Inner (medial) knee pain
Your health expert: Mr Damian McClelland, Trauma and Orthopaedic Consultant, and Clinical Director for Musculoskeletal Services at Bupa
Content editor review by Rachael Mayfield-Blake, Freelance Health Editor, September 2023
Next review due September 2026
Inner (or medial) knee pain is exactly that – pain on the inside of your knee. ‘Medial’ means ‘middle’, and the inner side of your knee is the side nearest to the middle of your body. There’s a range of things you can do to manage inner knee pain, and treatments that can help too.
Causes of inner knee pain
Several things can cause inner knee pain. These include:
- an injury such as a blow to the outside of your knee, which pushes your knee inwards
- activities that involve sudden twisting or pivoting of your knees – for example, skiing or playing rugby
- activities where you have to use your knee a lot – for example, cycling, gymnastics or swimming breaststroke
- getting older and your knee joint getting worn down
Conditions that cause inner knee pain
There are several types of knee injury and other conditions that can cause inner knee pain.
Medial collateral ligament injury is a tear of the ligament that runs down the inner side of your knee. A ligament is a band of tissue that connects one bone to another. Your medial collateral ligament connects your thigh bone to your shin bone, and helps to stabilise your knee. A tear can happen if you have a direct blow to your knee, if you twist your knee or if you overuse your knee.
Anterior cruciate ligament injury is a tear to one of the ligaments that runs across the inside your knee and connects your thigh and shin bones. You might completely or partially tear your anterior cruciate ligament. It’s a sudden injury and is caused by either twisting or overextending your knee suddenly. Or it can happen if you suddenly slow down, stop or change direction. It is nearly always associated with sports.
Meniscal injury is a tear to one of the cartilage ‘shock-absorbers’ in your knee. These are known as the menisci (one on its own is called a meniscus). You could tear a meniscus if you twist your knee. This type of injury is common in sports where you have to change direction suddenly – for example, football or basketball. It can also happen if you work in a job that involves heavy lifting and twisting – for example, construction or manual labour. You’re also more likely to tear your meniscus without any particular injury as you get older, through wear and tear.
Osteoarthritis of the knee is a common cause of inner knee pain. In osteoarthritis, structural changes happen to your joints: over time, your cartilage becomes damaged and painful. This condition mostly affects people over 45 and the older you are, the more likely you are to get it.
Patellofemoral pain syndrome (PFPS) means pain at the joint between your kneecap (the patella) and thigh bone (the femur). It might happen if there’s repeated stress on your knee or if your kneecap moves out of alignment. PFPS usually causes pain at the front of your knee, but you can get pain behind or on the inner side of your knee too.
Pes anserinus syndrome (or pes anserine bursitis) is when a small sac of fluid around your knee, known as a bursa, becomes inflamed. It’s common to have this condition alongside other knee problems. But anything that puts additional stress on your knees – for example, obesity and certain sports – may cause it too.
Medial plica syndrome is when a small fold of tissue (a plica) inside your knee becomes inflamed. It causes pain across the inside of your knee and tends to come on when you get active after sitting down for a while.
Inner knee pain symptoms
Pain on the inner side of the knee can feel different for different people. You may feel medial knee pain as a sharp pain or as a mild ache. It can come and go or you may get pain with particular movements such as squatting, going upstairs, or straightening your leg. Other inside knee pain symptoms you may have depend on what’s causing your pain. You may have swelling or, with some types of injury, your knee may click or get stuck in one position (lock).
With a medial collateral ligament injury, you’ll have some pain and stiffness on the inside of your knee. These symptoms usually happen straight away. You may have swelling, but not always.
Pain from an anterior cruciate ligament injury may be sudden and you may hear a ‘pop’. Your knee is likely to swell up quite quickly and may feel as if it’s going to give way.
Symptoms of a meniscus tear generally develop over several hours following the initial injury. You may have pain and swelling and find it difficult to fully straighten your leg. Your knee may also lock or feel unstable, as if it’s about to give way.
Osteoarthritis in your knee usually causes pain when you put weight on your affected leg, and gets better when you rest your leg. You may have stiffness and difficulty moving first thing in the morning or after you sit for a while. You may also have some swelling around your knee.
Patellofemoral pain syndrome causes either a sharp pain or an ache inside your knee, usually at the front of your kneecap, but might also be to the left or right of it. It will feel worse if you run, climb stairs, squat, or if you sit for a long time.
Pes anserine bursitis can cause pain when you go up and down stairs or when you stand up. You may also have pain at night or some slight swelling.
Medial plica syndrome usually causes pain when you go up or down stairs or if you’ve been active for a long time. It can also hurt when you get up from sitting down for a long time. Your knee may also catch or click when you bend or straighten your leg.
When to seek medical help
If your injury is mild, you may be able to manage your symptoms yourself, without seeking medical advice. But see a doctor or physiotherapist if:
- you can’t put weight on the affected leg
- you have severe pain even when you’re not putting weight on it
- your knee gives way, clicks painfully, or locks (gets stuck)
- you can’t move your knee
- your knee is hot, red, or very swollen
Diagnosis of inner knee pain
If you see your GP with knee pain, they’ll examine your knee and will likely ask:
- when your pain started and if there’s anything that makes it worse
- if there’s any activity, accident, or injury that could have caused it
- if you have any other symptoms – for example, your knee giving way or clicking, or pain in any other joints
They may suggest you have an X-ray or an MRI scan, but this isn’t always necessary. Your doctor may be able to make a diagnosis based on your examination and symptoms alone.
