Angina
Expert reviewers: Dr Khalid Khan, consultant cardiologist; Professor Mark Westwood, consultant cardiologist; Nafisa Rahim, GP
Content editor review by Victoria Goldman, Freelance Health Editor
Next review due October 2025
Angina is when you have chest pain often described as an uncomfortable tight or heavy feeling in your chest. This is often on the left side. It happens when not enough blood is getting to your heart muscle. The pain and discomfort can sometimes spread to your arms, jaw, upper tummy, neck and back. In addition, you can feel short of breath or sweaty.
About angina
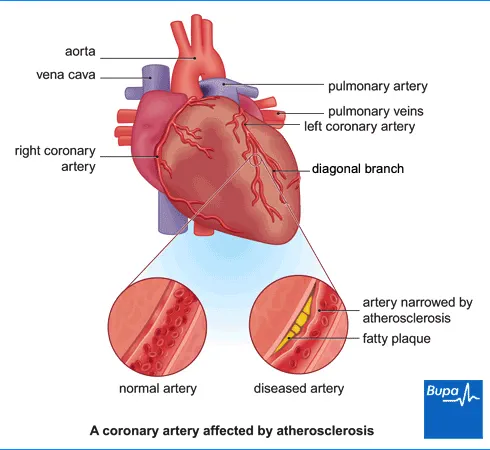
Angina is usually a symptom of coronary heart disease. If you have coronary heart disease, plaques of a fatty substance called atheroma build up in the walls of your blood vessels. This process is called atherosclerosis and it makes your blood vessels get narrower. This makes it harder for blood and oxygen to get to your heart muscle.
You’re most likely to notice angina when your heart’s working harder than usual – for example, when you’re exercising or if you are under emotional stress. Angina can be a sign that you may be at risk of serious health problems. It may lead to a heart attack, which can be life-threatening. But you can usually keep your angina symptoms under control with angina treatments and some healthy lifestyle changes. .
If you’re reading this because you have chest pain now, go directly to our section: What to do if you have chest pain.
Causes of angina
Angina is usually caused by coronary heart disease. You’re more likely to have coronary heart disease if you:
- have high blood pressure
- have diabetes
- have high cholesterol
- smoke
- have an inactive lifestyle
- are overweight
- have a family history of heart disease
- are older
- are male
How coronary heart disease (atherosclerosis) develops
Animation | Coronary heart disease (atherosclerosis) | Watch in 1:30 mins
Coronary heart disease happens when fatty deposits build up on the walls of the arteries to the heart. This is known as atherosclerosis. In this video, we explain how atherosclerosis develops.
Symptoms of angina
The main angina symptoms are chest pain or discomfort.
- You may feel a heaviness or pressure in your chest or like you’re being squeezed tightly.
- The pain or discomfort can be in the middle of your chest or spreading to your back, jaw, arms, shoulders and neck.
- The pain or discomfort doesn’t change when you move, breathe in or out or cough
For more information, see our section: What to do if you have chest pain.
If you have already been diagnosed with angina, see your GP as soon as you can if:
- your symptoms begin to change
- you get other symptoms such as feeling or being sick, sweating or dizziness
What to do if you have chest pain
If you haven’t been diagnosed with angina
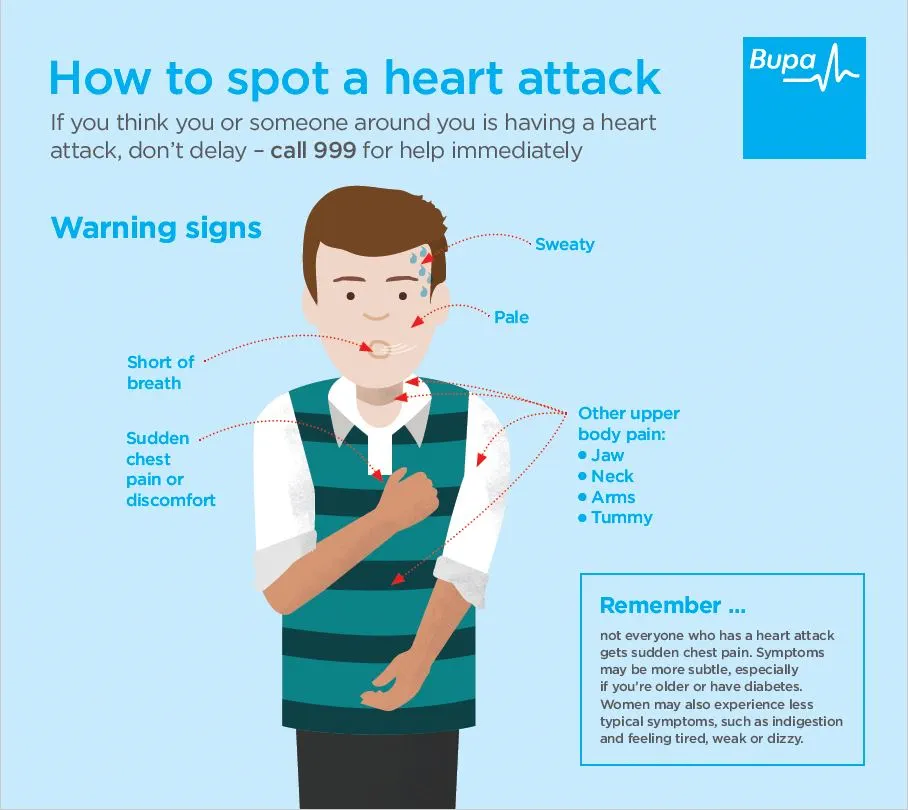
It can be difficult to tell the difference between angina and a heart attack because the symptoms can be similar. If you’ve never been diagnosed with angina, and you have chest pain which doesn’t go away after a few minutes, call 999. Other symptoms of a heart attack include shortness of breath, sweating and feeling sick.
