Lung cancer
Your health expert: Dr Sunil Skaria, Consultant Oncologist
Content editor review by Rachael Mayfield-Blake, September 2022
Next review due September 2025
Lung cancer is the third most common cancer in the UK. It can cause a persistent cough, breathlessness and weight loss. Most cases of lung cancer are caused by smoking.
What is lung cancer?
You may get lung cancer if cells in your lungs grow in an uncontrolled way. The cells usually form a lump (tumour).
Your lungs move oxygen from the air you breathe into your blood and remove carbon dioxide as you breathe out. They’re made up of lots of air tubes (called bronchioles) and air sacs (called alveoli).
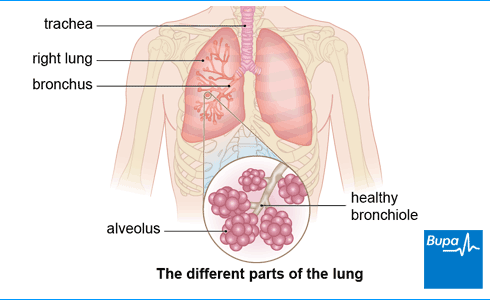
You have different types of cell in the different parts of your lungs. This means you can get different types of lung cancer.
When a tumour starts in your lung, this is called primary lung cancer. Sometimes cancer spreads to your lungs through your bloodstream or immune system from another part of your body, such as your kidney, breast or prostate. This is called secondary lung cancer.
Over 48,000 people are diagnosed with lung cancer each year in the UK.
Types of lung cancer
The two main types of cancer that start in the lung are non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). These names come from how the cancer cells look under a microscope.
Non-small cell lung cancer
About 8 in every 10 primary lung cancers are NSCLC. There are three main types of NSCLC– adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
- Adenocarcinoma mainly affects the outer part of your lungs. Around 4 in every 10 people with NSCLC have adenocarcinoma. This is related to smoking and exposure to asbestos. But it’s also the type of lung cancer you’re most likely to get if you don’t smoke.
- Squamous cell carcinoma affects your main airways (your bronchi), usually near the centre of your lungs. Around 3 in every 10 people with NSCLC have this type of lung cancer.
- Large cell carcinoma can appear in any part of your lungs, but most often in the centre of your lungs. It affects about 1 in every 10 people with NSCLC.
Small cell lung cancer
Two in 10 people with lung cancer have SCLC. SCLC can arise quickly and spread to other parts of your body, often before it’s been diagnosed. SCLC is almost always caused by smoking.
Causes of lung cancer
Smoking (tobacco cigarettes) is the biggest cause of lung cancer and in the UK it causes between 7 and 9 in every 10 lung cancers. Your risk of lung cancer is related to how much you smoke, how long you’ve been smoking and when you started smoking. Passive or second-hand smoking (breathing in other people’s smoke) is also linked to lung cancer.
You may also be more likely to get lung cancer if you:
- are exposed to asbestos
- are exposed to high levels of radon gas – a naturally occurring radioactive gas
- have had lung disease such as tuberculosis (TB) or chronic obstructive pulmonary disease (COPD) in the past
- inherit certain genes that make you more susceptible to lung cancer
How cancer develops
Cancer explained | Watch in 1:48 minutes
In this video, we explain how, when cells divide uncontrollably, this leads to cancer.
Symptoms of lung cancer
Many people with lung cancer have no symptoms at first. Sometimes, the early symptoms can be very general – for example, a cough or feeling a bit out of breath. You may think these symptoms are caused by smoking or a much less serious condition such as asthma. Lung cancer is sometimes only discovered if you have a chest X-ray for some other reason.
Lung cancer can cause:
- a cough that doesn’t go away (lasts longer than 3 weeks) or changes in some way (it may get more painful or sound different)
- coughing up blood
- shortness of breath
- pain in your chest
- losing weight for no reason
- feeling very tired
- losing your appetite
Other symptoms of lung cancer include:
- swelling of your face or neck
- a hoarse voice
- regular chest infections
You may also notice a broadening or thickening of the tips of your fingers – this is called clubbing.
If you have any of these symptoms or signs, see a GP as soon as possible.
Diagnosis of lung cancer
Seeing your GP
A GP will ask you about your symptoms and medical history and whether or not you smoke. If you only have a cough, they may ask you to wait and see if it gets better on its own. This is most likely to happen if you’re younger, have never smoked or your cough started when you had a cold or flu.
If your GP thinks your symptoms could be caused by lung cancer, they will refer you for a chest X-ray or a scan. You may have an urgent clinic referral if you’re over 40 and you smoke or have smoked in the past.
Referral to a specialist
If your chest X-ray shows signs of lung cancer, a GP will refer you to a doctor who specialises in chest disease. Sometimes, they may refer you even if your X-ray seems normal or before you have any X-rays.
