High blood pressure (hypertension)
Your health experts: Professor Mark Westwood , Consultant Cardiologist
Content review by Rachael Mayfield-Blake, February 2024.
Next review due February 2027.
High blood pressure is a common medical condition where the pressure inside your arteries (a type of blood vessel) is higher than it should be. You probably won’t get any high blood pressure symptoms. But you’re more likely to get conditions such as heart disease, a stroke or kidney disease. There’s a lot you can do to reduce your high blood pressure, but sometimes you’ll need to take medicines.
Having your blood pressure taken
Blood pressure | Watch in 2:19 minutes
If you have high blood pressure, it's important to get your blood pressure checked regularly. Having your blood pressure taken is a key health assessment tool. Discover how it happens during this video.
About high blood pressure
Every time your heart beats, it pumps blood under pressure to the rest of your body through blood vessels called arteries. You need some pressure to keep your blood moving. But if it’s always too high, it puts extra strain on your heart and blood vessels. Other parts of your body – for example, your brain and kidneys – may also be affected by high blood pressure.
The medical name for high blood pressure is hypertension.
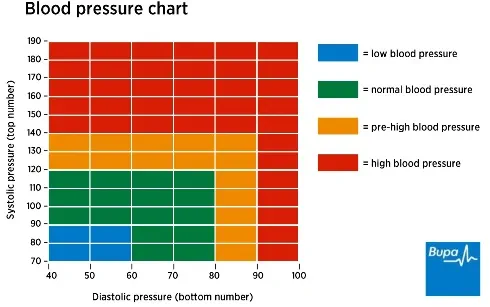
Blood pressure is measured at two points.
- The highest level (systolic blood pressure). This is when your heart muscle contracts and pumps blood out through the arteries.
- The lowest level (diastolic blood pressure). This is when your heart relaxes between beats and fills with blood.
Your blood pressure is shown as two numbers, measured in millimetres of mercury (mmHg). A reading of around 120/80mmHg is seen as healthy – above 140/90mmHg is considered high.
Causes of high blood pressure
For most people with high blood pressure, there’s no obvious cause. This is called primary hypertension or essential hypertension. Some things increase your risk of getting this type of high blood pressure. These include:
- your age – the risk increases as you get older
- your ethnic group – you have a higher risk of high blood pressure if you’re of African or black Caribbean origin
- having someone in your close family with high blood pressure
- being overweight or obese
- eating too much salt
- drinking too much alcohol
- not getting enough exercise
- anxiety and stress
Sometimes, high blood pressure is linked to an underlying medical condition. This is called secondary hypertension. Causes of secondary hypertension include:
- kidney disease
- pregnancy
- obstructive sleep apnoea (frequent pauses in breathing when you sleep)
- hormone disorders - for example, an underactive or overactive thyroid
- diabetes
Some medicines can increase your blood pressure. These include decongestant cough and cold remedies, anti-inflammatories, steroids and oral contraceptives. Always carefully read the information that comes with your medicine.
Herbal remedies (including teas) that contain liquorice can also raise your blood pressure. And illegal drugs such as cocaine can raise your blood pressure too.
Symptoms of high blood pressure
Most people don’t have any high blood pressure symptoms and aren’t aware of their condition. It’s usually found when you have your blood pressure measured. This may be as part of a health assessment or a regular check when you take certain medications – for example, the oral contraceptive pill.
If you have high blood pressure and it causes complications, you may get symptoms linked to the complications.
Diagnosis of high blood pressure
The only way to diagnose high blood pressure is to measure your blood pressure. Aim to check your blood pressure at least every five years; it’s important to know if your numbers have changed. You may be able to do this at your local pharmacy. It’s useful to know your readings so you can share these at any appointments you have with health professionals.
Measuring blood pressure
Your doctor or nurse will put a cuff on your arm that will gently inflate. Automated, digital devices make it quick and easy to check your blood pressure. Or, your doctor might take a reading using a stethoscope that they’ll hold against your arm to listen to the blood flow. Try to relax – it may be a little uncomfortable but it’s only for a few moments. To see how blood pressure is taken, watch our video on having your blood pressure taken.
Your GP or nurse will probably check your blood pressure several times during a visit. If your blood pressure is high, they may recommend you have more readings over a longer period to help make a definite diagnosis. There are two ways to do this.
- Ambulatory blood pressure monitoring (ABPM). You wear a device on your arm for 24 hours as you go about your normal activities. For more information, see our FAQ on 24-hour monitoring.
