Lymphoedema
Your health expert: Dr Kristiana Gordon, Associate Professor and Consultant Physician in Dermatology and Lymphovascular Medicine
Content editor review by Rachael Mayfield-Blake, September 2023
Next review due September 2026
Lymphoedema (pronounced lim-fo-dee-mah) is the build-up of a fluid, called lymph, in a part of your body which causes it to swell. Lymphoedema can affect any part of your body, but often happens in your arms or legs, as a result of faulty genes or damage to the lymphatic system.
About lymphoedema
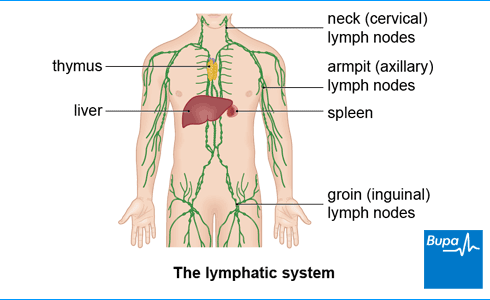
Lymphoedema happens when something goes wrong with your lymphatic system. Your lymphatic system includes a network of tubes that drain fluid (lymph) from all the tissues in your body. Lymphatic fluid passes through nodes (or glands), which filter it and remove waste and harmful cells. Your lymphatic system helps to maintain the right fluid balance in your body. It also supports your immune system as it fights infection.
When there’s a fault in your lymphatic system, the lymph fluid can’t drain away properly. This causes a build-up of lymph, which then collects in your tissues and causes swelling. It also increases your risk of skin infections if you damage your skin.
Causes of lymphoedema
There are two main types of lymphoedema, primary and secondary, which have different causes.
Primary lymphoedema is rare and is caused by problems with how your lymphatic system develops. You can be born with primary lymphoedema but it can also develop later in life (but the fault will have been present since birth). It may be something that runs in your family, but sometimes your lymphatic vessels just don’t develop properly for some reason.
Secondary lymphoedema is much more common. It’s caused by damage to your lymphatic system. A number of things can cause secondary lymphoedema, which include:
- cancer treatment – including surgery to remove lymph nodes (often for breast cancer), and radiotherapy, which can damage lymph nodes
- cancer – where enlarged lymph nodes or a tumour block the flow of lymph
- infections such as cellulitis of the leg, or a roundworm infection if you’ve travelled to a developing country
- an injury to your armpit or groin
- being very overweight (obese) – this can cause leg lymphoedema or make it worse
- reduced mobility – lack of movement will stop lymph from moving around your body
- problems with veins, such as varicose veins, which can overload your lymphatic system in your legs
Symptoms of lymphoedema
Early lymphoedema
One of the first lymphoedema symptoms you may notice is swelling in part of your body. This is most common in an arm, leg, hand, foot, but can affect other areas including your face or your genital area. There may only be a slight swelling at first, and it may be more noticeable towards the end of the day or in hot weather. Your jewellery, clothes or shoes may start to feel tight before you notice any swelling. If you get lymphoedema in your leg or arm, it may feel heavy too.
You may notice that your skin looks like it has compressions in it (pitting) – when you press your skin, the indentation remains.
Seek medical help as soon as you notice these symptoms as it’s best to start treatment as soon as possible. See your GP or, if you’re under the care of a cancer team, your cancer doctor or nurse. They should refer you to see a lymphoedema therapist, or sometimes a lymphoedema specialist doctor (if there is any doubt about the diagnosis).
Advanced lymphoedema
If you don’t get treatment, the swelling may become worse and more constant (it doesn’t go away overnight). The swollen area may turn very hard and solid, and the skin over the affected area can thicken and become rough.
Sometimes, in very advanced or severe lymphoedema, your skin may start to break down and leak fluid. Contact your doctor straight away if this happens.
If you have lymphoedema, you’re more likely to develop a skin infection called cellulitis. Cellulitis requires quick medical treatment with antibiotics for at least two weeks. For more information, see our section on living with lymphoedema.
