Beta-blockers
Your health expert: Madeeha Waheed, Oncology Pharmacist at Bupa, Medical Policy UKI
Content editor review by Rachael Mayfield-Blake, Freelance Health Editor, October 2022.
Next review due October 2025.
Beta-blockers (pronounced beeta-blockers) are medicines that make your heart beat more slowly and with less force. There are lots of different types of beta-blocker. While doctors prescribe them for a wide variety of health conditions, they’re best known for treating heart problems.
Uses of beta-blockers
Your doctor may recommend you take beta-blockers if you have a condition affecting your heart or blood vessels, such as:
- angina
- arrhythmia – for example, atrial fibrillation
- heart failure
- a previous heart attack – beta-blockers can reduce your risk of having another one
- high blood pressure (hypertension)– if other medicines haven’t helped to reduce your blood pressure
Beta-blockers are also sometimes used in the treatment of other conditions. For example, they may be used to:
- reduce the number of attacks you have if you get migraines
- relieve the physical symptoms of anxiety
- help manage the symptoms of an overactive thyroid gland
- treat glaucoma (an eye condition caused by a build-up of pressure in your eye)
- help with tremor (an uncontrollable trembling in part of your body) – especially for a condition known as essential tremor
Beta-blockers may not be suitable for everyone. For instance, a doctor may not be able to prescribe you a beta-blocker or will need to monitor you closely if you have any of the following health conditions.
- Asthma or other breathing problems such as chronic obstructive pulmonary disease (COPD). This is because beta blockers can sometimes make these problems worse.
- Worsening or unstable heart failure
- Severe narrowing of the arteries that carry blood to your arms and legs (peripheral arterial disease).
- Low blood pressure.
- Slow heart rate – especially a condition called heart block.
- Diabetes – especially if you regularly have episodes of low blood sugar levels.
- Raynaud’s (where the small blood vessels in your hands and feet are extremely sensitive to changes in temperature).
Let your doctor know if you’re pregnant or breastfeeding because they may need to take this into account if they prescribe a beta-blocker.
How beta-blockers work
Beta-blockers get their name from the way they work. They block the hormones adrenaline and noradrenaline so they work all around your body and can help to treat many different health conditions. Here, we just talk about how they affect your heart.
Beta-blockers slow your heart down and make it beat with less force. This means it doesn’t work so hard and doesn’t need as much oxygen. These effects are helpful if you have angina or heart failure, and can help to protect against further heart attacks.
Beta-blockers can also affect the way electrical signals pass through your heart, so they may be helpful if you have an irregular heart rhythm.
Beta-blockers can help to reduce blood pressure by widening arteries. Some beta-blockers are known to reduce levels of a protein called renin; this helps to control blood pressure.
Types of beta-blocker
There are different types of beta-blocker.
Non-selective beta-blockers
Non-selective beta-blockers block beta receptors all around your body. This means they affect your lungs and the blood vessels in your arms and legs, as well as your heart. Examples include propranolol (for example, Inderal) and nadolol (for example, Corgard).
Selective beta-blockers
Selective beta-blockers such as atenolol (Tenormin), bisoprolol (Cardicor) and nebivolol (Bystolic) target beta receptors in your heart. These medicines tend to be used more often for heart conditions because they’re less likely to cause side-effects elsewhere in your body.
Taking beta-blockers
Beta-blockers are only available on prescription from a doctor. Which one your doctor offers you will depend on why you need them. They come as:
- tablets or capsules
- syrup or solution
- injections – if they’re used to control an arrhythmia or following a heart attack
- eye drops (for glaucoma)
You take some beta-blockers once a day, others you may need to take two or three times a day. This will depend on what you’re taking them for and which beta-blocker your doctor has prescribed. Depending on your medical condition, your doctor may prescribe beta-blockers in combination with other medicines.
Stopping beta-blockers
If you’re unhappy with your beta-blockers for any reason (for example, because you’re getting side-effects) ask your doctor for advice. Don’t stop taking your beta-blocker medicine suddenly because your blood pressure may go up abruptly and you may get irregular heart rhythms (palpitations). If you take beta-blockers to treat angina (chest pain), suddenly stopping your medicine could make your chest pain worse.
If you need to stop taking beta-blockers, your doctor will tell you how to reduce your dose gradually. They may suggest you switch to a different beta-blocker or another type of medicine.
Always follow the instructions your doctor or pharmacist gives you about when to take your medicines. Read the patient information leaflet that comes with your medicine carefully. If you have any questions about your medicines or how to take them, ask a pharmacist.
Worried about your heart health?
Get a picture of your current health and potential future health risks with one of our health assessments.
To book or to make an enquiry, call us on 0333 920 7695∧
Interactions of beta-blockers
Beta-blockers can interact with certain other medicines, including some heart medicines, which can put you at increased risk of some side-effects. This also includes medicines for hypotension (low blood pressure). Your doctor will ensure that the medicines they prescribe are suitable to use together, and may monitor you if necessary.
Alcohol can interact with beta-blockers and cause a reaction. Always check with your doctor or pharmacist before you take any other medicine or alcohol at the same time as a beta-blocker.
