Transurethral resection of the prostate (TURP)
Your health expert: Mr Aziz Gulamhusein, Consultant Urologist and Robotic Surgeon
Content editor review by Victoria Goldman, August 2022
Next review due November 2025
Transurethral resection of the prostate (TURP) is a surgical procedure that involves removing part of the prostate gland. It’s used to treat a common condition where the prostate gets bigger, making it harder to pee. This condition is called benign prostatic hyperplasia (BPH).
Why would I need a TURP?
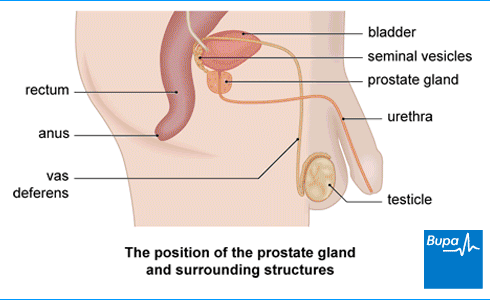
Transurethral resection of the prostate (TURP) may be used to treat an enlarged prostate (called benign (non-cancerous) prostate hyperplasia or BPH). If you have this prostate problem, your prostate gland gets bigger and blocks the flow of pee from your bladder. This can mean you find it hard to pee.
If you have TURP, part of your prostate gland is removed to try and boost the flow of pee. Your surgeon does this procedure through your urethra (the tube that carries pee from your bladder and out through your penis).
The prostate gland gets bigger in most men as they get older. If you have BPH, your GP will suggest other ways of controlling your symptoms first. These may be:
- lifestyle changes
- bladder and pelvic muscle training
- tablets
If these aren’t working and your symptoms aren’t getting better, your GP may refer you to a specialist in urinary tract problems. The specialist will decide whether TURP or other treatments may be right for you.
Deciding on TURP
Like any medical procedure, having a transurethral resection of the prostate (TURP) has lots of pros and cons. So, you’ll need to discuss the advantages and disadvantages with your surgeon.
For many people, TURP works well at boosting the flow of pee and easing BPH symptoms. These effects usually last for a long time and may improve your quality of life. But some people find their symptoms don’t completely go away after TURP. You may need to have the procedure again. The prostate gland always keeps growing, but most men won’t need another procedure for around 10 years.
You should be aware of the risk of complications, such as retrograde ejaculation – see the Complications of TURP section below for more information. If you go ahead with the procedure, you’ll need to prepare yourself for a short hospital stay and a recovery period of a few weeks.
Your surgeon will discuss with you what will happen before, during and after your surgery. If you’re unsure about anything, don’t be afraid to ask. No question is too small. It’s important that you feel fully informed and are happy to give your consent for the operation to go ahead. You’ll be asked to do this by signing a consent form.
Alternatives to TURP
Transurethral resection of the prostate (TURP) is just one way to treat an enlarged prostate gland. Other options include the following.
- Holmium laser enucleation of the prostate (HoLEP). This uses a high-powered laser to remove part of your prostate.
- Robotic prostatectomy. This uses keyhole surgery and robot-assisted techniques to remove your prostate gland. Robotic arms hold the instruments, which gives the surgeon more accuracy. The surgeon controls the instruments and the robot can’t work on its own.
- Transurethral vaporisation of the prostate (TUVP). This uses an electrical current to burn away parts of your prostate.
- Greenlight laser surgery. This uses a special laser to destroy prostate tissue without leaving any fragments behind.
- Transurethral incision of the prostate (TUIP). Your surgeon makes small cuts in the neck of your bladder and prostate to widen the bladder opening. It may be an option if your prostate is only slightly bigger than normal.
- Open prostatectomy. This surgery takes away part of your prostate through a cut in your tummy, rather than going through the urethra. It’s usually only suggested for a very large prostate.
- Urethral lift implant. This may be offered for a smaller prostate. The surgeon uses a small implant to pull the prostate tissue away from the urethra to open it up. One device approved for this procedure is called UroLift.
- Prostate artery embolisation. This procedure blocks the blood supply to your prostate gland. This causes some of the tissue to die so your prostate gets smaller.
- Rezum steam treatment. This uses steam to destroy part of your prostate. The steam is delivered to your prostate using an instrument inserted through your urethra.
Your surgeon will talk to you about which treatment is best for you. This will depend on lots of things, including:
- your symptoms
- how big your prostate is
- whether you have any other health problems
- what’s available at your local private hospital
Preparing for TURP
Your surgeon or nurse will assess you before your operation to check you’re fit for surgery. This may be at a pre-operative assessment clinic. They’ll also explain how to get ready for your operation.