Diagnosis of lymphoedema
It’s important that lymphoedema is diagnosed as soon as possible so you can get the right type of treatment.
Your GP will usually be able to tell if you have lymphoedema based on your symptoms, how the affected area looks, and your medical history. They’ll refer you to a lymphoedema therapist (often a nurse or physiotherapist), to confirm your diagnosis and manage your treatment.
Measuring volume
A lymphoedema therapist will examine the affected area to check the swelling and any changes to your skin. They may measure around the affected area using a tape measure. If your arm or leg is affected, they may compare it to the unaffected side. They’ll also compare measurements over time, or after treatment.
Other methods your lymphoedema therapist may use to measure the size of the swelling include:
- perometry, which uses an infra-red light
- bioimpedance spectroscopy, which uses an electrical current to measure water content in affected tissues
Other scans and tests
You may need other scans and tests to confirm the diagnosis, often at the recommendation of a lymphoedema specialist doctor. These include the following.
- A lymph scan (lymphoscintigraphy or lymphoscintigram, pronounced lim-fo-sin-ti-gram). This involves having an injection of a radioactive dye, which is tracked on scans over a period of two hours. The scan will show if there are any areas where lymph isn’t flowing properly.
- MRI scan, CT scan or ultrasound.
- Genetic testing. This can help diagnose primary lymphoedema.
Treatment of lymphoedema
While there isn’t a cure for lymphoedema yet, lymphoedema treatments can manage and improve your symptoms and reduce your risk of complications such as a cellulitis infection. This includes reducing swelling, stopping more fluid building up, looking after your skin, and reducing any discomfort. You may have a combination of different lymphoedema treatments, usually in a specialist lymphoedema clinic.
There are four main elements to lymphoedema treatment:
- skin care
- weight management
- exercise and movement
- compression
Manual lymphatic drainage massage may be helpful to some patients with lymphoedema, but is rarely recommended on a regular basis
Skin care
Your lymphoedema therapist will teach you how to look after your skin and keep it in good condition, with regular bathing and moisturising. This is important to reduce your risk of damaging your skin and developing infections. For more information on skin care, see our section on living with lymphoedema.
Weight management
One of the best ways to reduce swelling is to maintain a normal healthy weight. If you’re overweight it’s important to take steps to reduce this excess weight. Your GP practice may be able to help you.
Lymphoedema exercises
Exercise is a very important part of managing lymphoedema. Tensing and flexing your muscles as you move helps lymph to move around your body, especially if you are wearing a compression garment at the time. Exercise will also help you to maintain a healthy weight, which is another important part of managing lymphoedema.
Your lymphoedema therapist can advise you on a programme of exercise and movement to help you.
Compression treatment
Compression means wearing fitted, elastic compression garments, bandages or adjustable wraps, to reduce swelling.
Complete decongestive therapy (CDT), also known as Decongestive Lymphatic Therapy (DLT), is considered to be the best way to treat lymphoedema. CDT is divided into two parts or phases:
- an intensive or decongestive phase, which generally lasts for several weeks, and is aimed at reducing significant swelling
- a maintenance or long-term self-management phase, where you care for yourself and maintain the improvements by wearing compression garments every day, as well as exercise and maintain a healthy body weight
If your lymphoedema is severe, your therapist may suggest an intensive treatment course using a system of bandages (multi-layer bandaging) to reduce your swelling. They are applied several times a week for two or more weeks, depending on the severity of your lymphoedema. This is thought to be the most effective type of compression to reduce a large arm or leg down to a manageable size. Once the size and shape of the swelling has improved, you can start to wear compression garments instead to maintain the results of the intensive compression bandaging.
If your lymphoedema is mild to moderate, then you may not need daily bandaging, but be able to go straight into wearing a compression garment every day. This may be a sleeve, stocking, glove, or something else depending on where the swelling is. You’ll usually wear it all day but can take it off at night.