Side-effects of beta-blockers
Like all medicines, beta-blockers can cause side-effects, but these usually aren’t serious.
This section doesn’t include every possible side-effect of beta-blockers. Please read the patient information leaflet that comes with your medicine for more details. The following are some of the more common side-effects.
- You may feel tired or even exhausted. This may be most obvious when you first start taking beta-blockers or if your dose is increased. It usually gets better after a while.
- Your hands and feet may feel cold. You may need to wear gloves and thick socks in cold weather.
- You may feel dizzy if your heart rate becomes too slow. See your doctor if this happens.
- You may have disturbed sleep, including nightmares or vivid dreams.
Side-effects often wear off with time as your body gets used to the medicines. But if side-effects from your beta-blocker medicine are bothering you, talk to your doctor. They may be able to reduce the dose or switch you to a different medicine. For more information, see our section on taking beta-blockers.
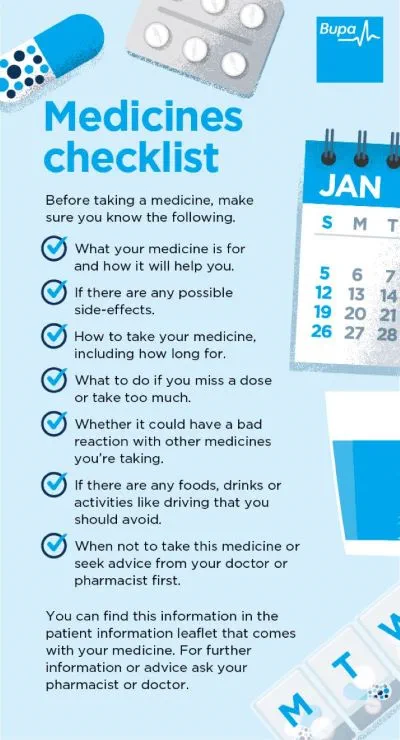
Medicines checklist
Our handy medicines checklist helps you see what to check for before taking a medicine.
Bupa's medicines checklist PDF opens in a new window (0.8MB)
Beta-blockers are most commonly used to treat heart problems. These include angina and an irregular heartbeat (arrhythmia) – for example, atrial fibrillation. Beta-blockers can also treat other health conditions: they can relieve the symptoms of anxiety and help to reduce the number of migraine attacks.
For more information, see our section: Uses of beta-blockers.
Side-effects of beta-blockers include feeling tired or even exhausted. And your hands and feet may feel cold. If your heart rate becomes too slow, you may feel dizzy. See your doctor if this happens. You may also have problems sleeping and get nightmares or have vivid dreams.
For more information, see our section: Side-effects of beta-blockers.
How long you stay on beta-blockers will depend on what you are taking them for, but it may be for the rest of your life. Ask your doctor to explain how long you’ll need to take them. It’s important to follow their advice. Don’t stop taking your beta-blocker medicine suddenly. If you do, your blood pressure may go up abruptly and you may get irregular heart rhythms (palpitations). If you need to stop taking beta-blockers, your doctor will tell you how to reduce your dose gradually.
For more information, see our section: Taking beta-blockers.
It’s possible you may put on weight when you take beta-blockers. There could be other factors linked to the weight gain. For instance, beta-blockers can make you tired, which may lead to you resting more and being less active. It’s important to keep active while you’re taking these medicines. Being physically active can make you feel better and is important for maintaining a healthy weight.
Angina
Angina is when you have chest pain or an uncomfortable tight feeling in your chest.
Heart attack
High blood pressure (hypertension)
Other helpful websites
Discover other helpful health information websites.
Did our Beta-blockers information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Beta-adrenoceptor blocking drugs. NICE British National Formulary. bnf.nice.org.uk, last updated 31 August 2022
- Watch: what are beta blockers and what do they do in your body? British Heart Foundation. www.bhf.org.uk, accessed 28 September 2022
- Farzam K, Jan A. Beta blockers. StatPearls Publishing. www.ncbi.nlm.nih.gov, last updated 21 July 2022
- Atrial fibrillation. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised August 2022
- Hypertension. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised July 2022
- Raynaud's phenomenon. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised February 2020
- Heart failure – chronic. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised July 2022
- Beta-blockers. Blood Pressure UK. www.bloodpressureuk.org, accessed 28 September 2022
- Propranolol hydrochloride. NICE British National Formulary. bnf.nice.org.uk, last updated 31 August 2022
- Nadolol. NICE British National Formulary. bnf.nice.org.uk, last updated 31 August 2022
- Atenolol. NICE British National Formulary. bnf.nice.org.uk, last updated 31 August 2022
- Nebivolol. NICE British National Formulary. bnf.nice.org.uk, last updated 31 August 2022
- Tenormin injection 0.5 mg/ml. emc. www.medicines.org.uk, last updated 7 January 2022
- Glaucoma. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised August 2022
- Medicines for my heart. British Heart Foundation. www.bhf.org.uk, published 2017
- UK Chief Medical Officers' physical activity guidelines. GOV.UK. gov.uk, published 7 September 2019