Scoliosis
Your health experts: Adam Byrne, Senior MSK Physiotherapist, Bupa UK and Dr Ade Adeniyi, Bupa Clinics GP
Content editor review by Rachael Mayfield-Blake, March 2022
Next review due March 2025
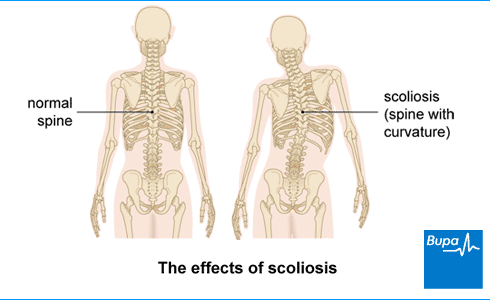
Scoliosis is when your spine permanently curves to the side at a noticeable angle, so your spine doesn’t look straight. It’s often called curvature of the spine and is most common in adolescents. You may need treatment to prevent the curve growing bigger but it may stop naturally, especially in young children.
Diagnosing idiopathic scoliosis
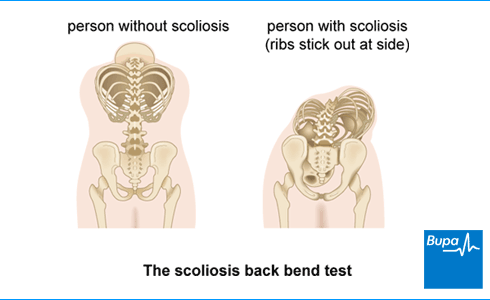
The back bend test for idiopathic scoliosis | Watch in 2 minutes
This video shows how a back bend test is done. This test can be used to help diagnose idiopathic scoliosis.
About scoliosis
Scoliosis means that your spine curves in an abnormal way (more than 10 degrees). For most people with scoliosis, their spine will curve in the lower back or chest, making a C or S shape. Your spine may also twist, which can pull on your rib cage and cause a hump.
Causes and types of scoliosis
There are different types of scoliosis, which relate to the age you first get it and the cause (if known).
Idiopathic scoliosis
Around eight in 10 people who have scoliosis have idiopathic scoliosis, which means the cause isn’t known. Idiopathic scoliosis most commonly develops between the ages of 10 and 18 and is called adolescent idiopathic scoliosis.
Mild scoliosis affects boys and girls equally but moderate-to-severe scoliosis is more common in girls. Scoliosis can be genetic – it often runs in families. The speed of growth, during teenage growth spurts, can affect how the spine curves, grows and develops. Once you stop growing, the curve doesn’t usually get any worse.
Congenital scoliosis
You can be born with abnormalities in the structure of your spine. This means your spine doesn’t form properly and is more likely to bend as you grow as a child. Because of the way a baby develops during pregnancy, problems with the spine can be linked to problems with other organs, such as the kidneys.
Syndromic scoliosis
Scoliosis can be part of a recognised syndrome (a condition with a group of common characteristics). People with Down syndrome often have musculoskeletal problems, which can include scoliosis. Marfan syndrome affects the body’s connective tissues and is likely to include scoliosis too.
Neuromuscular scoliosis
This type of scoliosis is caused by conditions that affect the nerves or muscles in your back. Examples include spina bifida and cerebral palsy. It's often worse if you can’t walk easily, or at all. If the curve continues to get worse, you’ll probably need scoliosis surgery.
Early-onset scoliosis
Early-onset scoliosis affects young children. It's known as infantile scoliosis in babies and children under three, and juvenile scoliosis if it develops between 3 and 10. It may be any of the types above. In infantile scoliosis, the spine usually curves to the left, from the chest area.
Adult degenerative scoliosis
If you had idiopathic scoliosis as a child, you may get it again because of wear and tear as you age. But normal wear of discs and joints may mean you get scoliosis for the first time as an older adult.
If you are developing a curvature of the spine, you may find it harder to stand up straight. You may also notice your ribcage, hip or waist sticking out. Adult scoliosis can be painful and cause shooting pain because of compressed nerves.
Other causes
If you damage your spinal cord at any age, it can increase your risk of scoliosis. This may be through an injury, infection, such as tuberculosis, or another health condition, such as osteoporosis.Symptoms of scoliosis
If you have scoliosis, one shoulder – often your right one – may look higher than the other. Your shoulder blade or ribs may stick out more. And your middle (waist) may seem off-centre because your hips are uneven. Clothes may not fit or hang as well as they should or did before.
Scoliosis may cause lower back pain that gets worse as the curvature of your spine increases. And it may hurt more after you’ve stood or sat down for a long time.
If you have adult degenerative scoliosis, you may have pain or pins and needles in your legs.
See your GP if you think you may have scoliosis.
Diagnosis of scoliosis
Your GP will ask about your medical history and your symptoms, and they’ll examine you. If you’re young, they’ll ask your parents if you’ve had any growth spurts.