See our infographic on how to spot a heart attack (PDF, 0.7MB) or click on the image below.
If you have been diagnosed with angina
If you’ve been diagnosed with angina and you have an angina attack, you should:
- stop what you’re doing, sit down and rest
- use your glyceryl trinitrate (GTN) spray or tablets (for more information, see our section: Treatment for angina)
- take a second dose of GTN after five minutes if the pain hasn’t eased
- take a third dose of GTN if the pain hasn’t eased after another five minutes
- call for an ambulance if your pain hasn’t eased five minutes after the third dose (15 minutes after your pain started). But call for an ambulance earlier than this if your pain is getting worse and you’re feeling unwell
Diagnosis of angina
Your doctor will usually ask you about:
- your symptoms
- your lifestyle
- your and your family’s medical history
They’ll also:
- examine you
- take your blood pressure
- listen to your heart and chest with a stethoscope
After that, your doctor may ask you to have some tests, including:
- blood tests – to check your glucose and cholesterol levels and for other health problems
- an electrocardiogram (ECG) – this shows the electrical activity of your heart
Your GP may refer you to a heart specialist (a cardiologist) for more tests or for treatment. You may have some of the following tests.
- Imaging tests such as a specialist computer tomography (CT scan) or specialist cardiac magnetic resonance imaging (MRI). These may include scans of your chest, tummy and coronary arteries (the vessels that supply your heart with blood).
- An echocardiogram, either when you’re resting or exercising. This test uses ultrasound to make moving images of the structure of your heart.
- An invasive coronary angiogram. A special dye is injected into your coronary arteries to make them show up on X-rays. It can show where a blood vessel is narrowed or blocked.
Self-help for angina
There are lots of things you can do to help control your symptoms and stop angina getting worse.
- Make sure you know what to do if you have chest pain. And always have your glyceryl trinitrate (GTN) medicine with you. For more information, see our section: What to do if you have chest pain.
- Plan your activities to avoid things you know trigger your chest pain.
- If your angina starts to get worse, the pain gets more severe or you’re getting an angina attack more often, contact your GP.
- If you smoke, stop. Ask your GP or pharmacist for advice or look online for local stop-smoking services.
- If you’re overweight, try to lose the extra weight.
- Eat a healthy, balanced diet that’s low in saturated fat, salt and sugar and high in fibre, fruit and vegetables.
- Stick to the recommended limits for alcohol. The current guidelines are for adults to drink no more than 14 units of alcohol a week, and to spread this out over the week.
Keeping active
Talk to your GP or nurse about how to exercise safely. They may be able to refer you to a cardiac rehabilitation programme.
- Aim to do 30 to 60 minutes of activity on at least five days of the week.
- Do an activity at a level that makes you feel warm and slightly out of breath.
- Choose activities such as walking, cycling and swimming.
- Don’t lift weights or do very vigorous sports like squash.
- Pace yourself. Stop what you’re doing if you get chest pain, very breathless or leg pain.
- Don’t exercise outside when it’s cold or very windy.
Your doctor may advise you to take your GTN medicine before doing some activities.
Driving with angina
If you have angina, you can probably drive as long as your symptoms are under control. But this varies from person to person and depends on which type of vehicle you drive.
- If you have a car or motorcycle licence, you don’t usually need to tell the Driver and Vehicle Licensing Agency (DVLA) about your angina. But you shouldn’t drive while you have any symptoms.
- If you drive a bus or lorry, you must tell the DVLA if you have angina. You won’t be able to drive until you’ve not had any symptoms for at least six weeks and have passed an exercise test.
It’s important to speak to your doctor about driving, and also to check with your insurance company.
Travelling by plane
Most people with angina can travel by plane. But it’s important to speak to your doctor because this will depend on your symptoms.
- If you only get chest pain after a lot of activity and your symptoms or medicines haven’t changed, you should be able to travel as normal.
- If you get chest pain after a little activity but your symptoms or medicines haven’t changed, you should ask for help at the airport. You should also consider asking for oxygen to be available during your flight.
- If you get chest pain when you’re resting or your symptoms and/or medicines have changed recently, you may want to postpone your flight. Or you could travel with a medical escort and make sure oxygen is available during your flight.