- If you smoke, you’ll be asked to stop. Smoking makes you more likely to have an infection and other complications after surgery.
- If you’re taking any medicines, you may be advised to stop some of these before the operation.
TURP is usually carried out under a general anaesthetic. This means you’ll be asleep during the procedure. Sometimes, you may have a spinal anaesthetic instead. This means you’ll be awake, but won’t be able to feel anything from your waist down. Your surgeon or anaesthetist will discuss with you which type of anaesthesia is best for you.
If you’re having a general anaesthetic, you’ll be given clear instructions about when to stop eating and drinking before your operation. It’s important to follow these instructions.
On the day of your operation, your surgeon will meet with you to check you’re well and still happy to go ahead. You may be asked to wear compression stockings. You may be given an injection of an anticlotting medicine called heparin. This helps to stop blood clots forming in the veins in your legs. You may also have an injection of antibiotics to help prevent infections after surgery.
How healthy are you?
With our health assessments you get an action plan that’s tailor-made for you.
To book or to make an enquiry, call us on 0370 218 8122∧
What happens during TURP?
Transurethral resection of the prostate (TURP) usually takes around 45 minutes to an hour.
The surgeon will check the anaesthetic’s working. Then, they’ll feed a thin telescopic tube up through your urethra (the tube in your penis that carries urine out of your body) into your bladder. This gives them a good view of your prostate. Then they’ll put in an electrically heated wire loop. They’ll use this to cut out small pieces from the middle of your prostate. Your surgeon then uses suction to remove the pieces of prostate from your bladder. These are sent to a laboratory for testing.
At the end of the procedure, your surgeon will put a tube (catheter) into your bladder. They’ll use a saltwater fluid (saline) to flush through any clots, blood and loose tissue.
What to expect afterwards
You may need to stay in hospital for up to three nights after you’ve had TURP. You’ll need to rest until the effects of the anaesthetic have worn off. You may have some discomfort as the anaesthetic wears off, but you'll be offered pain relief if you need it.
Your catheter will need to stay in place for up to a week. It will drain urine from your bladder into a bag. For the first day or so, you’ll have sterile fluid running through the catheter to wash out your bladder and help flush out blood clots. When your catheter is taken out, your nurse will check that you can pee normally. Not everyone can pee straightaway. If you have any problems, you’ll have a new catheter put in for a week or so.
After your catheter is taken out, you may notice blood in your urine for a while. It may also hurt or burn when you pee. You may need to pee more often too. These symptoms can come and go while you recover. They usually get better in a few days and aren’t normally anything to worry about.
When you’re ready to leave hospital, you’ll need to arrange for someone to drive you home. Before you leave, your doctor or nurse will give you some advice about your recovery and information about follow-up appointments.
Recovering from TURP
It can take several weeks to fully recover from TURP. Any side-effects will normally settle down by around six weeks. You should be prescribed any medicines you need – including painkillers from the hospital to take home with you. You may have a little stinging when you pee, but this shouldn’t hurt. You can also take over-the-counter painkillers, such as paracetamol or ibuprofen if you need them.
You may be given instructions to drink more than normal for a day or two. This will help to flush out your bladder and means you’re less likely to get an infection. You may have some blood clots in your pee around 10 to 14 days after your procedure. These are scabs from your prostate healing and coming away. If drinking more doesn’t clear this up, contact your GP.
Most people wait two or three weeks before going back to work. But always follow your surgeon’s advice. If your job is strenuous or involves heavy lifting, you may need to stay off work for longer. It’s best to wait at least two weeks before having sex.
Pelvic floor exercises
You’ll usually be advised to do pelvic floor exercises when you get home. Your pelvic floor is a layer of muscle that supports your bladder and bowel. Doing the exercises will help your bladder control.
Your doctor or nurse at the hospital will explain how to do the exercises, and how often.
- You can contract your pelvic floor muscles by tightening the ring of muscle around your back passage (anus) as if you're trying to control wind.
- At the same time, imagine you’re passing urine and try to stop the flow mid-stream – then restart it.
- You may see your penis dip down slightly.
Don’t give up even if you think they aren’t working – it can take a few months to see any changes. It can take time to get the technique right, so don’t be discouraged if you find it difficult at first.
Complications of Turp
Complications are problems that can happen during or after your procedure. The possible complications of any surgery include:
- an unexpected reaction to the anaesthetic
- a lot of bleeding
- getting a blood clot, usually in a vein in your leg (deep vein thrombosis or DVT)
Specific complications of TURP include the following.
- Retrograde ejaculation. This means you have little or no semen when you ejaculate. The semen passes into your bladder instead of out of your penis. This happens in up to seven out of 10 men who have a TURP.
