Tummy tuck (abdominoplasty)
- Mr Baljit Dheansa, Consultant Plastic Surgeon
A tummy tuck (abdominoplasty) is cosmetic surgery to take away loose skin and fat from your tummy. It may also bring your tummy muscles together. You may have liposuction at the same time, to help shape your tummy.
When is a tummy tuck necessary?
People have a tummy tuck for many different reasons. You may have it as part of another operation such as a hernia repair. Or you may want one because you have:
- loose skin after you’ve lost a lot of weight
- loose skin and muscles after pregnancy
- scars on your tummy from earlier surgery or an injury (as long as you also have loose skin so the tummy tuck can be done)
Tummy tuck surgery may make the shape of your tummy look better – by taking away extra fat and skin and bringing your tummy muscles together. It is a plastic surgery procedure to give you a flatter, smoother abdomen.
You’ll need to be as close to a healthy body weight as possible before your tummy tuck. Your GP or practice nurse may be able to advise you about this. Having a tummy tuck can’t help you to lose or control your weight.
Also, to get the best long-term result from this surgery, you should keep your weight healthy afterwards. You may not have a completely flat tummy following the procedure.
Who may not be able to have tummy tuck surgery?
You may not be able to have tummy tuck surgery if you:
- are a smoker
- are overweight
- have had blood clots in the past
- are planning to get pregnant in the future
- have heart disease or diabetes that isn’t controlled properly
- have body dysmorphia – when you think there’s something wrong with how you look, even though there isn’t
- don’t have very much loose skin
A plastic surgeon will be able to tell you if the surgery is right for you.
Getting tummy tuck information and advice
Getting the right advice before having a tummy tuck is important. You need to have a good think about:
- what you’re hoping to gain from surgery
- what is and isn’t possible
- the risks involved
- the aftercare
- the recovery time after surgery
If you decide to have tummy tuck surgery, it’s important to choose your surgeon carefully. You’ll need to make sure you find someone with the right training and qualifications. Your GP may be able to refer you to a suitable surgeon who works near you. Or they may give you advice on how to find one.
You should be happy with the hospital where you will be having the operation. You will also need to know about the care you will get after the surgery and what happens if anything goes wrong. You can ask your surgeon for this information.
Take your time to decide whether or not to have a tummy tuck. It isn’t essential surgery. So, you should think about how you’d feel and cope if there was a complication or something went wrong.
Make sure you see the surgeon who’ll be doing your operation before signing up. You should be given a ‘cooling off’ period of at least a couple of weeks before having surgery. If you still have questions after this, it may help to have a second consultation with your surgeon.
If you decide to go ahead, you’ll be asked to sign a consent form. It’s important to make sure you feel properly informed before signing this, and your surgeon should give you information in writing about the operation and its risks. You can change your mind at any time before your procedure.
Preparing for a tummy tuck
Your surgeon will explain how to get ready for your operation.
If you smoke, you’ll need to stop smoking at least six weeks before your surgery. Smoking makes you more likely to get a complication after surgery. It may also make your wounds heal more slowly. So it may take you longer to recover after your surgery.
Your surgeon may advise you to:
- lose some weight – you should be as close to the ideal weight for your height as possible before your operation
- stop taking the contraceptive pill around four weeks before your operation, so that you’re less likely to get a blood clot – make sure you use another form of contraception
If you’re overweight, you may be more likely to have complications after surgery than if you’re a healthy weight before surgery.
You’ll have your tummy tuck surgery under general anaesthesia. This means you’ll be asleep during the operation. You’ll usually have to stop eating or drinking for a few hours before your surgery. Your surgeon or anaesthetist will give you clear advice on what to do.
Your surgeon will explain what will happen before, during, and after your operation. This is your chance to ask any remaining questions you have about your surgery. You’ll be asked to sign the consent form.
