Gum disease
- Dr Emma Ajimoko, Head of Clinical Policy and Standards at Bupa Dental Care
- Michelle Harrison, Freelance Health Editor
Gum disease is when your gums become red, swollen, and bleed when you brush. It’s usually caused by a build-up of plaque if you don’t clean your teeth properly. Without treatment, gum disease can spread to the bones that hold your teeth in place, making your teeth loose or fall out.
About gum disease
You might sometimes hear doctors and dentists refer to gum disease as periodontal disease. The word periodontal means ‘around the tooth’. It happens if bacteria around your teeth make your gums inflamed. This can lead to the loss of the gums, bones and other structures that support your teeth, and sometimes lead to infection.
There are two main types of gum disease, depending on how far your gum disease has progressed. If your gum disease is still in the early stages, it’s known as gingivitis. More advanced gum disease is called periodontitis.
You might not know you have gum disease, because it doesn’t always cause pain. So it’s important to visit your dentist for regular check-ups. There are lots of things you and your dentist can do to reverse or stop gum disease before it gets worse.
Types of gum disease
There are two main types of gum disease – gingivitis and periodontitis.
Gingivitis
Gingivitis is the mildest form of gum disease (gingiva is another word for gums). It happens if plaque builds up on your teeth and causes inflammation around your gums. You might notice that your gums are red and swollen or that you have bleeding gums when you brush or floss your teeth.
At this stage, gum disease hasn’t spread to your jawbone, so it can be reversed. You can usually get rid of gingivitis by brushing and flossing your teeth thoroughly to remove any plaque. A dental hygienist can also help by giving your teeth a professional clean.
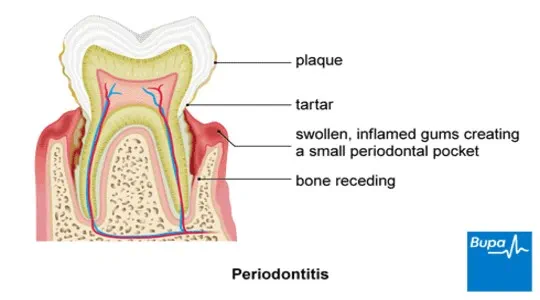
Periodontitis
When gingivitis is left untreated, the inflammation can spread to the ligaments and bones that hold your teeth in place. This is known as periodontitis. Your gums may begin to pull away from your teeth, leaving little pockets. These pockets trap plaque that you may not be able to reach with a toothbrush.
Over time, the plaque hardens to become tartar, which can irritate your gums even further by collecting more plaque. Tartar can’t be removed by brushing alone. The pockets may then become deeper and more difficult to clean, making the problem worse. Sometimes you may develop an infection in your gums and pus might collect under your gums, causing a painful abscess.
Without treatment, periodontitis can cause your gums to shrink back from your teeth (a process known as recession). This may then expose some of the roots of your teeth, making them feel sensitive. If you have any bone loss, your teeth may feel loose.
Although you can’t reverse periodontitis, your dentist can treat the condition and try and slow it down. But left untreated, your teeth can become wobbly and sometimes fall out.
What causes gum disease?
The main cause of gum disease is a build up of plaque on your teeth. Plaque is a sticky film of bacteria that forms on your teeth when you eat or drink. If you don’t remove plaque from your teeth properly by brushing and flossing, it hardens into tartar, irritates your gums and allows bacteria to spread.
There are also things that make you more likely to develop gum disease. These include:
- smoking
- getting older
- diabetes
- crooked teeth
- genetics
- taking medications that make your mouth dry
- stress
- obesity
- hormonal changes during pregnancy or menopause conditions that weaken your immune system –for example, cancer or HIV
Symptoms of gum disease
You might not know that you have gum disease but if you do, you might notice any of the following: .
- your gums bleed when you brush, floss or eat
- swollen, sore or inflamed gums
- pain when you chew
- a bad breath or taste in your mouth
- your gums have moved away from your teeth (receding gums)
- your teeth are looser
Diagnosis of gum disease
If you suspect you might have gum disease, make an appointment to see a dentist. They’ll be able to tell if you have gum disease with a few simple tests.
