Warts and verrucas
Your health expert: Dr Veronique Bataille, Consultant Dermatologist
Content editor review by Pippa Coulter, Freelance Health Editor, January 2023
Next review due, January 2026
Warts and verrucas are small, rough lumps or growths on your skin. A wart on the sole of your foot is sometimes called a verruca. Many people get a wart or verruca at some point in their lives. They’re most common in school-age children and teenagers.
Types of warts and verrucas
There are many different types of wart. There are differences in how they look and where they’re normally found on your body. We list some of the most common types affecting the skin on your hands, feet and other parts of your body below. We don’t include genital warts here. Genital warts are a sexually transmitted infection and are treated differently to the other types of warts.
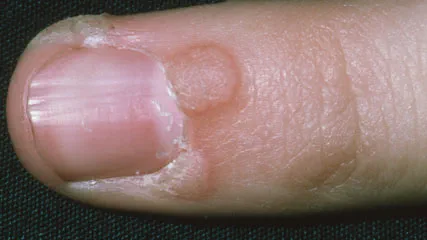
Common wart
These are firm, raised growths with a rough surface – they might look like a very small cauliflower. They’re normally greyish-white or light brown, and usually a few millimetres across. This type of wart is most commonly found on your hands, fingers or knees.
Verruca (plantar wart)
Verrucas are warts on the soles of your feet. They may have tiny black dots in the centre – these are blood clots that have formed in tiny blood vessels. They may be painful, especially when you put weight on them. Sometimes, if you have clusters of verrucas, they can fuse together. These are called mosaic warts.
Plane wart (flat wart)
Plane warts are round, smooth and slightly raised, with a flat top. They can be slightly brown, greyish-yellow or skin-coloured. They’re most common on your face and the backs of your hands. You will often have more than one at a time.
Filiform wart
These have a finger-like appearance, sometimes with a stalk. They’re most commonly found on your face or neck.
Causes of warts and verrucas
Warts and verrucas are caused by infection of your skin with the human papillomavirus (HPV). They can spread from person to person by direct skin contact. But the risk of them spreading is usually fairly low. They’re more likely to spread if you damage the top layer of the wart, as this exposes the virus more.
They can also spread indirectly, if you touch something, like a floor or surface that’s been contaminated with HPV. But this is less common. You’re more likely to get infected this way if your skin is damaged or wet, so infection is often linked to swimming pools and communal showers. You can also spread the infection from one part of your body to another, if you scratch or touch a wart or verruca.
You’re more likely to develop warts and verrucas if you have a weakened immune system. This might be because you have a medical condition or are taking medicines that suppress your immune system.
Symptoms of warts and verrucas
You might not like how your warts look, especially if they’re on your hands or face. But apart from their appearance, warts and verrucas don’t usually cause any symptoms. Verrucas can become uncomfortable or painful when you put weight on them. They may also bleed. Common warts around your nails can be painful too.
Self-help for warts and verrucas
Most warts and verrucas go away by themselves, so it’s often best just to leave them alone, especially in children. But if your wart or verruca is bothering you, there are some things you can try at home to help get rid of it. It’s important to be aware that these don’t always work.
Duct tape
Some people believe that placing duct tape over a wart or verruca helps to get rid of it. There’s no clear explanation as to how this might work. It might be that the tape cuts off the oxygen supply to the wart or verruca. Or, the tape may irritate the skin, encouraging the body’s immune system to fight off the virus.
There’s not enough evidence to support using this technique. But it shouldn’t do any harm, so you may want to give it a try. If you do decide to try it, follow these steps.
- Cover your wart or verruca with duct tape for six days. If it falls off, just replace it with a new piece.
- On the seventh day, remove the tape, soak the wart in water and rub with an emery board or pumice stone.
- Keep the wart uncovered overnight and re-apply fresh duct tape the next day.
- Continue this cycle for up to two months, until the wart disappears.
Over-the-counter wart and verruca treatments
There are treatments available for warts and verrucas that you can buy from a pharmacy or shop. You apply these yourself at home. They don’t always work. They can also be time-consuming, painful and cause side-effects. But if your wart or verruca is bothering you, you may want to consider trying them. See our, Treatment section for more information. You can ask a pharmacist if you need any advice.
When to seek help for warts and verrucas
You don’t usually need to see your GP about warts or verrucas. Warts and verrucas are usually harmless and go away by themselves without treatment. In children, about two-thirds disappear within two years. Some disappear much quicker than this – within a few months. It may take up to five to 10 years for warts and verrucas to clear up in adults.
There are some circumstances when you should see your GP, though. Always see your GP if you have a new growth on your skin and you’re not sure what it is, especially if it’s growing rapidly. Your doctor will usually be able to tell if it’s a wart just by looking at it and examining it.
You should also see your GP if:
- the wart or verruca is painful or bleeding
- you have a wart on your face
- you have lowered immunity – this can make it harder to get rid of the wart without treatment
- you have lots of warts covering a large area
Treatment of warts and verrucas
Some wart and verruca treatments you can buy over the counter from a pharmacy or shop. You apply these yourself at home. Other wart removal treatments are carried out by a GP or specialist doctor.
