Anal fissure
Your health expert: Mrs Sara Badvie, Consultant Laparoscopic, Colorectal and General Surgeon
Content editor review by Liz Woolf, Freelance Health Editor, August 2023
Next review due August 2026
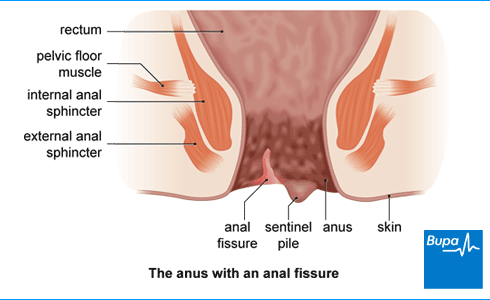
An anal fissure is a small tear or open sore (ulcer) in the skin just inside your anus (bottom or back passage). It causes severe pain and sometimes bleeding when you have a bowel movement (poo). Anal fissures often go away by themselves, especially with some simple self-help measures. But if they don’t, there are treatments that can help.
About anal fissure
Anal fissures develop in the skin lining your back passage, just inside your anus (your anal canal). They usually develop towards the back of your anus. But you can sometimes get one at the front or even both together. Some conditions can cause anal fissures – for example, Crohn’s disease. If you have this condition, you may get fissures anywhere around your anus.
If you’ve had an anal fissure for less than six weeks, it’s called an acute anal fissure. If it lasts for longer than six weeks, it’s known as a chronic anal fissure.
Anal fissures are common. It’s thought that around one in 10 people get one at some point in their life. Anyone, including children, can get an anal fissure but it’s most common in people aged 15 to 40.
Causes of anal fissure
For most people, there isn’t any obvious reason why they develop an anal fissure. This is called a primary anal fissure. It’s often thought to be caused by hard or painful bowel movements. These can cause the muscles around your anus (the internal sphincter muscles) to tense up and spasm. This makes your anus more likely to tear. It also reduces the blood supply to the area, which makes it harder for any tears to heal.
Sometimes, there is a clear underlying cause for an anal fissure. This is known as a secondary anal fissure. Causes of secondary anal fissures include:
- constipation – a hard poo can cause a tear
- pregnancy or giving birth – this can put pressure on the area between the anus and vulva (your perineum)
- inflammatory bowel disease such as Crohn’s disease
- a sexually transmitted infection or a skin infection
- a skin condition such as psoriasis
- medicines that are constipating such as opioid painkillers or some chemotherapy drugs
- trauma to your anus – for example, through having anal sex or through surgery
- bowel cancer
Symptoms of anal fissure
With an anal fissure, you may feel a tearing sensation when you poo. Once you have a tear in your anus, it can cause pain whenever you poo. This may be sharp, searing, or burning pain in or around your bottom. Some people describe this as feeling like ‘passing broken glass’. You may continue to feel a deep, burning pain for several hours afterwards.
Not everyone has bleeding with an anal fissure. But if you do, you might see blood in the toilet bowl or on the toilet paper after you’ve had a poo.
You may also have spasms (sudden tightening) in the muscles around your anus when you poo.
These symptoms may not always be due to an anal fissure. Other conditions, like piles (haemorrhoids) can cause similar symptoms. If you have any of the symptoms above, contact your GP for advice. It’s always important to seek medical advice if you notice bleeding from your bottom.
Diagnosis of anal fissure
Your GP will usually be able to diagnose an anal fissure by asking about your symptoms and examining you. They’ll ask you to describe your symptoms and how long you’ve had them. They may also ask you about your health in general and your medical history.
Your doctor will examine you by asking you to lie on your side with your knees bent towards your chest. They’ll then gently part your buttocks to examine the area and see if there’s a fissure.
If there’s any uncertainty about what’s causing your symptoms or if initial treatments don’t help, your GP may refer you to a colorectal surgeon. This is a surgeon who specialises in conditions affecting your bowel and back passage.
Looking for prompt access to quality care?
With our health insurance, if you develop new conditions in the future, you could get the help you need as quickly as possible, from treatment through to aftercare.
To get a quote or to make an enquiry, call us on 0808 273 6216∧
What should I do if I'm embarrassed to talk to my doctor?