If your GP thinks you have scoliosis and the curve is at least 10 degrees, they may refer you to a specialist doctor. This will be an orthopaedic specialist (a doctor who specialises in identifying and treating bone conditions). If you have a child who may have scoliosis, your GP will refer them to a paediatric orthopaedic specialist.
The orthopaedic specialist will ask you to do a back bend test. You bend forwards from your waist and this will show whether or not your shoulders, ribs, hips and waist are level, or if your ribs are more prominent on one side. Your specialist may use an instrument called a scoliometer, to measure the curve of your back.
The orthopaedic specialist may arrange further tests, including:
- x-rays
- an MRI (magnetic resonance imaging) scan – particularly if you’ve had muscle weakness or changes in sensation
These tests can help to identify the cause of a curved spine and the angle of the curve.
Treatment of scoliosis
Treatment of scoliosis will depend on your age, how severe the curve in your spine is, if it’s likely to get worse, and how it affects you. In many younger people, the scoliosis gets better on its own and they never need treatment.
The main aims of treatment are to slow or stop the curve progressing and to relieve or prevent symptoms and complications.
Bracing
A back brace for scoliosis is a type of corset that covers your upper body, from your armpits to your hips. Braces can only help children as you need to be still growing. They’re usually used for moderate severity scoliosis. A brace can stop the curve getting worse while your spine develops. It may also help to reduce the curve, particularly when combined with exercises for scoliosis.
Braces are made specifically to fit you and can be either rigid or flexible.
You may need to wear the brace every day for up to 23 hours until you stop growing. This can be difficult, particularly for children. But it’s thought that it’s more likely to help if you stick with it.
Casting
In babies and very young children, your specialist may suggest a cast, rather than a brace. This can help guide your child’s spine into a more normal position as they grow. Casts are made from plaster and worn all the time. As with a brace, they cover the upper body from the armpits to the hips. There are holes that allow the chest and stomach to expand so your child can eat and breathe properly. The plaster cast is put on while your child is under a general anaesthetic. It will need to be changed every three months as your child grows and their spine changes shape.
Other treatments
Regular exercise is usually part of the treatment of scoliosis because it improves core strength and fitness. This will help to keep your back and tummy (abdominal) muscles strong enough to support your spine. Your specialist doctor may refer you to have physiotherapy before you start any new sports or exercise.
Specialist physiotherapy exercises are recommended by physios as part of treatment for mild-and-moderate scoliosis, including during treatment with a brace. Exercises can also help with breathing difficulties related to the scoliosis.
You may decide to try complementary therapies alongside other treatment. Therapies such as Pilates and the Alexander technique can’t cure your scoliosis but may ease pain and improve your posture, mobility and balance. Talk to your doctor first about what’s right for you, and ideally make sure you have a specialist instructor or a physio who teaches Pilates as well, for example. Your curve may make it hard to do some of the exercises and you should stop if it hurts. Always find a qualified practitioner, ideally one who specialises in scoliosis.
If pain from adult scoliosis is having an impact on your everyday life, combined local anaesthetic and steroid injections into joints and nerves in your back may help.
Surgery
Although rare, your doctor may recommend surgery, which can stop the spine curving and reduce related problems. Whether it’s an option for you will depend on things like how bad the curve in your spine is and your age. An orthopaedic surgeon (a doctor who specialises in bone surgery) or spinal neurosurgeon (a doctor who specialises in conditions that affect your nervous system) will operate on you.
The most common type of surgery is called posterior instrumented correction and spinal fusion. In this procedure, your surgeon will connect metal implants and rods to bones in your spine (vertebrae) to correct the curve. These will hold the bones in place until they straighten and join together (fuse).
For children and adolescents, surgeons can use growth rods, which are extended every six months as they grow. Once you’re fully grown, your surgeon will usually remove the rods and you’ll have a spinal fusion operation. You may need to have more than one spinal fusion operation. This may be to extend the area of fusion further up or down your spine. This can be due to mechanical failure of the implants, which have to be replaced.
In older people with degenerative scoliosis, an operation to remove bone can free trapped nerves and relieve pain. This is called decompression. It’s sometimes combined with spinal fusion.
Complications of scoliosis
Complications of scoliosis include the following.
- If the curve of your spine restricts your lungs, it can cause breathing difficulties. This can happen to both adults and children, although it’s very rare in adolescent-onset scoliosis.
- You may get a hiatus hernia or other digestive problems because of the position of your stomach is different due to the position of your spine.
- In adults, scoliosis can cause problems walking.
If you get treatment for scoliosis early enough, you shouldn’t get these complications.
Prevention of scoliosis
You can’t prevent scoliosis but getting an early diagnosis and treatment may stop it from getting worse or even help to correct it.
There’s currently no screening programme for scoliosis in the UK. But the chances of developing scoliosis without yourself, family or friends noticing are very small. People usually spot it in themselves or in their children and see their GP. There’s no evidence that treating any earlier than that would be helpful. Doctors are also concerned that screening could lead to children having X-rays that they don’t need.