Your surgeon may provide compression garments for you to wear after the surgery. These will need to be the right size for you, so you should ask about these special clothing items before the operation. Compression garments can help with your recovery, by reducing swelling, for example.
What are the alternatives to tummy tuck?
Liposuction may be helpful if you’re not generally overweight and want to get rid of some fat from specific parts of your body. But a surgeon may not be able to tell you how well liposuction will work before you have it. Liposuction can lead to loose skin, especially if there are stretch marks, so your surgeon may not recommend it. When you have liposuction, your surgeon uses a tube to suck out any extra fat that’s under your skin.
You can have liposuction on its own, or you can have it as part of a tummy tuck procedure. Liposuction can help to change the shape of your tummy. But it only takes away unwanted fat. A tummy tuck takes away unwanted fat and skin, and can bring your tummy muscles together.
You could have no surgery – then you’d avoid the cost, risks, pain, and recovery time that come with tummy tuck surgery. Your surgeon can tell you about alternatives to having a tummy tuck. They can also advise you about any risks or complications that might come with these.
The alternatives are known as non-surgical tummy tucks. A skin-tightening therapy, for example, may help with mild skin excess. Body-contouring devices help to reduce fat, tighten skin, and bring muscles together. These include high-intensity focused ultrasound, laser therapy and cryolipolysis (using freezing temperature to destroy fat).
It may help to see a clinical psychologist to discuss:
- how you feel about your body
- how to feel more comfortable about how you look
What happens during a tummy tuck?
There are several different types of tummy tuck surgery. Your surgeon will explain which one is best for you. This may depend on how much skin and fat you want taken away. It may also depend on whether or not you want a smaller tummy tuck scar.
Most tummy tuck operations take around three hours.
Standard tummy tuck
Your surgeon will make a cut from one hip to the other along your pubic area. In women, this is called your bikini line. Then they’ll:
- make another cut around your belly button to free it from the surrounding skin
- take away extra fat and skin and bring your tummy muscles together
- pull the remaining skin down and make a new hole, so your belly button’s in the right place
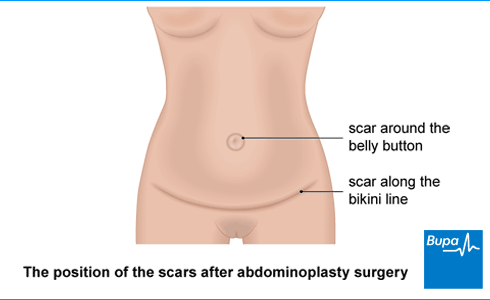
You’ll have a scar around your belly button and a long, curved scar on your tummy above your pubic area. Because of the normal pattern of pubic hair, the scar is generally higher in men than in women. These scars are usually (but not always) hidden by underwear or swimwear.
The picture below shows an example of where your scars will be after a tummy tuck. This varies from person to person and with the type of tummy tuck. Your surgeon will explain the tummy tuck scar you’re likely to have.
Mini tummy tuck
If you only need a small amount of skin or fat taken away, you may be able to have a mini tummy tuck.
Your surgeon will take away any unwanted skin and fat from your lower tummy.
Afterwards, you’ll have a curved scar above your pubic area. This may be slightly shorter than with a standard tummy tuck. Your belly button stays in the same place, but it may be a slightly different shape.
What to expect after a tummy tuck
You may be in hospital for up to three days after surgery.
When you wake up, you’ll have dressings over your lower tummy. You may also have thin tubes (drains) coming out of your wound to take away any fluid. These are usually taken out before you go home. Some surgeons may use newer techniques that don’t need drains. You may have a drip in your arm for fluids and medicines. This is usually taken out as soon as you can drink enough fluids.
You may feel a bit sore after a tummy tuck, so your surgeon or anaesthetist will prescribe painkillers.