Seeing a doctor when you're embarrassed | Watch in 2:08 minutes
Dr Naveen Puri talks about how to make it easier to see a doctor about a health issue when you are feeling embarrassed.
Hello, I am Dr Naveen Puri, I am one of the GPs within Bupa Health Clinics.
Today I want to speak to you about embarrassing problems you might have and what we can do if you attend one of our clinics.
I want you to know that many people feel embarrassed or concerned about speaking about certain things with their doctors, but I'm here to reassure you these are the kinds of things we deal with every day.
For me, looking at someone's bottom or their breasts or their genitalia is no different to looking at their nose or elbow.
And that's true for all doctors as we train for many years in these parts of the body and are very used to having these conversations with people just like you.
So what I would encourage you to do if you have any concerns from your perspective, be it a change in your bowel habit, be it a lump, a rash, a swelling. Something on your genitalia or a part of your body you're not particularly familiar with or feel uncomfortable discussing.
Please be assured your doctor has done it all before.
Some of the ways we find patients find it easier to speak to a doctor is to either tell the doctor you feel embarrassed up front. That way a doctor can make extra effort to make sure you feel comfortable.
Or some patients come to us with pieces of paper and will write the problem down and hand it to us. That way we can help with whatever is going on for you as well.
You may also find it helpful to ask for a specific doctor, someone you're familiar with in your practice. Or you might want to ask for a doctor of a specific gender, or background to your liking as well.
I'd also say, doctors do this every day so don't be alarmed if we ask you certain questions around your symptoms. It is purely so we can help you get the best outcome for your enquiry.
And then finally, feel free to use language that suits you as well. We don't expect you to know the medical words for things, or a name for your diagnosis. That's our job to find out for you.
So, take your time, see a doctor, and hopefully we can help put your mind at ease.
Self-help
Most anal fissures heal by themselves within six to eight weeks. There are a number of ways to help the fissure heal and to relieve your pain and discomfort.
Eating and drinking
Gradually increasing the fibre in your diet will help keep your poo soft and easier to pass. You should aim for up to 30g per day in total. You’ll need plenty of wholegrain foods, fruit, and vegetables. As well as more fruit and veg, try swapping white bread and pasta for wholegrain products, choose a high fibre breakfast cereal, and add beans or lentils to stews and curries.
You also need to make sure you’re drinking enough fluids. This is especially important if you’re increasing your fibre intake.
Staying regular
Because of the pain, you may tend to delay going for a poo. But make sure you go to the toilet as soon as you feel the need and try not to strain when you go. ‘Holding on’ and straining can make a fissure worse – this can be a common cycle in children.
Hygiene and comfort
Keeping the area clean and dry is important. This will help with healing and preventing infection. Sitting in a warm bath after you’ve had a bowel movement may help to relieve any pain.
You can also manage pain with over-the-counter painkillers such as paracetamol or ibuprofen. You can buy these without a prescription. Make sure you read the patient information leaflet in the packet.
Treatment of anal fissure
If your pain is particularly severe or your symptoms aren’t improving with self-help measures, there are a number of treatments your doctor may suggest.
Medicines
There are several different types of medicine that can help to relieve pain associated with an anal fissure or help the fissure to heal.
Laxatives or stool softeners
Ispaghula husk or lactulose can help if you’re constipated. These work by softening your poo and making it easier to pass. You can buy laxatives over the counter from a pharmacy without a prescription. A doctor will need to prescribe them if they are for a child.
Anaesthetic ointment
Your GP may prescribe an anaesthetic ointment (for example, lidocaine). Using this for a few days will help if you’ve been having extreme pain when you poo. You apply this ointment to your anus to help numb the area before you have a bowel movement.
Glyceryl trinitrate (GTN) ointment
Your doctor may also suggest an ointment containing glyceryl trinitrate (GTN). This helps to relax the sphincter muscles in your anus. Relaxing these muscles improves blood flow to the area, which helps the fissure to heal. Your GP may prescribe GTN ointment if you’ve had a fissure for more than a week and it isn’t getting better. You’ll need to keep using it for six to eight weeks to prevent your fissure from coming back. GTN sometimes causes headaches at first, but these usually stop in a few days. GTN ointment isn’t suitable for children or pregnant women.