Treatment for angina
There are several treatment options for angina, depending on what type you have and whether or not you have other health conditions as well.
Medicines
Medicine to treat angina attacks
If you have stable angina, your GP will prescribe a medicine called glyceryl trinitrate (GTN). This opens up your coronary arteries so more blood can flow to your heart. GTN usually comes as either a spray or a small tablet that you put under your tongue. You take this when you have an angina attack. GTN works within a few minutes and should help to ease the pain. You can also take GTN before doing activities that you know may trigger an angina attack.
Medicines to prevent angina attacks
Your doctor may prescribe medicines for you to take regularly. These may help to prevent an angina attack and reduce your chance of having further heart problems. You may be offered one or more of the following medicines.
- An anti-clotting medicine, such as aspirin or clopidogrel. This helps to stop blood clots forming and can make you less likely to have a heart attack.
- Medicines to lower and control your blood pressure.
- Anti-angina medicines, such as beta-blockers and calcium channel blockers. These help to reduce the symptoms of angina and prevent angina attacks.
- Statins. These help to lower your cholesterol level to reduce your risk of having a heart attack in the future.
- ACE inhibitors may be helpful in stopping heart disease getting worse if you have angina.
Your doctor may suggest some other medicines that work in similar ways to those listed above. They’ll talk to you about how these medicines may help and discuss any potential side-effects. Always read carefully the patient information leaflet that comes with your medicine. If you have any questions about taking your medicines, ask your pharmacist.
Surgery
If your symptoms aren’t getting better using medicines, your doctor may suggest you have an operation.
These are the two main procedures.
- A coronary angioplasty (also called percutaneous coronary intervention, PCI) can widen your narrowed coronary artery. In this procedure, your doctor will pass a thin tube into your artery. When the tube reaches the narrow part, your doctor will use a tiny balloon to widen the blood vessel. They’ll usually put a stent (a mesh tube) inside the blood vessel. The stent is then left in place to help keep the artery open.
- A coronary artery bypass graft (CABG) operation. Your surgeon takes a piece of a blood vessel from your leg, arm or chest. They use it to bypass the narrowed blood vessel. This can improve the flow of blood to the artery that supplies blood to your heart muscle.
If your cardiologist recommends one of these procedures, they’ll tell you what’s involved and discuss the benefits and risks with you.
Complications of angina
Angina can lead to complications, including:
- heart attack
- irregular heart rhythms
- heart failure
If you have angina, you may find it harder to do some of your everyday activities. This may reduce the quality of your life. You may also worry about your angina symptoms. For some people, this may lead to depression.
Most people with angina can lead very active lives with few symptoms or complications.
Prevention of angina
You may be able to prevent angina by having a healthy lifestyle. This includes:
- not smoking
- losing excess weight
- being physically active
- eating a healthy diet that’s low in fat and salt, while high in fruit, vegetables, grains, pulses and beans
- aiming to have two portions of fish a week, one of which should be an oily fish like sardines or salmon
- staying within the recommended alcohol limits – the current guidelines are for adults to drink no more than 14 units of alcohol a week
Worried about your heart health?
Get a picture of your current health and potential future health risks with one of our health assessments.
To book or to make an enquiry, call us on 0800 665 577
Other helpful websites
Discover other helpful health information websites.
Heart attack
Coronary heart disease
How to start exercising
We should all be getting active – and it may be easier than you think. Here we give you tips and advice for getting started
Three myths about heart disease and five tips to prevent it
Understand what heart disease is, debunk some common myths and learn how to reduce your risk.
Did our Angina information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Stable ischaemic heart disease. BMJ Best Practice. bestpractice.bmj.com, last reviewed April 2022
- Angina. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised January 2022
- Chest pain. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised August 2021
- Angina pectoris. Medscape. emedicine.medscape.com, updated July 2018
- Unstable angina. Medscape. emedicine.medscape.com, updated October 2020
- Acute myocardial infarction. Patient. patient.info, last reviewed December 2020
- Angina pectoris. MSD Manuals. msdmanuals.com, last full review/revision July 2020
- Heart health: Food fact sheet, top tips for a healthy heart. BDA The Association of UK Dietitians. www.bda.uk.com, updated July 2020
- Alcohol consumption: advice on low risk drinking. UK Chief Medical Officers' low risk drinking guidelines. Department of Health. gov.uk, published August 2016
- Heart disease and physical activity. Patient. patient.info, last reviewed December 2015
- Glyceryl trinitrate. NICE British National Formulary. bnf.nice.org.uk, last updated May 2022
- Driving and medical conditions. gov.uk, accessed June 2022
- Dislipidaemias. NICE British National Formulary. bnf.nice.org.uk, last updated May 2022
- Percutaneous coronary intervention (PCI). Medscape. emedicine.medscape.com, updated November 2019
- Coronary artery bypass grafting. Medscape. emedicine.medscape.com, updated March 2022
- Unstable angina. BMJ Best practice. bestpractice.bmj.com, last reviewed April 2022
- Stable angina. Patient. patient.info, last reviewed March 2022