The specialist will ask you to have some tests to confirm whether or not you have lung cancer. If you do have cancer, the tests can show which type of cancer you have, how advanced it is, and if it’s spread (metastasised). This is called cancer staging.
These tests may include the following.
- A CT scan of your chest and tummy. This uses X-rays to make three-dimensional (3D) images of part of your body. This is usually the first test you’ll have after a chest X-ray.
- A PET-CT (positron emission tomography) scan. You may be offered this type of CT scan if you have early-stage cancer. It helps doctors to see where your cancer is and if the cancer has spread.
- A bronchoscopy. This test lets your doctor look inside your lungs and take a sample of tissue (a biopsy). A bronchoscope is a narrow, tube-like, flexible telescopic camera. You’ll be given an anaesthetic spray and some medicine to make you sleepy before the doctor passes the bronchoscope down your windpipe into your lungs. Or you may have a general anaesthetic and be asleep during the test.
- A needle biopsy through the skin of your chest. This is called a percutaneous lung biopsy. Your doctor will numb your skin with a local anaesthetic then insert a fine needle. They’ll use an ultrasound or CT scan to guide the needle into the right place.
Looking for cancer cover that supports you every step of the way?
If you develop new conditions in the future, you can rest assured that our health insurance comes with full cancer cover as standard.
To get a quote or to make an enquiry, call us on 0808 273 6216∧
Treatment of lung cancer
Treatment for lung cancer will depend on which type of cancer you have, the stage of the cancer, and your general health. The stage of cancer is how big it is and if it has spread. The tests you have to diagnose your cancer (see our section on diagnosis of cancer) give some information about the stage. This information can help your doctor decide which treatment you need.
Lung cancer can be difficult to cure because it may have already spread by the time you’re diagnosed.
Non-small cell lung cancer
Non-small cell lung cancer (NSCLC) that’s at an early stage and hasn’t spread is usually treated with surgery or radiotherapy first. This may cure some types of NSCLC. Surgery may be followed by chemotherapy . If the cancer has already spread (metastasised), you may be offered treatments such as chemotherapy, radiotherapy, immunotherapy or targeted therapy.
Small cell lung cancer (SCLC)
Small cell lung cancer (SCLC) is usually treated with chemotherapy and radiotherapy rather than with surgery. This is because the cancer has often spread by the time it’s diagnosed.
If it isn’t possible to cure your cancer, your treatment will aim to extend your life and improve your quality of life as much as possible. This is called palliative care.
Surgery
Your surgeon may remove a small section of lung, part of a lung or a whole lung, depending on the size, type and position of your cancer.
Whether or not you’re offered surgery will depend on how healthy your lungs are. If you smoke, it’s best to stop smoking before your operation because this will help you to recover better afterwards. Before surgery, your doctor may give you some advice on how to get yourself as fit as possible so you’re ready for your operation.
Non-surgical treatments
Radiotherapy uses radiation to destroy cancer cells. Your doctor will target a beam of radiation onto the area of your lung with the cancer to shrink the tumour.
Chemotherapy uses medicines to destroy cancer cells. You may have chemotherapy on its own, after surgery or with radiotherapy. Chemotherapy is usually given as an injection or through a drip.
Targeted therapies are medicines that can block messages in your cancer cells to stop them growing and dividing. You may be offered targeted therapy if you have a particular type of NSCLC.
Immunotherapy is another type of cancer treatment, which helps your immune system to attack cancer cells. A number of immunotherapy drugs are now available to treat advanced NSCLC.
All lung cancer treatments can help to manage your cancer, but they can also cause side-effects. Your doctors and nurses will give you information about the treatments. This will help you decide which treatment is right for you and what to expect.
Prevention of lung cancer
The most important thing you can do to reduce your risk of developing lung cancer is to stop smoking. Speak to your local pharmacist or GP about the best ways to give up smoking. Nicotine replacement therapy (such as gums or patches) can help you quit. Vaping may be an option for you to consider, although quitting completely is best.
Try to avoid second-hand smoke – keep away from enclosed spaces where other people are smoking. Try to avoid exposing yourself to anything that could increase your risk of lung cancer – this includes asbestos and radiation.
There’s some evidence that eating fruit and vegetables can help to reduce your risk of getting lung cancer. So try to eat a balanced diet. Research suggests that taking vitamin supplements doesn’t seem to have any effect on the risk of lung cancer and possibly may be harmful.
Being more physically active may help to reduce your chance of getting several cancers.
Living with lung cancer
A diagnosis of cancer can be distressing for you and your loved ones. An important part of cancer treatment is getting enough support to deal with the emotional aspects as well as the physical symptoms.