You’ll go home with your stitches in. Most surgeons use stitches that dissolve by themselves. Your nurse or doctor will tell you:
- how long this will take
- how to care for your wound
- if you need compression garments
- if you need to come back to have any non-dissolvable stitches taken out
- about any other after-care you might need and how to contact them
You'll need someone to drive you home. Try to have a friend or relative stay with you for at least 24 hours when you get home after your tummy tuck.
You mustn’t drive, drink alcohol, use machinery, or sign legal documents for 24 hours after you’ve had a general anaesthetic. It’s important to ask your surgeon about what you should be able to do – and what you can’t do following the surgery. They can also tell when you should be able to drive again, based on the Driver and Vehicle Licensing Agency (DVLA) guidance. You should also check with your motor insurer.
You may have any of the following.
- Pain, bruising, and swelling, which will start to get better after a few days. Most swelling should go away after a few months.
- Scars, which will be very noticeable for the first few weeks. But then they’ll start to fade and blend in more with your normal skin tone. Tummy tuck scars don’t always disappear completely. Some people are more likely to have more noticeable scars.
- Numbness, because some of your nerves may be cut during a tummy tuck. Nerves heal very slowly, so it often takes months to get better. The numbness may not go away completely.
Recovering from a tummy tuck
After a tummy tuck, it’s important not to do too much too soon. The key is to pace yourself.
It usually takes about six weeks to recover, but everyone’s different. Your tummy tuck recovery time may depend on which operation you’ve had, so follow your surgeon's advice. What they recommend is important, to help with your wound healing, pain, and swelling. If you work, you’ll likely need about four weeks off.
When you get home, you may be advised to rest in bed for another day or two, but you should get up to use the toilet. You’ll recover faster if you’re up and about as soon as you feel well enough.
Avoid doing anything that strains your tummy muscles. You can roll onto your side to get out of bed, for example.
If you need to, you can take over-the-counter painkillers, such as paracetamol or ibuprofen. Always read the leaflet that comes with your medicine. If you have any questions, ask your pharmacist for advice.
Your surgeon may ask you to wear a support garment (a type of corset) for up to six weeks after surgery. This helps to ease pain and discomfort, and to reduce swelling.
Exercises you can do after a tummy tuck
The hospital should tell you how much exercise to do and how long it will take to get back to normal. Your surgeon or physiotherapist may recommend suitable exercises and when to start doing them.
Take things slowly. You should be back to normal exercise in around six weeks. If you’re doing anything that pulls on the tummy tuck scar and it feels like it’s stretching, take it a little slower. Your abdominal muscles protect your back when you lift, so you need to be careful until they’ve healed.
Your surgeon will advise on when you can start doing the following activities.
- Start with gently walking around at home.
- Go up and down stairs if it’s not too sore.
- Start doing light activities, such as making drinks or light meals.
- Once you’re comfortable around the house, gradually build up to longer walks of 5 to 10 minutes.
- Avoid vigorous activity (including sports) or heavy lifting (including shopping) for up to 12 weeks.
- Don’t have sex for three weeks after surgery.
- Don’t drive for a time. Ask your surgeon about this – they may recommend waiting two or three weeks, but it can be up to six weeks. Don’t drive when wearing a seatbelt is uncomfortable.
- Don’t do sit-up type exercises for at least six weeks and then take it slowly.
Once you have the go-ahead from your surgeon, you can do exercises to strengthen your tummy muscles. But don’t exercise before checking with your doctor because every operation and patient is different.
What are the complications?
