Dementia and Sundowning

Your health expert: Fran Vandelli, Dementia Lead, Bupa Care Services
Publish date 05/03/2025.
Next review 12/03/2028.
Fran Vandelli, Dementia Lead, Bupa Care Services, explores online search trends around sundowning and practical steps to care for affected loved ones.
What is sundowning?
Sundowning is a term that describes a wide range of behavioural symptoms with wide ranging causes. These symptoms may be more frequent later on in the day, but they can also be unrelated to the sun’s position.
Symptoms can include:
It can affect anyone, but it’s common with people living with dementia.

66 per cent of people living with dementia have experienced sundowning
Our sundowning and dementia research
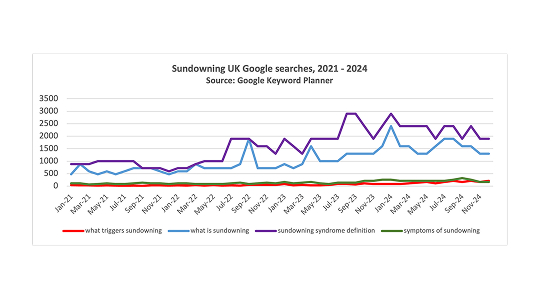
Our research shows more people are recognising how dementia symptoms can change throughout the day, particularly in the evening.
Between 2021 and 2024
- What triggers sundowning?
Searches became 7 times higher - What is sundowning?
Searches have tripled - Medications that cause sundowning
Searches have doubled
During autumn and winter, some find that their loved one's sundowning symptoms worsen. It's thought that the lack of natural light during these seasons may make it especially difficult for people affected, leading to increased anxiety and confusion than other times of the year.
Sundowning behaviours to look out for
Recognising the signs of sundowning is essential for caregivers to provide effective support. Key behaviours to look out for include:
Increased confusion
Those who experience typical sundowning symptoms may become more forgetful or struggle to recognise familiar places.
Living with dementia can be very tiring, especially if the person has been struggling to keep up with the day's antics without rest. This fatigue and stress can worsen confusion.
Disorientation
Those affected may become disorientated in their surroundings, leading to misunderstanding their environment.
For example, they might look at the clock and be convinced that they need to run an important errand from earlier in their lives, like picking their children up from school.
Difficulty sleeping
Trouble falling or staying asleep during the night is often reported. It's important to get enough direct sunlight at the beginning of the day to help the brain wake up properly.
Without this, it's hard for the brain to know when it's time to sleep, as melatonin production becomes limited.
When it comes to people living with dementia, we often leave the lights on for them, thinking it's safer. However this means that they're less likely to sleep well when they go to bed.
Agitation and restlessness
This can show as pacing, rocking, or being unable to sit still. Medications, such as psychotropics, can lead to restless leg syndrome, restlessness and fidgeting.
Mood swings
Sudden changes in mood, such as irritability, anxiety, or sadness.
What triggers sundowning?