Your dentist will do a thorough examination of your mouth to check for signs of plaque, tartar, inflammation or bleeding. If you have any pockets around your gums, they’ll use a tiny ruler to measure how deep these are. Pockets bigger than 4mm may be a sign of more advanced gum disease.
Your dentist will ask about your medical history and lifestyle, to determine if there’s anything that could be causing gum disease, like smoking or medication.
The symptoms of periodontitis include:
Finally, your dentist might want to take dental x-rays of your mouth so they can see if there’s any bone loss inside your gums.
Sometimes, your dentist will refer you to a gum specialist called a periodontist for treatment. A periodontist is a dentist who specialises in treating gum disease.
How to treat gum disease
The type of treatment you need for gum disease will depend on how severe it is. Periodontal disease treatment aims to manage any existing gum disease and stop it from getting worse. Your dentist or periodontist might recommend the following.
Professional cleaning and better oral hygiene
If you have gingivitis (early stage gum disease), you might be able to reverse gum disease by getting rid of the bacteria before it spreads. Your dentist will recommend you have your teeth cleaned professionally by a dental hygienist and teach you how to clean your teeth properly at home. They’ll arrange regular check-ups to make sure your gums are getting better.
Professional mechanical plaque removal (PMPR)
If you have periodontitis, your dentist might suggest a deeper cleaning treatment called professional mechanical plaque removal (PMPR). This is when your dentist removes plaque and tartar (hardened plaque) from both above and below your gumline. It was previously known as scaling and root planing.
There are two main types of PMPR:
- Supragingival PMPR. This is when your dentist cleans the visible parts of your teeth, above your gumline.
- Subgingival PMPR. This aims to clean the roots of your teeth, that sit below your gumline.
PMPR may be carried out over several appointments and is sometimes done using a local anaesthetic so you don’t feel any pain.
Medication
If your gums are badly infected, your dentist might suggest treating the infection by:
- using a prescribed mouthwash
- taking antibiotics
- applying an antibiotic gel onto your gums
Gum surgery
If you have severe periodontal disease and other treatments haven't worked, your dentist may refer you to a periodontist for gum surgery. Surgery involves lifting your gums to remove tartar from deep pockets or reshaping damaged gum and bone tissue. Types of surgery for gum disease include flap surgery, bone grafts, and tissue regeneration to restore healthy gums and support your teeth.
How to prevent gum disease
The best way to prevent gum disease is to take good care of your teeth and gums to stop plaque from building up. This includes the following.
- See a dental hygienist to professionally remove plaque and tartar from your teeth and gums.
- Visit your dentist for regular check-ups.
- Brush your teeth twice a day with a fluoride toothpaste.
- Clean in between your teeth at least once a day with floss, an interdental brush or a water flosser.
- If you smoke, speak to your GP or pharmacist for advice and support giving up.
Dental hygiene
Dental check-ups
Healthy teeth for life
Tooth abscesses
Sensitive teeth
Other helpful websites

This information was published by Bupa's Dental Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Periodontal (gum) disease. National Institute of Dental and Craniofacial Research. nidcr.nih.gov, last reviewed August 2024
- Dental and periodontal diseases. Patient. patient.info/doctor, last updated June 2023
- About periodontal (gum) disease. Centers for Disease Control and Prevention. cdc.gov, published May 2024
- Gum disease. Oral Health Foundation. dentalhealth.org, accessed October 2024
- Periodontitis (pyorrhoea). MSD Manuals. msdmanuals.com last reviewed/revised April 2024
- PMPR. Periodontal Care (Scottish Dental Clinical Effectiveness Programme). periodontalcare.scdep.org.uk, accessed July 2025
- BSP UK clinical practice guidelines for the treatment of periodontal diseases. British Society of Periodontoloogy and Implant Dentistry www.bsperio.org.uk, published November 2023
![]()
Our information has been awarded the PIF tick for trustworthy health information.
^ We may record or monitor our calls.
Bupa Dental Care is a trading name of Oasis Dental Care Limited. Registered in England and Wales No: 00478127. Registered office: Bupa Dental Care, Vantage Office Park, Old Gloucester Road, Hambrook, Bristol, United Kingdom BS16 1GW.
Oasis Dental Care Limited has a number of trading names including Bupa Dental Care. Please see the list of our different trading names.