Other treatments
Specialised lymphatic massage techniques
Manual lymphatic drainage (MLD) massage can help to move lymph away from swollen areas and around your body. It should be combined with compression to help reduce swelling and maintain the results. Your lymphoedema therapist can teach you how to massage yourself, or a relative or carer can do it for you.
Intermittent pneumatic compression
Sometimes, your therapist may suggest you use pneumatic compression. This provides compression by using a pump device to inflate a cuff around the affected area of your body.
Your clinic may offer certain other treatments too, which may include the following.
- Kinesio taping to help drain fluid and reduce swelling in lymphoedema. This is a technique commonly used for sports injuries.
- Laser therapy, which has been reported to soften the hard fibrotic areas that can build up in chronic lymphoedema.
Not all of these treatments are widely available, so they may not be offered at your clinic.
Liposuction
Your doctor or therapist may suggest surgery to help manage your symptoms in the long term but this is rare. Liposuction, for example, may help to reduce the volume of fat in an affected arm or leg (chronic poorly controlled lymphoedema can encourage fat to build up in the limb, and this fat cannot be removed by compression). You’ll need to wear very strong compression 24 hours a day for the rest of your life after liposuction. This will help with the swelling after the surgery and help to maintain the results.
Living with lymphoedema
Whether you’re at risk of lymphoedema or already have a diagnosis, there are things you can do to look after yourself. This might prevent you developing lymphoedema, or stop it from getting any worse.
Keep in contact with your medical team
Attend check-ups with your doctor or therapist. Between check-ups, let them know about any changes in parts of your body that are affected or at risk. This could be increased swelling, or changes in your skin or sensation in your body.
Keep to a healthy weight and exercise
It’s important to keep your weight at a healthy level to prevent and manage lymphoedema. A key part of this is to keep active and do some regular exercise. Exercise will help you to manage your symptoms, as well as keep your weight under control. If you’re overweight, it’s a good idea to lose the excess weight because it may improve your symptoms.
If you have questions about what diet or type of exercise would be best for you, speak to your doctor or lymphoedema specialist.
Know the signs of cellulitis
If you have lymphoedema, you’re at greater risk of developing a skin infection called cellulitis. This is not the same as cellulite (harmless dimpled skin). Symptoms of cellulitis can include:
- redness or a rash
- swelling
- a feeling of warmth
- pain
- a fever or flu-like symptoms
It’s important to watch out for early signs of cellulitis. Call 111 or contact your GP as soon as possible if you think you may have the infection.
Look after your skin
Keeping your skin clean, well moisturised, and protecting it from damage will help to prevent an infection. Here are some tips.
- Wash your skin with warm water. Carefully dry it (especially between fingers and toes) and moisturise every day. Your therapist may recommend some moisturising creams.7
- Dry carefully between your toes after washing and look out for signs of athlete’s foot. Treat this quickly with athlete’s foot cream for two weeks, as it can cause splits in the skin which lets in bacteria that cause cellulitis infections.
- Take care when you cut your nails and don’t cut your cuticles. Consider having your toenails cut professionally if you have severe lymphoedema of the feet.
- Wear insect repellent to help prevent insect bites.
- Wear gloves when gardening and doing housework or DIY.
- Don’t walk around barefoot or wear shoes that give you blisters.
- If you do get a cut or graze, clean and dry it well and put some antiseptic cream over the area.
- Wear sun protection so you don’t get sunburnt.
- Use an electric razor if you wish to remove hair.
Other self-care measures
Other steps to reduce lymphoedema symptoms include the following.
- Don’t put pressure on the affected body part. For example, don’t wear jewellery or clothing that’s too tight because it can block the flow of lymph.
- Try not to sit or stand in one position for a long time – for example, on long journeys. Move around often and do some gentle stretches. Part of living with lymphoedema in your legs is if they’re swollen, elevate them when you sit. You could rest your legs up on a cushion, for example.