We don't know for sure what triggers sundowning, but as the label of the behavioural symptoms suggests, it's often linked to when the sun goes down.
However, it can also happen at any time of the day. Sundowning can happen at any stage of a dementia diagnosis, but it tends to be more common the more the condition develops.
It's thought the latter part of the day may trigger behavioural changes. For example, if you've been feeling tired, thirsty, hungry or overstimulated, this can worsen symptoms. Symptoms include restlessness, disorientation, mood swings and trouble sleeping.
When it becomes dark outside and people typically retreat indoors, it may be unsettling for people living with dementia. They may become agitated if they forget where they are, or worry about what they think they should have been doing that day.
Dementia expert's tips for managing sundowning
If a loved one is experiencing sundowning symptoms, there are a few ways you can help to manage their distress. As we don't yet understand everything about this behaviour, there's no clear formula to ease symptoms for all. It may be a case of trial and error to adapt what your loved one needs at that time.
Check your loved one's immediate needs
Have they been lacking anything during the day, like food, drink or toilet access? Try to offer them these outlets to see if it helps alleviate their distress.
Sundowning symptoms may also be similar to ways a person would behave if they’re in physical discomfort. Be sure to make sure your loved one isn’t injured, struggling with a water infection or in need of pain relief.
Assess what's happened during the day
Has anything happened during the day that may have impacted your loved one? They may be acting out from frustration if they don't feel they've been listened to. A change in surroundings may lead to distressed feelings, too.
If nothing obvious has happened during their day, it may be useful to start a diary for a few weeks to record your loved one's actions. This could include what they've eaten and drank, to help spot any behavioural patterns and get an idea of anything that may be triggering them.
Offer meaningful disractions
Simple distraction techniques may help ground your loved one during a sundowning episode. Try playing their favourite music, offering to make them a drink or snack, or moving into a different but familiar room with them.
Sometimes, being close to your loved one and holding their hand can help soothe them.
Check their immediate surroundings
Your loved one's environment - especially when the sun sets - may contribute to sundowning triggers. Look at their room from their perspective and be mindful of any ways items could be disorientating them.
It may be worth repositioning objects or drawing curtains to reduce glare and shadow. This could include lights flashing or reflecting in mirrors, or shadows casting on the walls. Also consider the brightness of the room - is it bright enough to highlight uneven surfaces?
Communicate clearly and simply
Remain calm, and ask them clearly and slowly what's wrong. They may offer a response that you're able to directly help with, like food and drink. Try to use short sentences to avoid confusion.
If you need to give them instructions, make them simple and clear for example "can you come over here, please?”
Light therapy for sundowning
Research into this topic is still in the early stages, but there are signs that light therapy may help dementia and sundowning symptoms. It's thought that bright light therapy may help regulate your body's circadian rhythm. This could reduce the need to nap and increase nighttime sleep quality.
Your circadian rhythm acts as your body s internal biological clock. It helps control and standardise your body's functions each day. Bright light therapy uses a special light box that emits a higher amount of light than a person usually gets throughout the day.
When the months are darker, sitting in front of a light box for a set time each day has been linked to calming people living with dementia. This can help promote uninterrupted sleep. It's good practice to help your loved one to get sunlight exposure during the day, anyway. You could do this by going out for a walk together or ensuring they have access to seating by a window.

What's the best way to prevent sundowning?
There isn't a clearcut way to prevent sundowning. Everyone affected by it is different and may have different triggers. Trying out some of the following sundowning prevention techniques might offer you and your loved one some peace:
Keep a daily routine
Incorporate activities that you know your loved one will enjoy, from visiting a local beauty spot to watching their favourite TV show.
Adding structure to your loved one's day can help reduce the temptation to nap which may add to their nighttime sleep quality.
Close curtains and blinds before sundown
When it comes to the evening, close curtains and blinds before sunset arrives to help your loved one adjust to the evening more easily.
Create a wind down routine with your loved one to help soothe and calm. Keep media volume quiet to signify it's time to get ready to sleep.
Keep evening meals small
During their evening meal, don't overwhelm them with portion size.
Eating too much before bed may lead to disrupted sleep.
Offer caffeine-free drinks
Caffeine-free drinks alternatives encourage better sleep patterns.
Cover reflective surfaces
Cover reflective surfaces like windows and mirrors. They may exacerbate those with sundowning symptoms.

The toll of sundowning on caregivers
Watching a loved one experience sundowning symptoms can be difficult. Being a carer can affect your mental and physical health. Alongside helping your loved one, it's important to recognise the signs of carer burnout and take the time to offload and recuperate.
If you're struggling to balance caring alongside your other responsibilities, remember that there is support and advice available to you. From speaking to trusted friends and family, to contacting charities, there are outlets to help you make sense of what you're going through.
You might want to consider respite care to give your loved one chance to receive professional care, and so that you can catch up with errands or self-care.


