Gynaecological laparoscopy
Your health expert: Dr Madhavi Vellayan, Consultant Gynaecologist
Content editor review by Pippa Coulter, September 2022
Next review due, September 2025
A gynaecological laparoscopy is a procedure to look inside your pelvis (lower abdomen or tummy). It allows your surgeon to examine your womb (uterus), fallopian tubes and ovaries. Gynaecological laparoscopy can help to diagnose conditions and also to treat them where possible.
About gynaecological laparoscopy
A laparoscopy is also called keyhole surgery. It means a surgeon performs the procedure through small cuts (incisions) in your tummy. It can be a safer alternative to open surgery, which involves having a larger cut to open up your tummy. It’s usually associated with fewer complications and a shorter recovery time.
You may have a gynaecological laparoscopy to investigate certain symptoms, such as pain in your pelvis. You may have other tests, such as an ultrasound, magnetic resonance imaging (MRI) or computer tomography (CT) scan first. You may also have a gynaecological laparoscopy to treat a condition. Examples of when you may have one include:
- diagnosing and treating endometriosis
- removing scar tissue (adhesions)
- treating an ectopic pregnancy
- performing a sterilisation, which means sealing or blocking your fallopian tubes so that you can no longer get pregnant
- diagnosing and removing an ovarian cyst
- removing your womb (hysterectomy) or ovaries (oophorectomy)
- treating fibroids
- investigating long-term pain in your pelvis
- if you’re having fertility problems, it’s sometimes used to look for reasons why you might not be getting pregnant
- investigating whether you may have cancer or whether cancer has spread
Your doctor will explain why they’re recommending a gynaecological laparoscopy, and will talk about the benefits and potential risks involved. They will discuss with you what will happen before, during and after your procedure, including any pain you might have. If you’re unsure about anything, don’t be afraid to ask. You’ll be asked to sign a consent form before the procedure, so it’s important that you feel fully informed.
Preparing for a gynaecological laparoscopy
A specialist doctor called a gynaecologist will usually carry out your gynaecological laparoscopy. Your hospital will give you information explaining how to prepare for your procedure.
If you’re having a gynaecological laparoscopy to diagnose a condition, you’ll usually have the procedure and go home the same day. If you are having the procedure to treat a condition, you’re still likely to be able to go home the same day. But sometimes you may need to stay in hospital overnight, so be prepared for this. Your doctor will let you know if this may be necessary. If you go home the same day, you’ll need someone to drive you and stay with you overnight.
A gynaecological laparoscopy is usually done under general anaesthesia, which means you’ll be asleep during the procedure. A general anaesthetic can make you sick, so you’ll need to stop eating and drinking around six hours before your procedure. You can usually drink water up to two hours before your procedure, but check any fasting instructions with your hospital.
At the hospital, a nurse will test your urine (pee) to check that you’re not pregnant or have any conditions that could cause complications.
You may be asked to wear compression stockings to help prevent blood clots forming in the veins in your legs (deep vein thrombosis). You may need an injection of an anticlotting medicine, as well as wearing compression stockings for procedures that are likely to take longer.
Gynaecological laparoscopy procedure
Gynaecological laparoscopy usually takes about half an hour to an hour if you’re having it to diagnose a condition. It will take longer if your doctor needs to treat a condition.
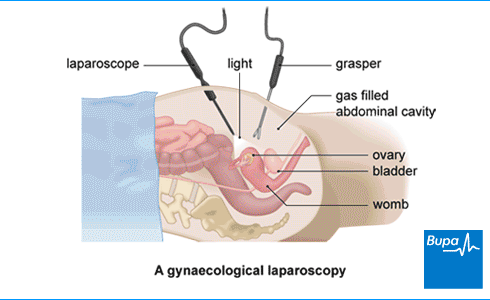
Your doctor will first make a small cut in your lower tummy, usually in or near your tummy button (navel). They’ll then put a needle through this cut and pass carbon dioxide through to gently inflate your tummy. This allows your surgeon to see better and have room to move the instruments around.
Next, your doctor will insert a laparoscope through the same cut, to see inside your tummy. A laparoscope is a small tube with a camera and a light on the end. The camera on the laparoscope sends video images of the inside of your tummy to a monitor where your doctor can see it. Your doctor will then make one or more additional small cuts in your tummy to pass through any instruments needed for your procedure.
