Hiatus hernia
- Mr Peter Lamb, Consultant Upper Gastrointestinal and General Surgeon
- Pippa Coulter, Freelance Health Editor
Key points
- A hiatus hernia happens when part of your stomach moves upwards into your chest.
- Hiatus hernia can cause symptoms like heartburn, but many people don’t have any symptoms.
- Risk factors for hiatus hernia include older age and conditions such as obesity and pregnancy.
- Treatment for hiatus hernia may not be needed, but it can include lifestyle changes, medications, or surgery.
What is hiatus hernia?
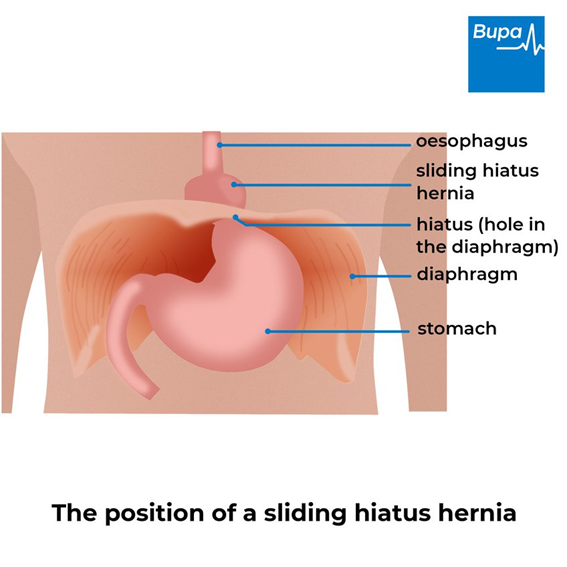
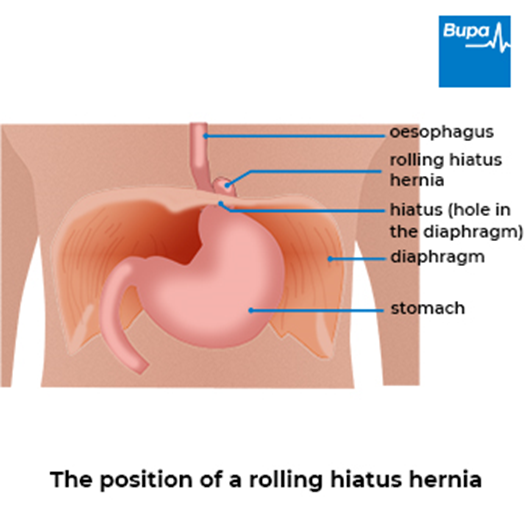
A hiatus hernia (sometimes called a hiatal hernia) is when part of your stomach slides upwards into your chest. Usually, your stomach sits completely below a sheet of muscle, called your diaphragm. This separates your chest from your abdomen (tummy). There’s an opening (‘hiatus’) in your diaphragm to let through a tube called your oesophagus. Your oesophagus carries food from your mouth to your stomach.
There are two main types of hiatus hernia: sliding hiatus hernia and rolling hiatus hernia. You can also have a mixed hiatus hernia, which is a combination of these types.
You don’t always need treatment for a hiatus hernia.
How a sliding hiatus hernia forms
How a hiatus hernia forms | Watch in 1:49 minutes
There are two types of hiatus hernia: sliding and rolling. This animation explains how a sliding hiatus hernia forms, which is the more common type.
Symptoms of hiatus hernia
Many people with a hiatus hernia don’t have any symptoms.
If you have a sliding hiatus hernia, you may develop gastro-oesophageal reflux disease (GORD). This is when acid from your stomach travels back up your food pipe (oesophagus). This can include indigestion symptoms such as:
- heartburn – a burning sensation in your chest
- reflux of stomach acid into your mouth – causing a sour taste
- feeling or being sick
- feeling bloated, or getting full quickly
- coughing or wheezing, or feeling short of breath
- pain in your chest or upper abdomen (tummy)
- finding it difficult or painful to swallow
When to seek help
You can usually manage symptoms of indigestion, like heartburn, yourself. A pharmacist can also advise you on this. But there are times when you should contact your GP. These include if your symptoms last longer than a few weeks, get worse, or if treatment isn’t working.
There are also some circumstances when you should seek urgent medical advice. These include if you are:
- having difficulty swallowing
- over 55 and have other symptoms – such as losing weight or blood in your vomit
Treatment of hiatus hernia
Treatment for hiatus hernia depends on how severe your symptoms are. There are things you can do to ease or prevent them. There are also medicines that may help with symptoms, and sometimes, surgery for hiatus hernia may be an option.
