How do you prevent constipation?
Constipation is a common condition that affects your usual pattern of bowel movements. You may go less often than usual, or you may find it difficult or uncomfortable to go. You might also feel like you haven’t emptied your bowels completely. Here, I talk about what constipation is and how you can prevent it.

What causes constipation?
If you have constipation, you’ll go less often than normal and may have hard or lumpy poo that’s smaller or larger than usual. If this goes on for longer than three months, it’s called chronic constipation. Anyone can get constipation, but it’s twice as common in women than it is in men. It’s also common in pregnant women, people over 65, and children.
There are lots of reasons why you may be constipated. These include:
- your diet – for example, if you don’t eat enough fibre or drink enough fluids
- taking certain medicines such as some types of antidepressant, calcium or iron supplements, and painkillers like codeine or morphine
- not being active enough
- not going to the toilet when you need to go
Some people get constipation for no obvious reason.
What are the signs of constipation?
The main constipation symptoms include:
- straining when you try to have a poo
- feeling as though you haven’t fully emptied your bowel
- passing poo that’s either larger or smaller than normal, or that’s hard and lumpy
- having fewer than three bowel movements a week
If you see blood coming from your back passage (rectum), either on toilet paper or in the toilet, contact your GP as soon as possible.
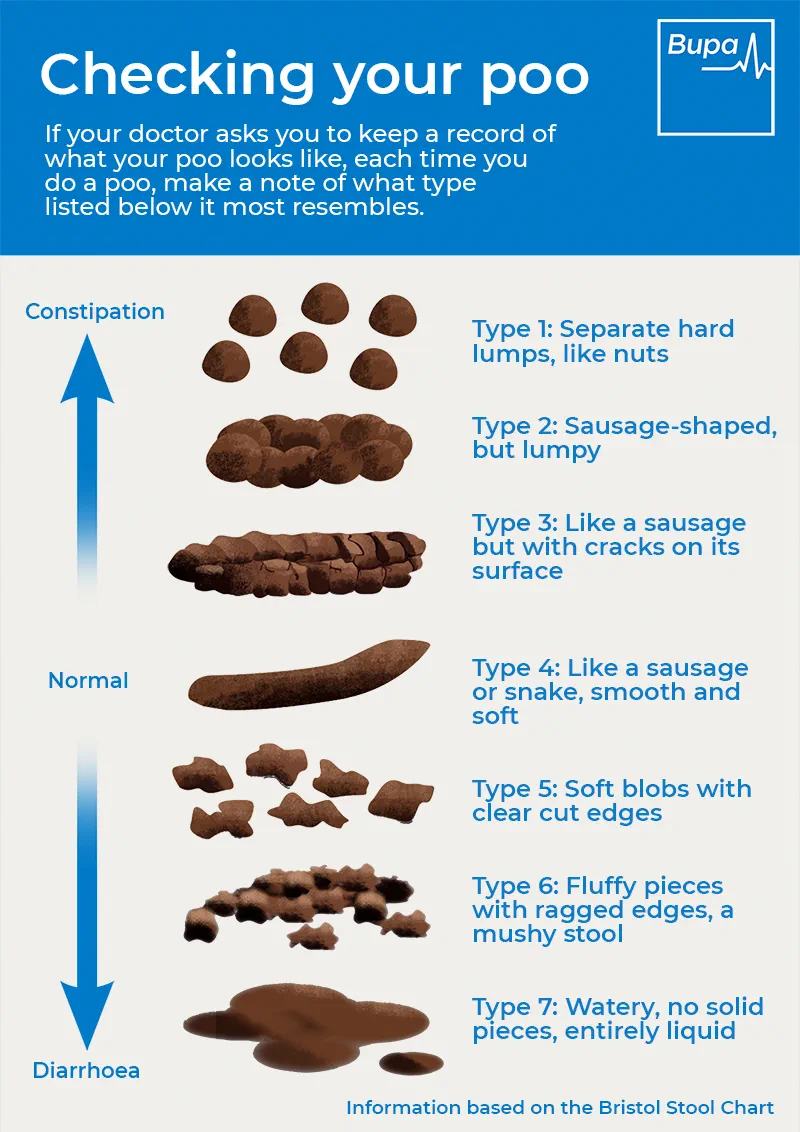
Infographic: Checking your poo
Bupa's 'Checking your poo' infographic (PDF, 1.8MB), helps you understand what’s normal, and what is constipation or diarrhoea.
Normal poo is smooth and sausage shaped. If your poo is very hard and lumpy this might be a sign of constipation. If your poo is watery and loose this might be diarrhoea.
How can I get constipation relief?
There are some self-help measures that can help with constipation. This includes increasing the amount of fibre you eat and drinking enough fluids. This can help to relieve constipation and is good for your general health. Doing regular exercise can also be helpful. It doesn’t need to be too strenuous or vigorous – modest exercise can help ease constipation.
What medicines treat constipation?
A type of medicine called a laxative can help to relieve constipation if self-help steps haven’t worked. There are several types of laxatives that work in different ways.
A pharmacist or GP will usually recommend you start treatment with a bulk-forming laxative. These work by bulking up your poo and drawing in water. This stimulates your bowel muscles to move and push poo out. If you continue to have problems, you might need to try an osmotic laxative. This sort of laxative draws water into the bowel to soften your poo. If you find your poo is soft but you still find it difficult to have a bowel movement, you can try a stimulant laxative. These stimulate the muscles in your bowel to contract more often and with more force.
If laxatives are not reliving your constipation, talk to your GP to see if they can offer any other treatments.
What should I eat to prevent constipation?
Fibre is important for your digestive health. It helps to bulk up the poo in your large bowel and move it along your digestive tract more quickly, helping to prevent constipation. Fibre also makes your poo softer, which helps with this process. It's recommended that adults should have 30g of fibre a day.
Fibre is found in all types of fruit and vegetables, so aim to eat at least five portions a day.
Other good sources of fibre include:
- wholegrain cereals
- wholemeal bread
- wholegrain rice
- rolled oats or oat bran
- seeds, such as flax seeds
- pulses, such as peas and beans (though for some people, these can cause bloating)
It’s also important to drink plenty of fluids.
What else prevents constipation?
A sedentary lifestyle or not moving around enough can be linked to constipation, so it’s important that you try to exercise regularly. Make sure you are going to the toilet regularly when you need to go.
Constipation can be very uncomfortable and painful. But, it can be easily managed with a healthy diet and there are treatments available for severe constipation.
Are you interested in learning more about your health? Discover more about our range of health assessments.
-
Sources Sources
- Constipation. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised September 2021.
- Constipation. BMJ Best Practice. bestpractice.bmj.com, last reviewed September 2022.
- Constipation in Adults. Patient. patient.info, last edited January 2022.
- Oxford Handbook of Nutrition and Dietetics 3e (3 edn, online), published April 2020.
- Constipation. Nice British National Formulary. bnf.nice.org.uk, last accessed October 2022.
- Fibre: Food fact sheet. The Association of UK Dietitians, published April 2021.
- Fibre: for everyone? Guts UK. gutscharity.org.uk, last accessed October 2022.
About our health information
At Bupa we produce a wealth of free health information for you and your family. This is because we believe that trustworthy information is essential in helping you make better decisions about your health and wellbeing.
Our information has been awarded the PIF TICK for trustworthy health information. It also follows the principles of the The Information Standard.

More mental health and wellbeing articles
Did you find our advice helpful?
We’d love to hear what you think. Our short survey takes just a few minutes to complete and helps us to keep improving our healthy lifestyle articles.
Legal disclaimer
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.