At the end of the procedure, your doctor will release the carbon dioxide gas from your tummy. They will close the cuts in your skin with stitches or glue.
Aftercare for gynaecological laparoscopy
You’ll need to rest until the effects of the anaesthetic have passed. You might have some discomfort as the anaesthetic wears off but you'll be offered pain relief.
If you’ve had a laparoscopy for diagnosis, you’ll usually be able to go home after a few hours – as soon as you feel ready. You’ll need someone to take you home, and to stay with you for the first 24 hours while the anaesthetic wears off. If you’ve had treatment as part of your laparoscopy, your medical team may sometimes ask you to stay in hospital overnight. Before you go home, your nurse will give you advice about caring for your wounds. You may be given a date for a follow-up appointment.
Having a general anaesthetic can affect how you feel for the first 24 hours. You might find that you're not so coordinated or that it's difficult to think clearly. This should pass within 24 hours. In the meantime, don't drive, drink alcohol, operate machinery or make any important decisions.
Your stitches may dissolve on their own. If you have non-dissolvable stitches, you’ll need to have them taken out, usually after about five to seven days. A practice nurse at your GP surgery should be able to do this for you.
Recovery after gynaecological laparoscopy
It’s important to rest and take it easy for the first couple of days after a laparoscopy. You can start getting back to your usual activities as soon as you feel able. But build up the amount you do slowly.
Gynaecological laparoscopy recovery time depends on the type of surgery you’re having. If you’ve had a laparoscopy to diagnose a condition or for a minor procedure, you should be back to your usual activities within about three days. If you’ve had a more complicated procedure, it may take up to two or three weeks to feel like you’re back to normal.
You might have some pain and discomfort for a few days after your procedure. Your hospital may give you painkillers to take home, or you can take over-the-counter painkillers, such as paracetamol or ibuprofen.
You may also have some spotting or bleeding from your vagina for a few days. You can use sanitary pads until the bleeding stops.
Moving around as much as you can after your laparoscopy will help prevent blood clots forming in your legs. Even when you’re resting, moving your feet and legs around will help. Your doctor may also suggest you wear compression stockings or have blood thinning injections for a while after your operation. These help to prevent blood clots too.
You shouldn’t drive until at least 24 hours after your general anaesthetic. You should only drive once you’re able to manoeuvre your car safely and comfortably, without causing any discomfort or pain. Check with your own insurance company whether they have their own conditions.
You should be able to have sex as soon as you feel ready.
Side-effects of gynaecological laparoscopy
Side-effects are the unwanted but mostly temporary effects that you may get after having a gynaecological laparoscopy. Possible side-effects of a gynaecological laparoscopy include:
- a small amount of bleeding from your vagina
- pain and discomfort in your tummy
- pain in your shoulder – this is thought to be caused by the gas used to inflate your tummy irritating a nerve
- feeling more tired than usual
- bruises around your wounds
Complications of gynaecological laparoscopy
Complications are when problems occur during or after your procedure. Complications of laparoscopy in gynaecology include the following.
- Infection of a wound. This may cause sore, red skin around your scars.
- Urine infection. You may have a burning or stinging feeling when you pee, or you may need to pee more often.
- Hernia (bulging of tissue) near your wound. This causes a bulge under your skin. It can happen when a wound hasn't healed properly and tissue slips through the layers.
- Damage to organs in your tummy, such as your bowel, bladder, womb or major blood vessels. Worsening pain in your tummy can be a sign.
- Deep vein thrombosis (DVT) – a blood clot in a vein in your lower leg. This may cause your leg to become red, swollen and painful. It can be dangerous if it travels to your lungs.
You should seek medical help if you think you may have any of these complications.
The risk of serious complications is low for most people having a gynaecological laparoscopy. But there are some factors that can increase your risk. These include if you:
- are obese
- are older
- have had surgery on your tummy before
- have a long-term health condition
Your doctor will explain how these factors may affect you, and any special measures they can take to reduce your risk.