- Home testing. You can measure your blood pressure yourself at home for four to seven days. You measure your blood pressure morning and evening after resting for at least five minutes.
You can buy your own device to measure blood pressure at home. See the British and Irish Hypertension Society website for trusted devices.
Further tests
If you have high blood pressure, your doctor will want to find out if there’s a reason for this. They’ll also want to see if it has done any harm, especially to your heart or kidneys.
Your doctor will ask about your general health, any symptoms you have, and any medicines you take. They may ask about your family’s medical history. They may also ask about your weight, diet, whether or not you smoke, how much you exercise, and if you drink alcohol. They may examine you too.
Your doctor may offer you further tests, which may include the following.
- A urine test to check for protein or blood in your pee because that could be a sign of kidney damage.
- A blood test to check your cholesterol level which will assess your risk of heart disease. It will also check for diabetes, and problems with your kidneys.
- An electrocardiogram (ECG) to see how your heart is working.
- An examination of the back of your eyes with an ophthalmoscope to check if the blood vessels there are healthy.
If your blood pressure is very high or your GP suspects it’s caused by a serious condition, they may refer you to a specialist. They may also refer you to a specialist if you have high blood pressure and you’re under 40. Or if you have problems taking medicines to control your blood pressure. Your specialist may recommend further tests and will explain what these involve.
Self-help for high blood pressure
Your doctor will encourage you to make lifestyle changes to help reduce your blood pressure. These include the following.
- Lose excess weight. Aim to reduce your waist measurement. You are at an increased risk of high blood pressure if your waist measurements exceed 102cm (40 inches) in men, and 88cm (35 inches) in women. You are at a much lower risk of high blood pressure if your waist measurements are under 94cm (37 inches) for men, and below 80cm (31.5 inches) for women. Our video below shows you how to measure your waist. You should also aim to get your BMI (body mass index) down to 25 or less. You can find out your BMI using our BMI calculator.
- Be more physically active.
- Eat a healthy, balanced diet.
- Eat less salt – you should have less than 6g (one teaspoon) a day.
- Stick to recommended guidelines on how much alcohol you drink.
- Drink less coffee and other caffeinated drinks like cola.
- Try to improve your sleep. And be mindful that jet lag and constant travel can raise your blood pressure.
Stress can make your blood pressure go up, so learn how to manage stress.
Stopping smoking may not have a direct impact on your blood pressure, but it reduces the risk of complications like heart disease and stroke.
How to measure your waist
Waist measurements| Watch in 42 seconds
Learn easy and simple ways to measure your waist today.
Treatment of high blood pressure
There are several things your doctor will consider in deciding how best to treat you. These include:
- your age
- your ethnic group (especially if you are of African or Caribbean origin)
- any other medical conditions you have
- your risk of heart disease and stroke
- the possible causes of your high blood pressure
- how high your blood pressure is
Medicines
There are several medicines to lower your blood pressure that can be used in combination with self-help measures. Your GP may start you on a combination of two medicines. It can take time to find the medicines that work for you.
The medicines most often used to treat high blood pressure are listed here.
- Angiotensin-converting enzyme inhibitors (ACE inhibitors) such as ramipril or lisinopril. These relax and widen blood vessels.
- Angiotensin-II receptor blockers (ARBs) such as candesartan, losartan or valsartan. These work in a similar way to ACE inhibitors. They are an option if you get side-effects (for example, a dry cough) from ACE inhibitors.
- Calcium-channel blockers (CCBs) such as amlodipine or diltiazem. These relax and widen your blood vessels so your heart receives a better blood supply. This means it needs to do less work to pump blood round your body.
- Thiazide diuretics such as bendroflumethiazide and indapamide. These make your kidneys produce more pee. This reduces the amount of fluid in your blood.
If these medicines aren’t suitable for you or if they don’t work well enough, your doctor may prescribe other medicines to treat your high blood pressure. For instance, sometimes beta-blockers may be suitable.
Always read the information that comes with your medicines. If you have any questions about taking them, ask a pharmacist.
Your doctor may suggest you regularly monitor your blood pressure at home as part of your treatment.
Worried about your heart health?
Get a picture of your current health and potential future health risks with one of our health assessments.