GP Subscriptions – Access a GP whenever you need one for less than £20 per month
You can’t predict when you might want to see a GP, but you can be ready for when you do. Our GP subscriptions are available to anyone over 18 and give you peace of mind, with 15-minute appointments when it suits you at no extra cost.
Self-help for hiatus hernia symptoms
There are several things you can do to ease or prevent the symptoms of a hiatus hernia. These include the following.
- If you’re obese or overweight, try to lose any excess weight.
- Avoid large meals. Aim for several smaller meals throughout the day.
- If heartburn bothers you at night, try raising the head of your bed. Don’t eat anything for at least three hours before you go to bed.
- Try to avoid things that raise the pressure inside your abdomen (tummy). This might include wearing tight clothing around your middle.
- If you smoke, try to stop, as smoking may trigger symptoms.
Which foods should I avoid if I have a hiatus hernia?
If you have symptoms such as heartburn caused by a hiatus hernia, you may find that avoiding certain foods helps prevent these. Common trigger foods include:
- fatty and spicy foods
- alcohol
- caffeine
A food and symptoms diary (PDF, 1.4MB) may help you identify foods that cause you problems.
Medicines
Certain medicines can trigger or worsen symptoms of hiatus hernia. Your doctor may suggest reducing or stopping the medicine if so. Don’t stop any medicines without advice from a doctor.
Your doctor may also recommend or prescribe indigestion medicines. These can help to ease your symptoms, but they won’t cure your hiatus hernia. These medicines include:
- antacids and alginates, which neutralise the acid in your stomach or form a barrier over it
- proton pump inhibitors (PPIs), which reduce the amount of acid your stomach produces
Surgery
There are certain circumstances when surgery for hiatus hernia may be an option. These include if:
- medicines aren’t controlling your symptoms or you need high doses to control your symptoms
- you can’t tolerate the side-effects of medicines
- you don’t want to take medicines long-term
- you have a rolling or a mixed hiatus hernia with symptoms
Your GP will need to refer you to a specialist surgeon to discuss whether surgery may be an option for you. The most common surgical treatment for a hiatus hernia is an operation called a fundoplication.
What can I take to ease hiatus hernia pain?
You can take over-the-counter indigestion medicines to manage symptoms such as heartburn. You can buy these from a shop or pharmacy, without a prescription from your doctor. But you should only take these for short periods of time. If you need something more, talk to your pharmacist or GP about other medicines that may help.
What happens if I don’t fix my hiatus hernia?
A hiatus hernia doesn’t always need to be fixed. You’ll usually only need treatment if it’s causing you symptoms. You can often manage hiatus hernia symptoms with lifestyle changes and medicines. If you don’t have surgery to fix the hiatus hernia, you might need to continue with these measures over the long term.
Types of hiatus hernia
There are two main types of hiatus hernia.
- Sliding hiatus hernia. The area where your oesophagus and stomach join is called the gastro-oesophageal junction. In this type, the gastro-oesophageal junction slides up into your chest first. The top part of your stomach then follows. Around 9 in 10 people with a hiatus hernia have this type.
- Rolling hiatus hernia (also called a para-oesophageal hiatus hernia). In this type, a different part of your stomach passes up into your chest to lie alongside your oesophagus. Your gastro-oesophageal junction stays in place below your diaphragm. Only around 1 in 10 people have this type.
You can also have a mixed hiatus hernia, which is a combination of these types.
It’s thought that up to half of adults have a hiatus hernia, so they’re very common.
Hiatus hernia causes
It’s not always clear exactly what causes a hiatus hernia. But there are certain factors that can make you more likely to develop one, including:
- older age – this is thought to be because the muscles in your diaphragm get weaker and less flexible as you get older
- anything that increases the pressure in your abdomen, such as obesity, pregnancy, a lung condition, long-term constipation, or ascites (build-up of fluid in your abdomen)
- previous surgery or injury to your abdomen or oesophagus
Diagnosis of hiatus hernia
To diagnose a hiatus hernia, a GP may:
- ask you about your symptoms and what could be triggering them
- examine you
- recommend tests to rule out other conditions or plan your treatment
- refer you to a doctor who specialises in conditions of the digestive system (a gastroenterologist)
If you have typical indigestion or GORD symptoms, you may not need tests to diagnose hiatus hernia.
Tests for hiatus hernia include the following.
- An endoscopy (also called a gastroscopy). This involves passing an endoscope (tube-like flexible camera) into your mouth or nose, and down into your stomach.