If you develop a complication during your laparoscopy, your doctor may need to convert from a keyhole procedure to open surgery. This means making a bigger cut in your tummy so they can identify the problem and treat it. It’s also important to understand that the laparoscopy may not always identify a clear reason for any symptoms you’re having, such as pelvic pain.
Worried about your Period health?
A personalised care plan for heavy, painful or irregular periods for those 18 and over. Now available.
To book or to make an enquiry, call us on 0333 920 0881∧
It depends on the type of procedure you are having. If you’re having a laparoscopy to investigate symptoms, it can be a relatively minor procedure. But if you’re having more complex surgery, like a hysterectomy, it can still be a major procedure. Your doctor will explain what to expect from the procedure and your recovery.
A simple gynaecological laparoscopy to look inside your pelvis may take as little as half an hour. If your doctor needs to treat a condition, it can take much longer. For more information, see our section on Gynaecological laparoscopy procedure.
You may have some bleeding from your vagina, like a period, for a few days after a gynaecological laparoscopy. You can use sanitary pads until the bleeding stops. If you have bleeding that continues or gets worse, seek medical advice. For more information see Side-effects of gynaecological laparoscopy.
A gynaecological laparoscopy can help with diagnosing several conditions. These include endometriosis, ovarian cysts, fertility problems and cancer. Sometimes, a laparoscopy may not show up any reasons for your symptoms. Your doctor may then suggest further tests or treatment. See our About section for more information.
A gynaecological laparoscopy is usually done under general anaesthesia, which means you’ll be asleep during the procedure and won’t feel anything. You might have some pain and discomfort for a few days afterwards. You can take painkillers to manage this if you need to. See our Recovery section for more information.
Hysterectomy
Hysteroscopy
Did our Gynaecological laparoscopy information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Laparoscopy recovering well patient information leaflet. Royal College of Obstetricians & Gynaecologists. www.rcog.org.uk, accessed 5 September 2022
- Diagnostic laparoscopy. Consent advice No. 2. Royal College of Obstetricians & Gynaecologists. www.rcog.org.uk, published June 2017
- Gynecologic laparoscopy. Medscape. emedicine.medscape.com, updated 12 September 2018
- Endometriosis: diagnosis and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 6 September 2017
- Ovarian cysts. BMJ Best Practice. bestpractice.bmj.com, last reviewed 6 August 2022
- General surgery. Oxford handbook of operative surgery. Oxford Academic. academic.oup.com, published May 2017
- Kaloo P, Armstrong S, Kaloo C, et al. Interventions to reduce shoulder pain following gynaecological laparoscopic procedures. Cochrane Database of Systematic Reviews 2019, Issue 1. Art. No.: CD011101. DOI: 10.1002/14651858.CD011101.pub2
- Laparoscopy. Encyclopaedia Britannica. www.britannica.com, accessed 5 September 2022
- Caring for someone recovering from a general anaesthetic or sedation. Royal College of Anaesthetists. www.rcoa.ac.uk, published November 2021
- You and your anaesthetic. Royal College of Anaesthetists. www.rcoa.ac.uk, published February 2020
- Small bowel obstruction. BMJ Best Practice. bestpractice.bmj.com, last reviewed 6 August 2022
- Ectopic pregnancy and miscarriage: diagnosis and initial management. National Institute of Health and Care Excellence (NICE). www.nice.org.uk, last updated 24 November 2021
- Sterilisation. Sexwise. www.sexwise.org.uk, last updated August 2018
- Hysterectomy. Medscape. emedicine.medscape.com, last updated 3 May 2021
- Lawson AA, Rentea RM. Oophorectomy. StatPearls Publishing. www.ncbi.nlm.nih.gov, last updated 8 May 2022
- Uterine fibroids. BMJ Best Practice. bestpractice.bmj.com, last reviewed 6 August 2022
- Chronic pelvic pain in women. BMJ Best Practice. bestpractice.bmj.com, last reviewed 6 August 2022
- Fertility problems: assessment and treatment. National Institute for Health and Care Excellence. www.nice.org.uk, last updated 6 September 2017
- Personal communication, Dr Madhavi Vellayan, Consultant Gynaecologist, 22 September 2022
- Surgical wounds – principles of wound management. Oxford handbook of adult nursing. Oxford Academic. academic.oup.com, published online June 2018