Wart and verruca creams and gels
There are many creams, gels and medicated plasters for treating warts and verrucas. You can buy these over the counter at a pharmacy. If you see a GP about a wart or verruca, they will usually suggest this first too.
Many of these treatments contain an ingredient called salicylic acid. This is a chemical that helps to break down the skin on your wart or verruca. This triggers your immune system to clear the virus. It may provide some help in getting rid of warts or verrucas. If you decide to try a salicylic acid preparation, the following tips may help.
- Don’t use salicylic acid preparations on your face or large areas of skin. This is because it can cause irritation and scarring.
- Check with your pharmacist or doctor before using it if you have diabetes and are prone to ulcers or have nerve damage.
- Before applying the treatment, soften the wart by soaking it in water and rubbing it with an emery board or pumice stone to remove any excess hard skin.
- Try to get as little as possible of the treatment on the surrounding area because it can cause irritation to healthy skin. Protect the skin around the wart with petroleum jelly or soft paraffin. Avoid getting the treatment on broken skin.
- Once the treatment has dried, it may help to cover the wart with a plaster or simple dressing.
- You may need to use the treatment daily for up to three months. If your wart is becoming very sore though, stop the treatment for a few days and then restart.
Cryotherapy
Cryotherapy is the process of freezing your wart using liquid nitrogen so it falls off. Your doctor applies the liquid nitrogen to your wart using either a spray or a cotton bud. It takes between five and 30 seconds. You usually need to repeat the treatment every two to three weeks until the wart has gone, up to a maximum of six times. It sometimes leads to blistering or scarring of your skin and can be painful, so it is not recommended for younger children.
There’s some evidence that cryotherapy may help to remove warts and verrucas, but it hasn’t been shown to work any better than salicylic acid treatment. Not all GP practices carry out cryotherapy. And depending on where you live, it’s not always available on the NHS for wart and verruca treatment. This means you may need to pay to have the treatment privately.
There are over-the-counter cryotherapy preparations that claim to remove warts and verrucas. These are a type of cryotherapy that you apply yourself at home. You can buy them at a pharmacy. They contain other gases that act to freeze the wart or verruca. However, there is very little evidence to support their use. They can’t freeze at temperatures as low as liquid nitrogen, so they’re unlikely to work as well.
Specialist treatments
Your GP may sometimes refer you to a dermatologist or specialist skin clinic for treatment. This might be if you have large areas of skin affected, warts on your face or a weakened immune system.
Your dermatologist may suggest various different options for wart removal. These include stronger medications that you either take by mouth, apply to your skin or are injected into the wart.
Surgery and laser treatment aren’t used very often for wart removal, as the warts can come back after these procedures. They can also be painful and leave a scar. If used, your doctor may recommend combining these with other treatments.
Prevention spread of warts and verrucas
If you have a wart or verruca, taking the following measures may help to stop it spreading to other people.
- Don’t scratch or pick your wart or verruca as it’s more likely to spread.
- If you have warts on your fingers, don’t bite your nails or suck your fingers.
- If you use nail files or pumice stones on your wart or verruca, don’t share these or use on other areas of your skin.
- Avoid shaving in areas where you have warts, and disinfect your razor after every use.
- Keep your feet clean and dry. See a chiropodist or podiatrist if you find it difficult to do this. Change your socks every day.
- Wear flip-flops in communal showers and changing rooms.
- Cover your wart or verruca with a waterproof plaster when you go swimming. Swimming socks are not needed.
- Don’t share your towels, shoes or socks.
There’s no reason why you can’t continue to take part in activities, such as sports or swimming, if you have a wart or verruca. But make sure you follow the advice above to avoid passing it on to other people.
Other helpful websites
Discover other helpful health information websites.
Did our Warts and verrucas information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Warts and verrucae. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised February 2020
- Plantar warts (verrucas). British Association of Dermatologists. www.bad.org.uk, updated November 2018
- Al Aboud AM, Nigam PK. Wart. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 8 August 2022
- Suspected cancer: recognition and referral. National Institute for Health and Care Excellence. www.nice.org.uk, last updated 15 December 2021
- Viral warts. British Association of Dermatologists. www.bad.org.uk, produced September 2021
- Common warts. BMJ Best Practice. bestpractice.bmj.com, last reviewed 29 October 2022
- Kwok CS, Gibbs S, Bennett C, et al. Topical treatments for cutaneous warts. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No.: CD001781. DOI: 10.1002/14651858.CD001781.pub3
- Dermatology. Oxford handbook of general practice. Oxford Academic. academic.oup.com, published online June 2020
- Nguyen NV, Burkhart CG. Cryosurgical treatment of warts: dimethyl ether and propane versus liquid nitrogen – case report and review of the literature. J Drugs Dermatol 2011; 10(10):1174–76
- Genital warts. BMJ Best Practice. bestpractice.bmj.com, last reviewed 24 October 2022
- Personal communication, Dr Veronique Bataille, Consultant Dermatologist, 20 January 2023