- Barium swallow and meal. In this test, you drink a fluid containing a substance called barium, which helps to show up your oesophagus and stomach on an X-ray.
- Oesophageal function tests. These look at how well your oesophagus is working and monitor any reflux you have. The test involves passing a fine tube (catheter) into your nose and down into your oesophagus. Your doctor may recommend this if you’re considering surgery.
Complications of hiatus hernia
There can be long-term complications associated with GORD due to a hiatus hernia. These include the following.
- Inflammation of your oesophagus (oesophagitis). Your oesophagus can become damaged by the acid from your stomach. This can lead to ulcers which may bleed.
- Anaemia caused by bleeding from an ulcer in your oesophagus.
- Narrowed oesophagus (a stricture). This is caused by scarring of your oesophagus from repeated inflammation. This can cause food to get stuck or to come back up.
- Aspiration pneumonia. This is when you breathe food or drink into your airways. It can then cause an infection in your lung.
- Barrett’s oesophagus. This is where the cells that line your oesophagus become damaged. Eventually, these cells may become cancerous.
Your doctor may suggest referral to an upper GI surgeon if you have signs of developing these complications.
If you have a larger rolling or mixed hernia, your stomach can turn and get twisted as it moves into your chest. This is called strangulation and results in the blood supply to your stomach being cut off, causing severe pain. This is an emergency and you’ll need urgent surgery to correct it.
Barrett's oesophagus
Barrett's oesophagus is when the cells that line the lower part of your oesophagus get damaged by acid and bile travelling upwards from your stomach.
Fundoplication
Fundoplication is an operation to treat gastro-oesophageal reflux disease (GORD) when it can’t be controlled with lifestyle changes and medicines.
Indigestion
Indigestion medicines can be used to relieve pain or discomfort in your upper abdomen (tummy) or chest that may occur soon after meals.
Indigestion medicines
This information is for you if you have indigestion and are considering seeing your doctor.
Did our Hiatus hernia information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Hiatus hernia. BMJ Best Practice. bestpractice.bmj.com, last reviewed 9 December 2022
- Hiatus hernia. Patient. patient.info, last edited 14 April 2020
- Smith RE, Shahjehan RD. Hiatal hernia. StatPearls Publishing, www.ncbi.nlm.nih.gov/books, last updated 22 August 2022
- Abdominal cavity. Encyclopaedia Britannica. www.britannica.com, accessed 9 January 2023
- Dyspepsia – proven GORD. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised October 2022
- Conditions for which over the counter items should not routinely be prescribed in primary care: Guidance for CCGs. NHS England. www.england.nhs.uk, published 29 March 2018
- Indigestion. Guts UK! gutscharity.org.uk, accessed 10 January 2022
- Dyspepsia and gastro‑oesophageal reflux disease in adults. Quality standard. National Institute for Health and Care Excellence. www.nice.org.uk, published 23 July 2015
- Gastro-oesophageal reflux disease and dyspepsia in adults: investigation and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 18 October 2019
- Dyspepsia – unidentified cause. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised July 2022
- Roman S, Kahrilas P. The diagnosis and management of hiatus hernia. BMJ 2014; 349:g6154. doi: 10.1136/bmj.g6154
- Sfara A, Dumitrascu DL. The management of hiatal hernia: an update on diagnosis and treatment. Med Pharm Rep 2019; 2(4):321–25. doi: 10.15386/mpr-1323
- Esophagogastroduodenoscopy (EGD). Medscape. emedicine.medscape.com, updated 4 February 2022
- JAG guidance: transnasal endoscopy. Royal College of Physicians. Joint Advisory Group on GI Endoscopy (JAG). www.thejag.org.uk, October 2018
- Barium meal. Macmillan Cancer Support. www.macmillan.org.uk, reviewed 30 April 2020
- Chen A, Tafti D, Tuma F. Barium swallow. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 7 September 2022
- Baldwin D, Puckett Y. Esophageal manometry. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 26 September 2022
- Electronic medicines compendium. www.medicines.org.uk, accessed 11 January 2023
- Salisbury BH, Terrell JM. Antacids. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 15 August 2022
- Leiman DA, Riff BP, Morgan S, et al. Alginate therapy is effective treatment for GERD symptoms: a systematic review and meta-analysis. Dis Esophagus 2017; 30(5):1–9. doi: 10.1093/dote/dow020
- Proton pump inhibitor. Encyclopaedia Britannica. www.britannica.com, accessed 4 September 2020