Calcium-channel blockers
A cream containing calcium-channel blockers (for example, diltiazem cream) may help. Like GTN ointment, this medicine relaxes the muscles in your anus and improves blood flow to the area. It has fewer side-effects than GTN ointment. It is usually prescribed by a specialist colorectal surgeon. Your GP may refer you if you’re not able to tolerate GTN or if you have a chronic anal fissure.
Procedures to treat anal fissure
If other treatment options haven’t helped your anal fissure to heal or it keeps coming back, your GP may refer you to a colorectal surgeon. Your surgeon will talk to you about what other options they may recommend. These include the following.
- Botulinum toxin (Botox) injections into the sphincter muscle in your bottom. The aim is to temporarily relax this muscle so that your fissure can heal.
- Lateral internal sphincterotomy – a type of surgery that involves cutting the sphincter muscles in your anus. This releases the tension around your anus and lets your fissure heal
- Fissurectomy – cutting away the damaged skin around your anal fissure
- Anal advancement flaps – taking healthy skin from your anal lining and using it to replace the broken skin in your fissure.
There is more information about all these procedures in our page of information on anal fissure procedures.
Prevention of anal fissure
You can reduce your risk of developing an anal fissure by preventing constipation. This is really important if you’ve already had an anal fissure that’s healed because it can help to stop the fissure from coming back.
You can help to prevent constipation by making sure you have a healthy balanced diet that contains plenty of fibre. It’s also important to make sure you’re drinking enough fluids and exercising regularly.
If you have another health condition that increases your risk of getting an anal fissure, speak to your doctor. They will tell you the best way to manage your condition and reduce your risk of getting an anal fissure.
As your fissure is healing, you’ll start to notice your symptoms improving. Your pain should lessen and if you had any bleeding, this should stop too. You should have a follow-up appointment with your doctor after six to eight weeks. This is to check that the fissure has healed.
Most anal fissures heal within six to eight weeks. But they may heal more quickly or take longer than that. You can help by making changes to your diet and lifestyle and take medicines for pain relief. There is more information in our section on self-help for anal fissures.
Anal fissures often don’t have a specific cause. But they are often linked to constipation. You may be more likely to get one if you’re pregnant or have an inflammatory bowel condition. There is more information in our section on causes of anal fissure.
The main symptom of anal fissure is pain when having a poo (bowel movement). The pain can be severe and go on for some time afterwards. You may also have some bleeding. There is more information in our section on anal fissure symptoms.
It’s most important to prevent constipation if you have an anal fissure. You need to eat enough fibre, drink plenty of fluids and make sure you exercise daily. You can take over-the-counter painkillers to help with pain. For more advice, see our section on self-help for anal fissure.
Anal fissure procedures
If you have an anal fissure that hasn’t healed with other treatments, your doctor may suggest surgery.
Constipation
Constipation is a common condition that affects your usual pattern of bowel movements.
Why is fibre important?
Fibre is a plant-based carbohydrate found in foods such as wholegrains and vegetables, also described as roughage. Many of us don’t get enough fibre in our diets.
Piles
Did our Anal fissure information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Anal fissure. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised April 2021
- Anal fissure. BMJ Best Practice. bestpractice.bmj.com, last reviewed July 2023
- Anal fissure clinical presentation. Medscape. emedicine.medscape.com, last updated March 2023
- Anal fissure. Patient. patient.info, last updated October 2022
- Suspected cancer: recognition and referral. National Institute for Health and Care Excellence (NICE). nice.org.uk, last updated January 2021
- Fibre: food fact sheet. British Dietetic Association. www.bda.uk.com, published April 2021
- Oxford Handbook of General Practice (5th edit). Oxford Academic. academic.oup.com, published online June 2020
- Constipation in children. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised November 2020
- Colorectal Surgery (2nd edit). Oxford Academic. academic.oup.com, published online July 2021
- Anal fissure treatment & management. Medscape. emedicine.medscape.com, last updated March 2023
- Constipation in adults. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised January 2023

