Haemorrhoids (Piles)
- Mrs Sara Badvie, Consultant Laparoscopic, Colorectal and General Surgeon
What are haemorrhoids?
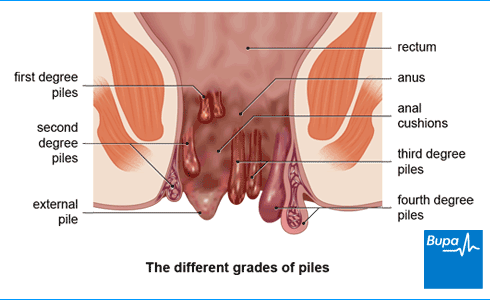
Haemorrhoids (piles) are enlarged blood vessels inside or around the opening of your bottom (anus). Your anus is lined with spongy tissue and blood vessels called the anal cushions. These help your anus to close. If the blood vessels in this area become enlarged, you might experience symptoms of piles.
How do I know if I have haemorrhoids (piles) – what do they look like?
Piles don’t always cause pain or other symptoms. But sometimes you might see blood on the toilet paper, drips in the toilet, or on the surface of your poo. You might be able to feel piles on your anus or hanging down from your anal canal too.
Are skin tags the same as piles?
No, skin tags aren't the same as piles. But you may get them if you have external piles (swellings that develop on the outside edge of your anus). Blood clots can sometimes form in external piles and this will stretch your skin over the area. As the pile heals, it will gradually shrink and leave behind a small tag of extra skin. You can also get skin tags without having piles or a blood clot.
Types of piles
The following are two main types of piles.
Internal piles
Internal piles start inside your anal canal (the short, muscular tube connecting your rectum with your anus). Internal piles can also hang down and come out your anus. They’re graded into four categories:
- First degree piles: these may bleed but don’t come out of your anus.
- Second degree piles: these come out of your anus when you have a poo, but go back inside afterwards.
- Third degree piles: these come out of your anus and only go back inside if you push them back in.
- Fourth degree piles: these always hang down from your anus and you can’t push them back in. They can become very swollen and painful if the blood inside them clots.
External piles
External piles are swellings that develop further down your anal canal, closer to your anus. They can be really painful, especially if they have a blood clot in them.
It’s possible to have both internal and external piles at the same time.
Causes of piles
Piles develop when the veins in your anal canal become swollen, which may happen for a number of reasons. These include if you:
- strain when you go to the toilet, for example if you have constipation
- anal canal weakens with age
- have a persistent cough
- lift heavy objects
Piles are also common during pregnancy. They may develop due to the higher pressure in your tummy (abdomen) when you’re pregnant. They usually get better after you give birth.
Symptoms of piles
Piles don’t always cause pain or other symptoms, but if you do have piles symptoms, they might include:
- bleeding when you poo – you may see blood (usually bright red) on the toilet paper, or drips in the toilet or on the surface of your poo
- a lump in or around your anus
- a slimy discharge of mucus from your anus, which may stain your underwear
- itchy, sore skin around your anus
- a feeling of ‘fullness’ and discomfort in your anus
- a feeling that your bowels haven’t completely emptied after you’ve gone to the toilet
- pain and discomfort after you go to the toilet
These symptoms can also be caused by conditions such as:
If you have any of these symptoms, contact a GP for advice.
Why does the skin around my anus get itchy?
The skin around your anus often gets itchy because of a slimy discharge of mucus that can come out from your anus. This may irritate your skin and cause you some discomfort. You may also find that poo occasionally leaks out too, which can make it worse. If you have skin tags, they can trap moisture near your skin and make it difficult to clean yourself properly after you go to the toilet. This can cause further itching and discomfort.
Diagnosis of piles
Your GP will ask about your symptoms and examine you. To do this they might:
- gently put their finger into your anus to feel your rectum – they’ll wear gloves and use some gel to make it more comfortable.
- look inside your rectum using a short, tube-like instrument called a proctoscope. They may refer you to a specialist doctor to do this.