You should have a lung cancer clinical nurse specialist assigned to you as soon as you’ve been diagnosed. This person will coordinate your care. A range of doctors and nurses will help to support you through your treatment and help you to make decisions about the type of treatment you’d like. They can prescribe medicines and offer practical advice to deal with symptoms such as pain, exhaustion, coughing and depression.
Your hospital should also offer a range of helpful services, including dietitians, counsellors, complementary therapists and benefits advisers. Voluntary groups and patient organisations such as Macmillan nurses and Marie Curie nursing and day centres are also available.
If you have more advanced cancer, you can get support through hospices or at home. Your doctor will discuss this with you.
Ask your cancer specialist about any new cancer treatments you see in the news. They may be in the experimental stages and you might be able to join a local clinical trial. Your cancer specialist can tell you if you’re right for the trial and if the treatment being tested could be right for you. You can find out more about clinical trials happening near you on the Cancer Research UK website.
Effects of smoking
Did our Lung cancer information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Respiratory medicine. Oxford handbook of general practice. Oxford Medicine Online. oxfordmedicine.com, published online June 2020
- Lung cancer statistics. Cancer Research UK. www.cancerresearchuk.org, accessed 22 July 2022
- Lung and pleural cancers – recognition and referral. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised February 2021
- Lung anatomy. Medscape. emedicine.medscape.com, updated 7 December 2017
- Lung tumours. Oxford handbook of clinical medicine. Oxford Medicine Online. oxfordmedicine.com, published online September 2017
- What is lung cancer? Cancer Research UK. www.cancerresearchuk.org, last reviewed 11 September 2019
- What is secondary lung cancer? Cancer Research UK. www.cancerresearchuk.org, last reviewed 20 March 2020
- Lung carcinoma. MSD Manuals. www.msdmanuals.com, last full review/revision July 2020
- Types of lung cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 28 January 2020
- Non-small cell lung cancer. BMJ Best Practice. bestpractice.bmj.com, last reviewed 25 June 2022
- Non-small cell lung cancer (NSCLC). Medscape. emedicine.medscape.com, updated 20 May 2022
- Small cell lung cancer. BMJ Best Practice. bestpractice.bmj.com, last reviewed 25 June 2022
- Thoracic malignancies. Oxford handbook of oncology. Oxford Medicine Online. oxfordmedicine.com, published online October 2018
- Lung cancer symptoms. Cancer Research UK. www.cancerresearchuk.org, last reviewed 12 September 2019
- Cough (acute): antimicrobial prescribing. National Institute for Health and Care Excellence (NICE). nice.org.uk, published 7 February 2019
- Lung cancer: diagnosis and management. National Institute for Health and Care Excellence (NICE). nice.org.uk, published 28 March 2019
- Lung cancer in adults. National Institute for Health and Care Excellence (NICE). nice.org.uk, last updated 13 December 2019
- PET-CT scan for lung cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 10 October 2019
- Bronchoscopy for lung cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 3 October 2019
- Biopsy through the skin for lung cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 2 October 2019
- General principles of radiation therapy. Medscape. emedicine.medscape.com, updated 24 February 2022
- Chemotherapy treatment for lung cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 30 October 2019
- Immunotherapy and targeted cancer drugs for non-small cell lung cancer (NSCLC). Cancer Research UK. www.cancerresearchuk.org, last reviewed 10 January 2020
- Tepotinib for treating advanced non-small-cell lung cancer with met gene alterations. National Institute for Health and Care Excellence (NICE). nice.org.uk, published 18 May 2022
- Sotorasib for previously treated KRAS G12C mutation-positive advanced non-small-cell lung cancer. National Institute for Health and Care Excellence (NICE). nice.org.uk, published 30 March 2022
- Treatment for lung cancer. National Institute for Health and Care Excellence (NICE). nice.org.uk, accessed 28 July 2022
- Tobacco: preventing uptake, promoting quitting and treating dependence. National Institute for Health and Care Excellence (NICE). nice.org.uk, published 30 November 2021
- Research and analysis. Nicotine vaping in England: 2022 evidence update main findings. GOV.UK. gov.uk, published 29 September 2022
- UK Chief Medical Officers' physical activity guidelines. GOV.UK. gov.uk, last updated 16 February 2022
- Coping with lung cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 14 November 2019
- Support at home for you and your family. Cancer Research UK. www.cancerresearchuk.org, last reviewed 29 June 2021
- Palliative care. Patient. patient.info, last edited 29 January 2019
- How to join a clinical trial. Cancer Research UK. www.cancerresearchuk.org, last reviewed 1 February 2022
- After lung cancer surgery. Cancer Research UK. www.cancerresearchuk.org, last reviewed 24 October 2019