Like all types of surgery, a tummy tuck can cause some complications. These complications include:
- an unexpected reaction to the anaesthetic, including an allergic reaction
- a lot of bleeding
- getting a blood clot, usually in a vein in your leg (deep vein thrombosis, DVT)
Other complications of a tummy tuck include:
- an infection – this may need antibiotics
- bleeding under your skin (haematoma) – you may need more surgery to stop the bleeding and drain the area
- seroma – a collection of fluid around your wound that may need draining with a needle and syringe
- unusually red or raised scars – these may take several months to fade
- a blood clot in your lungs (pulmonary embolus)
- damage inside your body – for example, to your blood vessels, muscles or bowel – this may be temporary or permanent and may mean you need more surgery
- loose skin and fat between your tummy tuck scar and new belly button
- your body not looking the same on both sides – this is called asymmetry
- bulges at the ends of your scar – these may need more surgery to fix them
- deep stitches poking out of your skin in the weeks after your surgery – these can be removed easily by the surgeon
- problems with wound healing – these can slow down your recovery and cause more noticeable scars
- pins and needles, a burning sensation, numbness, or pain on touching your skin – this is because nerves can get damaged during the operation; this may be permanent in some people.
If you smoke, you may be more likely to have complications after surgery. You’re also more likely to have complications if you have diabetes. Your surgeon will want to make sure your diabetes is under control before and after surgery. Talk to your surgeon if you’re at all worried.
Sepsis (adults)
Some people are at higher risk of getting sepsis after surgery. Sepsis is a life-threatening complication that can develop if you get an infection. Sepsis is a medical emergency. Call 999 or go to A&E immediately if you have any of the following symptoms.
- Slurred speech, confusion, difficulty making sense.
- Extreme shivering or muscle pain.
- Passing no pee (urine) during a day.
- Severe difficulty breathing, feeling breathless, or breathing very fast.
- It feels like you’re going to die.
- Skin changes, such as your skin looking blue, pale or blotchy, or a rash that does not fade when you roll a glass over it.
A tummy tuck (abdominoplasty) is cosmetic surgery to take away loose skin and fat from your tummy. It may also bring your tummy muscles together.
Tummy tuck scars usually fade over 12 to 18 months but won't go away completely. For the first few weeks they’ll be very noticeable. But then they should start to blend in more with your normal skin tone. For more information, see our section on what to expect after a tummy tuck.
Not everyone can have a tummy tuck. The surgery may not be right for you if you’re a heavy smoker, are very overweight or have had blood clots in the past. For more information, see our section on who may not be able to have tummy tuck surgery.
You will have some soreness in the area following a tummy tuck but this is easily controlled. Your anaesthetist or other hospital doctor will be able to discuss the pain relief options with you and write you a prescription for painkillers.
A tummy tuck is a permanent operation and the results should stay with you for the rest of your life. Remember, the results are best if your weight stays stable.
General anaesthesia
General anaesthesia is when medication is given to make you temporarily unconscious during an operation, so don't feel pain or other sensations.
Healthy weight for adults
Weighing too much or too little can increase your risk of several diseases, including heart disease, diabetes and cancer
What’s the safest way to lose weight?
Read on to understand what you can do to lose weight safely. We also give some tips to help you put your plan into action.
Tips for a healthy and well-balanced diet
A healthy, well-balanced diet involves eating foods from a variety of food groups to get the nutrients that your body needs to function.
Tools and calculators
BMI calculator
BMI, or body mass index, is one way of measuring whether you’re a healthy weight for your height.
Simply enter your details into our calculator and the result will give you an indication of whether you're a healthy weight.
Calories calculator
If you want to lose weight, you need to increase your physical activity and watch your calorie intake. Bupa's calorie calculator will help you to work out how many calories you're burning in a day.
