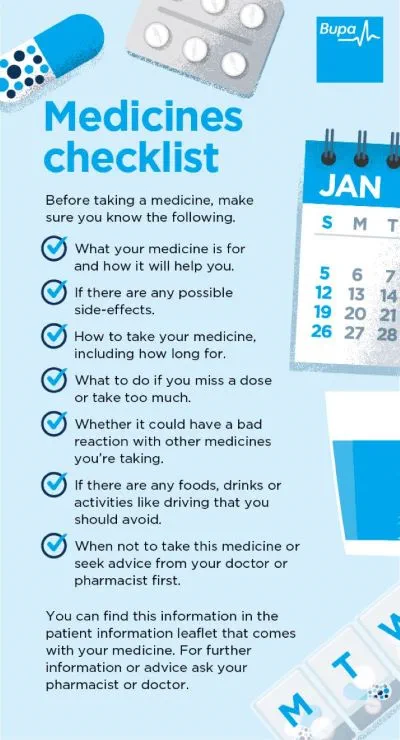
Calcium-channel blockers are only available on prescription, usually as tablets. The information that comes with your medicine will tell you how to take it, and how often. Some calcium-channel blockers come in long-acting ('modified release') versions.
If you forget to take a tablet, check the patient information leaflet that comes with your medicine. This will explain what you need to do if you miss a dose. Don’t stop taking your calcium-channel blockers unless your doctor tells you to. If you suddenly stop taking calcium-channel blockers, it can raise your blood pressure and cause pain and tightness in your chest (angina). If you’d like to stop taking your medicine, your doctor will tell you how to do this safely.
Always follow the instructions your doctor or pharmacist gives you about when to take your medicines. Read the patient information leaflet that comes with your medicine carefully. If you have any questions about your medicines or how to take them, ask your pharmacist.
If you take too much medicine, or think you’re reacting badly to it, seek advice from a health professional immediately. This could be from your pharmacist, doctor or the hospital.
Interactions of calcium-channel blockers
Calcium-channel blockers may interact with some foods and medicines. For instance:
- grapefruit juice can increase the effects of some calcium-channel blockers, which can cause problems
- alcohol and calcium-channel blockers can both cause low blood pressure, so together might cause problems
Check the information that comes with your medicine to see if there are any recommendations about foods and drinks to avoid. And if you have any queries, ask your pharmacist.
Calcium-channel blockers may interact with other medicines, including some other heart medicines and some antibiotics. If you’re taking beta-blockers, you won’t be able to take certain calcium-channel blockers. Always check with your pharmacist or doctor before you take any other medicines or herbal remedies at the same time as a calcium-channel blocker.
Side-effects of calcium-channel blockers
You may not get any calcium-channel blocker side-effects but, as with all medicines, there's a possibility. Side-effects vary, according to which calcium-channel blocker you take. The patient information leaflet can tell you exactly which side-effects may happen and how common they are with your particular medicine. Some of the most common side-effects of calcium-channel blockers include:
- flushing
- headache
- swelling in your feet and ankles
- dizziness
- rapid or irregular heart beat (palpitations)
- nausea (feeling sick or being sick) rashes
Some calcium-channel blockers, especially verapamil, may cause constipation. This is because calcium-channel blockers have an effect on the muscle that forms part of the walls of your bowel. This can slow down movements in your bowel and lead to constipation.
Side-effects may settle down on their own, so give your new medicine a chance and wait a few days to see if things get better. If the side-effects continue and you feel unwell, contact your doctor. Don’t stop taking the medicine without discussing it with your GP first.
Calcium-channel blockers are medicines that work on your heart and your arteries (blood vessels). They can treat a number of different health conditions, such as angina and high blood pressure. They’re only available on prescription, usually as tablets.
See our section: Uses of calcium-channel blockers above for more information about what they can treat.
Calcium-channel blockers sometimes have letters such as SR, XL, LA or MR in the name. This means they have been designed to release your medicine slowly and steadily over a longer period of time. Doctors often refer to them as ‘modified release’ medicines. If you have this type of calcium-channel blocker, swallow them whole – don’t chew or crush them up as their slow-release mechanism will no longer work.
Calcium-channel blockers aren’t suitable for everyone. Let your doctor know if you’re pregnant, breastfeeding or trying for a baby, as you shouldn’t take some types of calcium-channel blockers, and others may cause problems. Let them know if you have any other health conditions and take medicines for them too.
See our sections: Uses of calcium-channel blockers and Interactions of calcium-channel blockers above for more information.
Which calcium-channel blocker is best will depend on your individual circumstances. Your doctor will take into account if you have any other health conditions and if you take any other medicines. For example, if your only health problem is high blood pressure, they may prescribe you a medicine called amlodipine (eg Istin). Whereas if you also have angina, they may prescribe you a medicine called felodipine (eg Cardioplen). Your doctor will explain what the best choice is for you.
Angina
Angina is when you have chest pain or an uncomfortable tight feeling in your chest.
High blood pressure (hypertension)
Heart attack
Coronary heart disease
Other helpful websites
Did our Calcium-channel blockers information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Cardioprotective drugs. The ESC textbook of preventive cardiology. Oxford Medicine Online. oxfordmedicine.com, published online June 2015
- Calcium-channel blockers. NICE British National Formulary. bnf.nice.org.uk, last updated 2 September 2021
- Nifedipine. NICE British National Formulary. bnf.nice.org.uk, last updated 2 September 2021
- Raynaud's phenomenon. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised February 2020
- Cluster headache. BMJ Best Practice. bestpractice.bmj.com, last reviewed 6 September 2021
- Felodipine. NICE British National Formulary. bnf.nice.org.uk, last updated 2 September 2021
- Lacidipine. NICE British National Formulary. bnf.nice.org.uk, last updated 2 September 2021
- Drug cabinet: calcium-channel blockers. British Heart Foundation. www.bhf.org.uk, accessed 7 October 2021
- Therapy-related issues: Cardiovascular system. Oxford handbook of clinical pharmacy. Oxford Medicine Online. oxfordmedicine.com, published online April 2017
- Calcium-channel blocker toxicity. Medscape. emedicine.medscape.com, updated 25 March 2021
- Calcium-channel blockers. Statpearls [internet]. McKeever RG, Hamilton RJ. www.ncbi.nlm.nih.gov, last update 25 July 2021
- Hypertension. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised April 2021
- Verapamil hydrochloride. NICE British National Formulary. bnf.nice.org.uk, last updated 2 September 2021
- Diltiazem hydrochloride. NICE British National Formulary. bnf.nice.org.uk, last updated 2 September 2021
- Calcium-channel blockers (CCBS). Blood Pressure UK. www.bloodpressureuk.org, accessed 7 October 2021
- Verapamil. NICE British National Formulary. bnf.nice.org.uk, last updated 2 September 2021
- Diltiazem. NICE British National Formulary. bnf.nice.org.uk, last updated 2 September 2021
- Constipation. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised September 2021
- Personal communication, Madeeha Waheed, Oncology Pharmacist at Bupa Clinical and Operational Improvement, 17 November 2021
- Amlodipine. NICE British National Formulary. bnf.nice.org.uk, last updated 2 September 2021