To book or to make an enquiry, call us on 0800 665 577
Complications of high blood pressure
Complications of high blood pressure include:
- coronary heart disease (including angina and heart attack)
- heart failure
- a stroke
- kidney disease or failure
- peripheral artery disease
- problems with your sight
- vascular dementia
With medicines and lifestyle changes, you can reduce the risk of these happening.
Special considerations for high blood pressure
Diabetes
High blood pressure is a particular issue if you have diabetes. Both hypertension and diabetes increase the risk of kidney disease and cardiovascular disease. If you have diabetes, get your blood pressure measured at least once a year.
Pregnancy
If you’re pregnant, you’ll have your blood pressure checked regularly. Having high blood pressure during pregnancy may cause problems for you and your baby. It may be a sign of a condition called pre-eclampsia.
If you’re on medicines for high blood pressure and you get pregnant, your doctor may suggest you change your medicines.
High blood pressure that develops during pregnancy may get better by itself after you give birth. But you may be more at risk of getting high blood pressure again later in life.
A blood pressure measurement consistently above 140/90mmHg is considered high, whereas a reading of around 120/80mmHg is seen as healthy. Your blood pressure will naturally go up and down during the day and night, and when you’re resting or active. But if you get tested and it’s always high, even when you’re sitting down, you have high blood pressure. If your measurement is between 120/80 mmHg and 140/90 mmHg, you should make some changes to your lifestyle so you don’t develop high blood pressure.
For more information, see our section about high blood pressure.
Most people with high blood pressure don’t have any symptoms, so you may not realise. The only way to find out if your blood pressure is high is to have it checked. It’s a good idea to have your blood pressure checked at least every five years, and more often if you have diabetes.
For more information, see our section on diagnosis of high blood pressure.
Your GP can prescribe medicines to lower your high blood pressure. But there’s a lot you can do yourself too and it’s important to take these steps. This includes losing weight, being more active, drinking less alcohol and eating a healthy diet.
For more information, see our sections on self-help for high blood pressure and treatment of high blood pressure.
There isn’t one main cause of high blood pressure and for most people, there’s no obvious cause at all. But some things increase your risk of getting high blood pressure. These include being overweight or obese, or drinking too much alcohol. High blood pressure is sometimes linked to an underlying medical condition such as kidney disease or obstructive sleep apnoea (frequent pauses in breathing when you sleep).
For more information, see our section on causes of high blood pressure.
You wear a small digital machine on a belt round your waist and an inflatable cuff on your upper arm for 24 hours. Your blood pressure will be measured every 30 minutes or so, including overnight. You can carry on with your normal activities, but don’t get the equipment wet. Your nurse or GP will explain what the test involves and can answer any questions you have about it.
For more information, see our section on diagnosis of high blood pressure.
Coronary heart disease
Stroke
How to start exercising
We should all be getting active – and it may be easier than you think. Here we give you tips and advice for getting started
Other helpful websites
Discover other helpful health information websites.
Did our High blood pressure (hypertension) information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Hypertension. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised March 2023
- Hypertension. MSD Manuals. msdmanuals.com, reviewed/revised September 2023
- Iqbal AM, Jamal SF. Essential hypertension. StatPearls Publishing. www.ncbi.nlm.nih.gov, last updated 20 July 2023
- High blood pressure. British Heart Foundation. www.bhf.org.uk, last updated March 2023
- Hypertension in adults: Diagnosis and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 21 November 2023
- Essential hypertension. BMJ Best Practice. bestpractice.bmj.com, last reviewed 11 December 2023
- Hypertension. Patient. patient.info, last updated 30 June 2022
- BP monitors. British and Irish Hypertension Society. bihsoc.org, accessed 11 January 2024
- Salt. British Heart Foundation. www.bhf.org.uk, accessed 11 January 2024
- Hypertension medication. Medscape. emedicine.medscape.com, updated 9 November 2022
- Calcium-channel blockers (CCBS). Blood Pressure UK. www.bloodpressureuk.org, accessed 11 January 2024
- Diuretics. Blood Pressure UK. www.bloodpressureuk.org, accessed 11 January 2024
- Diabetes – type 2. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised November 2023
- Antenatal care – uncomplicated pregnancy. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised February 2023
- Hypertension in pregnancy: Diagnosis and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 17 April 2023
- Hypertension. NICE British National Formulary. bnf.nice.org.uk, last updated 22 November 2023
- Further health tests. Blood Pressure UK. www.bloodpressureuk.org, accessed 11 January 2024