Did our Tummy tuck (abdominoplasty) information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Tummy Tuck (Abdominoplasty). British Association of Aesthetic Plastic Surgeons. baaps.org.uk, accessed April 2024
- Abdominoplasty. Background. Medscape. emedicine.medscape.com, updated April 2022
- Information for Commissioners of Plastic Surgery Services. Page 13: Body Contouring Procedures: Tummy tuck. NHS Modernisation Agency: Action on Plastic Surgery. bapras.org.uk, accessed April 2024
- Phan R, Kaplan E, Porrett JK, et al.. Incisional abdominal hernia repair with concomitant abdominoplasty: Maintaining umbilical viability. JPRAS Open 2018; 16:100–4. doi: 10.1016/j.jpra.2017.09.002
- Abdominoplasty. Etiology. Medscape. emedicine.medscape.com, updated April 2022
- Abdominoplasty. Indications. Medscape. emedicine.medscape.com, updated April 2022
- Abdominoplasty. Contraindications. Medscape. emedicine.medscape.com, updated April 2022
- Higgins S, Wysong A. Cosmetic Surgery and Body Dysmorphic Disorder – An Update. Int J Womens Dermatol 2017; 4(1):43–8. Published 2017 Nov 20. doi:10.1016/j.ijwd.2017.09.007
- BAAPS Consumer Safety Guidelines. British Association of Aesthetic Plastic Surgeons. baaps.org.uk, accessed May 2024
- Considering cosmetic surgery. British Association of Aesthetic Plastic Surgeons. baaps.org.uk, accessed May 2024
- Good surgical practice. Consent. The Royal College of Surgeons. rcseng.ac.uk, accessed May 2024
- Abdominoplasty. Presentation. Medscape. emedicine.medscape.com, updated April 2022
- Contraceptives, hormonal. NICE British National Formulary. bnf.nice.org.uk, accessed May 2024
- Abdominoplasty. Complications. Medscape. emedicine.medscape.com, updated April 2022
- Anaesthesia Explained. Types of anaesthesia. Royal College of Anaesthetists. rcoa.ac.uk, published March 2021
- Anaesthesia Explained. On the day of your operation. Royal College of Anaesthetists. rcoa.ac.uk, published March 2021
- Abdominoplasty. British Association of Plastic Reconstructive and Aesthetic Surgeon. bapras.org.uk, accessed January 2022
- Mazzoni D, Lin MJ, Dubin DP, et al. Review of non-invasive body contouring devices for fat reduction, skin tightening and muscle definition. Australas J Dermatol 2019; 60(4):278–83. doi: 10.1111/ajd.13090
- What is fat freezing and what are the risks? BBC. bbc.co.uk, published September 2021
- Abdominoplasty. Surgical therapy. Medscape. emedicine.medscape.com, updated April 2022
- Surgical drains. Patient. patient.info, last reviewed October 2021
- Plastic surgery. Suturing wounds. Oxford Handbook of Clinical Surgery (online). 5th ed. Oxford Medicine Online. oxfordmedicine.com, published online November 2021
- Surgery. Recovery after surgery. Oxford Handbook of Adult Nursing (online). 2nd ed. Oxford Medicine Online. oxfordmedicine.com, published online June 2018
- Caring for someone recovering from a general anaesthetic or sedation. Royal College of Anaesthetists. rcoa.ac.uk, published November 2021
- Assessing fitness to drive – a guide for medical professionals. Driving after surgery. Page 123. Driver and Vehicle Licensing Agency. gov.uk, updated February 2024
- Ducic I, Zakaria HM, Felder JM, et al. Abdominoplasty-Related Nerve Injuries: Systematic Review and Treatment Options. Aesthetic Surg J 2014; 34(2):284–297. academic.oup.com, published February 2014
- Liposuction. Post-operative care. Oxford Handbook of Clinical Surgery (online). 5th ed. Oxford Medicine Online. oxfordmedicine.com, published online November 2021
- Abdominoplasty. Other tests. Medscape. emedicine.medscape.com, updated April 2022
- Sepsis. Patient. patient.info, last updated February 2024
- What is sepsis? sepsistrust.org, accessed 26 May 2024
- Sepsis: risk stratification for adults, children, and young people with suspected sepsis. National Institute for Care and Health Excellence. cks.nice.org.uk, last updated February 2024
- Abdominoplasty (tummy tuck). my.clevelandclinic.org, last reviewed January 2024
- Personal communication, Mr Baljit Dheansa, Consultant Plastic Surgeon, September 2024
- Markus MacGill, Content editor