If you, or your child, is examined by a doctor for other reasons, they may detect early signs of scoliosis. Especially if you’ve already been diagnosed with a syndrome or condition linked to scoliosis.
Living with scoliosis
How scoliosis affects your daily life depends on the severity of the curve of your spine and the treatment you have.
Poor posture can cause pain and muscle weakness and change the way you move. But it’s difficult to have good posture if you have scoliosis. You may find you bend your knees and tilt your pelvis back to avoid leaning forwards or sideways. Instead, try to spread your weight evenly, keep your neck straight and try not to tilt your pelvis. Keep your hips as level as you can. It may help to look in a mirror to check your posture, or ask your family for help.
Scoliosis can also affect your body image and confidence. See the links in our Other helpful websites section for advice and support groups. It may help to share experiences with people going through the same thing.
Looking for physiotherapy?
You can access a range of treatments on a pay as you go basis, including physiotherapy.
To book or to make an enquiry, call us on 0370 218 6528∧
A number of things can cause scoliosis. You may be born with a problem with your spine. Or you may have another health condition that affects the nerves or muscles in your back and causes scoliosis, such as spina bifida. But for most people, the cause isn’t known.
See our section: Cause of scoliosis above for more information.
There isn’t a cure for scoliosis, but there are treatments that can help to slow or stop the curve in the spine progressing, and to relieve or prevent symptoms and complications. But most people with scoliosis don’t ever need treatment because the curve may stop naturally, especially in young children.
See our section: Treatment of scoliosis above for more information.
One shoulder, usually your right one – may look higher than the other, and it may stick out more. Your waist may seem off-centre because your hips are uneven. Some people get lower back pain. And adults with scoliosis may have pain or pins and needles in their legs.
See our section: Symptoms of scoliosis above for more information.
Scoliosis can sometimes cause problems. For example, if the curve of your spine restricts your lungs, it can make it difficult to breathe. And adults with scoliosis can have difficulties walking. But you can usually avoid these problems with early treatment.
See our section: Complications of scoliosis above for more information.
Osteoporosis
Physiotherapy
Benefits of exercise
Not only does regular exercise help you manage your weight and reduce your risk of developing diseases, it can help prevent and treat mental health problems
Did our Scoliosis information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Scoliosis and kyphosis. Patient. patient.info, last edited 23 August 2021
- Scoliosis. BNJ Best Practice. bestpractice.bmj.com, last reviewed 11 October 2021
- Scoliosis. Scoliosis Research Society. www.srs.org, accessed 11 November 2021
- What is congenital scoliosis? British Scoliosis Society. britscoliosis.org.uk, accessed 12 November 2021
- Down syndrome. Medscape. emedicine.medscape.com, updated 18 May 2020
- Marfan syndrome (MFS). Medscape. emedicine.medscape.com, updated 18 June 2020
- Neuromuscular scoliosis. Medscape. emedicine.medscape.com, updated 16 March 2021
- Infantile scoliosis. Medscape. emedicine.medscape.com, updated 1 November 2019
- Idiopathic scoliosis. MSD Manual Professional Version. www.msdmanuals.com, last full review/revision October 2020
- What is adult degenerative scoliosis? British Scoliosis Society. britscoliosis.org.uk, accessed 12 November 2021
- Developmental rheumatology in children. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised May 2019
- Musculoskeletal problems. Oxford handbook of general practice. Oxford Medicine Online. oxfordmedicine.com, published online June 2020
- Nonsurgical treatment options for scoliosis. American Academy of Orthopaedic Surgeons. orthoinfo.aaos.org, last reviewed September 2019
- Early onset scoliosis. Scoliosis Association UK. sauk.org.uk, accessed 12 November 2021
- What is early onset scoliosis? British Scoliosis Society. britscoliosis.org.uk, accessed 12 November 2021
- What is adolescent idiopathic scoliosis? British Scoliosis Society. britscoliosis.org.uk, accessed 12 November 2021
- Idiopathic scoliosis in children and adolescents. American Academy of Orthopaedic Surgeons. orthoinfo.aaos.org, last reviewed April 2021
- Complementary therapies. Scoliosis Association UK. sauk.org.uk, accessed 12 November 2021
- Negrini S, Donzelli S, Aulisa AG, et al. 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord 2018; 13:3. doi: 10.1186/s13013-017-0145-8
- Hiatus hernia. Patient. patient.info, last edited 14 April 2020
- Evidence map: Screening for adolescent idiopathic scoliosis. UK National Screening Committee. view-health-screening-recommendations.service.gov.uk, published March 2021
- Posture and positioning. Scoliosis Association UK. sauk.org.uk, accessed 12 November 2021
- Living with scoliosis. Scoliosis Research Society. www.srs.org, accessed 12 November 2021