You might need to have a blood test to check if you have anaemia if you have a lot of bleeding.
If your symptoms, examinations or test results suggest your symptoms might be caused by something else, your GP may refer you to hospital for more tests. These can rule out other conditions, such as bowel cancer.
GP Subscriptions – Access a GP whenever you need one for less than £20 per month
You can’t predict when you might want to see a GP, but you can be ready for when you do. Our GP subscriptions are available to anyone over 18 and give you peace of mind, with 15-minute appointments when it suits you at no extra cost.
What should I do if I'm embarrassed to talk to my doctor?
Seeing a doctor when you're embarrassed | Watch in 2:08 minutes
Dr Naveen Puri talks about how to make it easier to see a doctor about a health issue when you are feeling embarrassed.
Hello, I am Dr Naveen Puri, I am one of the GPs within Bupa Health Clinics.
Today I want to speak to you about embarrassing problems you might have and what we can do if you attend one of our clinics.
I want you to know that many people feel embarrassed or concerned about speaking about certain things with their doctors, but I'm here to reassure you these are the kinds of things we deal with every day.
For me, looking at someone's bottom or their breasts or their genitalia is no different to looking at their nose or elbow.
And that's true for all doctors as we train for many years in these parts of the body and are very used to having these conversations with people just like you.
So what I would encourage you to do if you have any concerns from your perspective, be it a change in your bowel habit, be it a lump, a rash, a swelling. Something on your genitalia or a part of your body you're not particularly familiar with or feel uncomfortable discussing.
Please be assured your doctor has done it all before.
Some of the ways we find patients find it easier to speak to a doctor is to either tell the doctor you feel embarrassed up front. That way a doctor can make extra effort to make sure you feel comfortable.
Or some patients come to us with pieces of paper and will write the problem down and hand it to us. That way we can help with whatever is going on for you as well.
You may also find it helpful to ask for a specific doctor, someone you're familiar with in your practice. Or you might want to ask for a doctor of a specific gender, or background to your liking as well.
I'd also say, doctors do this every day so don't be alarmed if we ask you certain questions around your symptoms. It is purely so we can help you get the best outcome for your enquiry.
And then finally, feel free to use language that suits you as well. We don't expect you to know the medical words for things, or a name for your diagnosis. That's our job to find out for you.
So, take your time, see a doctor, and hopefully we can help put your mind at ease.
Self-help for piles
There’s lots you can do to improve piles symptoms. You might like to try the following:
- eat a high-fibre diet to help make your poo softer and easier to pass
- don’t have too many caffeinated drinks, like tea and coffee
- keep active each day – if external piles makes cycling difficult use a cushioned seat pad
- try not to strain when you go to the toilet
- after having a poo gently clean around your anus with water and pat the area dry
Treatment of piles
Do piles go away?
Sometimes piles can go away without treatment. Most people don’t need an operation to treat piles. But if you still have symptoms of piles and other treatments haven’t worked, or your piles keep bleeding, surgery might be the right option for you.
How do you get rid of piles?
There are plenty of piles treatments that can relieve your symptoms. Below are the main treatments for piles.
Medicines for treating piles
Below are some medicines for piles – always read the instructions, and check with a doctor if you have any concerns.
- Fibre supplements such as ispaghula husk (eg Fybogel) can soften hard poo.
- A mild laxative such as lactulose can make poo easier to pass.
- Over-the-counter painkillers, such as paracetamol, may help to ease any pain from piles. Avoid opioid-based painkillers (such as codeine). These can cause constipation.
- Haemorrhoid creams, ointments, and suppositories may ease any pain and itchiness from piles. Some contain a local anaesthetic, such as lidocaine. Only use these for a few days as they may affect the sensitivity of your skin.
- Products containing corticosteroids, such as Anusol HC and Proctosedyl, may reduce swelling and pain. Don’t use these for more than a week as they can damage the skin around your anus. Most are available over the counter and others on prescription.