- Urine infections. It’s common to have some pain when you pee at first after a TURP. But if your pain gets worse, you have a high temperature or your pee is cloudy and smelly, contact your GP surgery. It could be a sign of an infection. You may need antibiotics to clear it up.
- Narrowing of the tube from the bladder (urethral stricture) caused by scarring. This can happen in up to one in 10 men. It can slow the flow of urine.
- Regrowth of the prostate. In up to one in 10 men the prostate regrows and blocks urine flow again years later. If this happens, you may need to have TURP again.
- Incontinence (leaking urine). This usually gets better with time but sometimes can be a long-term problem. If you’re having trouble with this, contact your GP and they can talk you through the options available to manage it.
- Erectile dysfunction. This can happen in up to one in 10 men who had normal erections before their TURP. Or you may have had problems with erections before your operation. This may carry on after TURP. There are medicines and other treatments that may help.
Laser treatments may mean less bleeding, a shorter hospital stay and shorter time needing a catheter. Your surgeon will advise whether TURP or laser is best for you. See our Alternatives to TURP section for more information.
You may notice some blood clots in your pee. You may also have incontinence (leaking pee) after TURP too. But these should all clear up after a few weeks. For more information, see our Recovering from TURP section.
Prostate cancer
Men's Health
Explore our information on a range of conditions, treatments and procedures relating to men's health.
Did our Transurethral resection of the prostate (TURP) information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Transurethral Resection of the Prostate. Medscape. emedicine.medscape.com, updated September 2021
- Benign prostatic hyperplasia (BPH). MSD Manual. www.msdmanuals.com, last full review/revision November 2020
- Benign prostatic hyperplasia. BMJ Best Practice. bestpractice.bmj.com, last reviewed June 2022
- Benign prostatic hyperplasia (BPH). Patient. patient.info, last edited June 2021
- Transurethral prostatectomy (TURP) for benign disease. British Association of Urological Surgeons. www.baus.org.uk, published July 2021
- Good surgical practice. Consent. The Royal College of Surgeons. www.rcseng.ac.uk, published September 2014
- Holmium laser enucleation of the prostate (HoLEP). British Association of Urological Surgeons. www.baus.org.uk, published June 2021
- GreenLight XPS for treating benign prostatic hyperplasia. The technology. National Institute for Health and Care Excellence (NICE) Medical Technologies Guidance MTG29. www.nice.org.uk, published June 2016
- 2022 Non-neurogenic Male LUTS Guidelines. European Association of Urology. uroweb.org, updated 2022
- Open (Millin's) prostatectomy for benign obstruction. British Association of Urological Surgeons (BAUS).
- UroLift for treating lower urinary tract symptoms of benign prostatic hyperplasia. Recommendations. National Institute for Health and Care Excellence (NICE) Medical Technologies Guidance MTG58. www.nice.org.uk, published May 2021
- Prostate artery embolisation for lower urinary tract symptoms caused by benign prostatic hyperplasia. National Institute for Health and Care Excellence (NICE) Interventional Procedures Guidance IPG611. www.nice.org.uk, published April 2018
- Rezum for treating lower urinary tract symptoms secondary to benign prostatic hyperplasia. Recommendations. National Institute for Health and Care Excellence (NICE) Medical Technologies Guidance MTG49. www.nice.org.uk, published June 2020
- You and your anaesthetic. Royal College of Anaesthetists. www.rcoa.ac.uk, published February 2020
- Joint briefing: smoking and surgery. Action on Smoking and Health, the Royal College of Anaesthetists, the Royal College of Surgeons of Edinburgh and the Faculty of Public Health. ash.org.uk, published April 2016
- Transurethral Resection of the Prostate. Medscape. emedicine.medscape.com, updated September 2021
- Pelvic floor exercises in men. British Association of Urological Surgeons. www.baus.org.uk, published September 2020
- Urinary tract infection in adults. Patient. patient.info, last reviewed January 2022
- Urethral stricture. The MSD Manuals. www.msdmanuals.com, last full review/revision May 2021
- Benign prostatic hyperplasia (BPH) treatment and management. Medscape. emedicine.medscape.com, last updated February 2021
- Erectile dysfunction. Patient. patient.info, last reviewed March 2022
- Caring for someone recovering from a general anaesthetic or sedation. 2nd ed. Royal College of Anaesthetists. www.rcoa.ac.uk, published November 2021
- Benign prostatic hyperplasia. BMJ Best Practice. bestpractice.bmj.com, last reviewed October 2022
- Personal communication. Mr Aziz Gulamhusein. Consultant Urologist and Robotic Surgeon. November 2022