- Don’t spend too long in extreme cold or heat, such as in hot tubs, saunas, or by sitting close to a fire.
- If one of your arms is affected, don’t have injections, blood tests or your blood pressure taken in that arm (if possible). Tell any health professional you see about your lymphoedema.
The main cause of lymphoedema is a problem with your lymphatic system. This causes lymph (fluid) to build up in the affected part of your body. There are many things that can cause lymphoedema, including cancer treatment, infections and injury. Sometimes there’s no particular cause – it’s just something you’re born with.
See our causes of lymphoedema section for more information.
Lymphoedema isn’t cancer. But it can develop following treatment for cancer, or rarely, because of cancer. Cancer treatments, such as surgery and radiotherapy on your lymph nodes can disrupt the normal flow of lymph. Sometimes, cancer itself can spread to your lymph nodes, which can lead to a blockage.
The best treatment for lymphoedema is usually a combination of treatments, including compression, exercise, weight management, and skin care. Some people might have surgery. It’s important to seek medical help as soon as possible if you have lymphoedema symptoms because lymphoedema is easier to treat at an early stage.
See our treatment of lymphoedema section for more information.
One of the first signs of lymphoedema is swelling in part of your body, most often in an arm, leg, hand, foot. Your leg or arm may feel heavy or weak, and you may notice that your skin looks pitted. Later signs include severe swelling and the swollen area may turn very hard and solid.
See our symptoms of lymphoedema section for more information.
The first stage of lymphoedema is mild swelling in part of your body, usually an arm, leg, hand, foot. You might only notice it towards the end of the day or if your clothing or jewellery feels tight. Seek medical help straightaway so you can start treatment. If you don’t get treatment, lymphoedema can progress to an advanced stage where the swelling gets worse and more constant. In very advanced or severe lymphoedema, your skin may start to break down and leak fluid.
See our symptoms of lymphoedema section for more information.
Other helpful websites
Discover other helpful health information websites.
Did our Lymphoedema information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Lymphoedema. BMJ Best Practice. bestpractice.bmj.com, last updated 8 February 2022
- Guidelines on the management of cellulitis in lymphoedema. British Lymphology Society and the Lymphoedema Support Network. www.thebls.com, published October 2022
- What is lymphoedema? Lymphoedema Support Network. www.lymphoedema.org, last reviewed October 2022
- Sleigh BC, Manna B. Lymphedema. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 19 April 2023
- Skin care for lymphoedema. Macmillan. www.macmillan.org.uk, reviewed 1 March 2023
- Lymph facts. British Lymphology Society. www.thebls.com, reviewed May 2023
- Lymphedema. Medscape. emedicine.medscape.com, updated 18 April 2023
- Lymphoedema. Macmillan. www.macmillan.org.uk, reviewed 1 March 2023
- Just diagnosed? Lymphoedema Support Network. www.lymphoedema.org, last reviewed October 2022
- Lymphatic drainage for lymphoedema. Macmillan. www.macmillan.org.uk, reviewed 1 March 2023
- Managing lymphoedema with physical activity. Macmillan. www.macmillan.org.uk, reviewed 1 March 2023
- Compression treatment for lymphoedema. Macmillan. www.macmillan.org.uk, reviewed 1 March 2023
- Types of treatment for lymphoedema. Cancer Research UK. www.cancerresearchuk.org, last reviewed 11 April 2023
- Managing and treating lymphoedema. Macmillan. www.macmillan.org.uk, reviewed 1 March 2023
- Liposuction for chronic lymphoedema. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 27 April 2022
- Bass LS, Kaminer MS. Insights into the pathophysiology of cellulite: a review. Dermatol Surg 2020; 46(1):S77–85. doi: 10.1097/DSS.0000000000002388
- Reducing your risk of lymphoedema. Macmillan. www.macmillan.org.uk, reviewed 1 March 2023
- Lymphedema: the basics. OncoLink. www.oncolink.org, last reviewed 11 July 2022