Non-surgical treatments for piles
Piles will usually go away on their own but, if they don’t, you might need a day case procedure at hospital. Non-surgical treatments include the following.
- Banding: a small elastic band is put around the pile, reducing the blood supply. The pile will die and fall off after a few days.
- Sclerotherapy: an injection of an oily solution into your piles, which will make them shrivel up.
- Infra-red coagulation: an infrared light is used to cut the blood supply to your piles and make them shrink.
- Bipolar diathermy and direct current electrotherapy treatment: In this procedure, heat or an electrical current is used to destroy the pile.
Your doctor will let you know the benefits and risks of each procedure and which is the best option for you.
Surgery for piles
Most people don’t need an operation to treat piles. But if you do, there are different types of surgery for piles, which include the following.
- Haemorrhoidectomy: pile removal surgery.
- Stapled haemorrhoidopexy: the area of tissue with piles are attached higher up your anal canal and stapled in place. Your piles then won’t come out your anus anymore and will shrink.
- Haemorrhoidal artery ligation operation (HALO): the blood supply to the piles is cut off, which makes them shrink.
Complications of piles
Piles rarely cause any serious problems but sometimes they can lead to the following.
- External piles can become inflamed and swollen; ulcers can also form on them.
- Skin tags can form when the inside of a pile shrinks back but the skin remains.
- If mucus leaks from your anus, it can make the surrounding skin very sore.
- Internal piles that hang down can sometimes get strangulated and lose their blood supply. If a blood clot forms (thrombosis), piles can be very painful. External piles can also become thrombosed.
Prevention of piles
Following a healthy lifestyle can help to prevent constipation. The following changes can help:
- Eat plenty of fibre-rich foods.
- Drink plenty of fluids – which helps to keep your poo soft.
- Limit caffeinated drinks, such as tea and coffee. And don’t drink too much alcohol.
- Exercise regularly.
How healthy are you?
With our health assessments you get an action plan that’s tailor-made for you.
To book or to make an enquiry, call us on 0345 600 3458
Rectal prolapse
A rectal prolapse is when part of your rectum sticks out through your anus (back passage) to form a lump.
How do you prevent constipation?
Constipation is a common condition that affects your usual pattern of bowel movements.
Did our Haemorrhoids (Piles) information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Hemorrhoids. BMJ Best Practice. bestpractice.bmj.com, last reviewed 28 January 2023
- Haemorrhoids. PatientPro. patient.info, last edited 22 August 2022
- Haemorrhoids. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised July 2021
- Cristea C, Lewis CR. Hemorrhoidectomy. StatPearls Publishing. www.ncbi.nlm.nih.gov, published 2022
- Anal canal anatomy. Medscape. emedicine.medscape.com, updated 29 June 2016
- Haemorrhoids. NICE British National Formulary. bnf.nice.org.uk, last updated 1 February 2023
- Hemorrhoids. Medscape. emedicine.medscape.com, updated 31 May 2022
- Digital rectal examination (DRE). Prostate Cancer UK. prostatecanceruk.org, updated January 2022
- Assessment of anaemia. BMJ Best Practice. bestpractice.bmj.com, last reviewed 28 January 2023
- Van Tol RR, Kleijnen J, Watson AJM, et al. European Society of Coloproctology (ESCP) guideline for haemorrhoidal disease. www.escp.eu.com, published 2020
- Personal communication, Mrs Sara Badvie, Consultant Laparoscopic, Colorectal and General Surgeon, 1 April 2023
- Constipation. NICE British National Formulary. bnf.nice.org.uk, last updated 1 February 2023
- Mckeown DG, Goldstein S. Hemorrhoid banding. StatPearls Publishing. www.ncbi.nlm.nih.gov, published 2022
- Circular stapled haemorrhoidectomy. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 17 December 2003
- Hemorrhoids: Expanded version. American Society of Colon and Rectal Surgeons. fascrs.org, accessed 28 February 2023
- Rachael Mayfield-Blake, Freelance Health Editor

Legal disclaimer
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.