If you have cartilage or ligament damage, your doctor may suggest a keyhole surgery procedure to look inside your knee. This is called an arthroscopy and involves making a small cut in your knee and inserting a thin tube and a camera. As well as helping with your diagnosis, damaged tissue can be repaired or removed during the procedure.
Self-help for inner knee pain
There’s a lot you can do to help yourself if you have a knee injury. It’s a good idea to follow the POLICE procedure after an inner knee injury.
POLICE principle
POLICE stands for the following.
- Protect. Protect your injury from further damage. Rest immediately after the injury but not for long. Consider using some form of support or crutches.
- Optimal Loading. Get active sooner rather than later. Start to put weight on your knee and build up your range of movement. Do this gradually – be guided by what feels right for you.
- Ice. Place a cold compress such as a bag of ice or frozen peas wrapped in a towel onto your knee. Do this for around 20 minutes every couple of hours for the first two to three days.
- Compression. Compress your knee using a bandage to help reduce swelling.
- Elevation. Elevate your knee above the level of your heart to reduce swelling. Sit or lie on a chair and use a cushion to raise your leg.
Infographic: POLICE principles
Bupa's POLICE infographic (PDF, 0.5 MB) below illustrates the ‘POLICE principles’ to reduce your pain and help you to recover.

And there are certain things you should avoid in the first three days after your injury so you don’t damage your knee further.
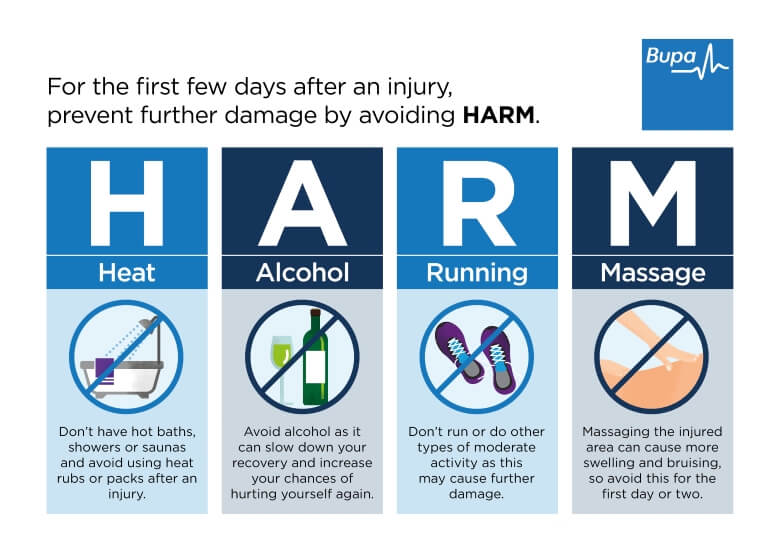
HARM principle
These can be remembered as HARM, which stands for the following.
- H – Heat. Don’t have hot baths, showers or saunas, and avoid heat packs and rubs.
- A – Alcohol. Drinking alcohol can slow down your recovery and mask your symptoms – increasing the risk that you’ll injure yourself again.
- R – Running. Don’t run or do any other form of moderate exercise.
- M – Massage. Massaging the affected areas can cause more swelling and damage, so avoid this for the first day or two.
You can use both POLICE and HARM to treat any type of soft tissue injury to your knee, including an inner knee injury.
Infographic: HARM principle
Bupa's HARM infographic (PDF, 0.6 MB) below illustrates the ‘HARM principle' of things you should avoid doing in the first three days after your injury.
Treatment of inner knee pain
Inner knee pain treatment includes physiotherapy, painkillers and surgery. If you need treatment and what treatment you have, will depend on exactly what’s wrong with your knee. For instance, you may be more likely to need surgery if you have cartilage damage (a meniscus tear) or osteoarthritis that causes severe pain. If you have a ligament injury, physiotherapy may be enough if your knee is stable when you move it.
For information on treatments, please see the relevant knee condition page.
- Medial collateral ligament injury
- Meniscus tear
- Anterior cruciate ligament injury
- Osteoarthritis of the knee
- Patellofemoral pain syndrome (PFPS)
Not quite what you're looking for? Browse all our knee pain pages to find the right treatment advice for your condition.
Looking for physiotherapy?
You can access a range of treatments on a pay as you go basis, including physiotherapy.
To book or to make an enquiry, call us on 0370 218 6528∧
There are lots of different conditions that can cause pain on the inner side of your knee. These include ligament injuries, cartilage damage, and osteoarthritis. These conditions are most often caused by a sports injury, overuse of your knee, or getting older.
For more information, see our sections on causes of inner knee pain and conditions that cause inner knee pain.
The treatment you need for your inner knee pain will depend on exactly what’s causing it. There are many things you can do yourself, including resting your knee and applying an ice pack to it. But for some types of injury, you may need physiotherapy or surgery to repair any damage.
For more information, see our sections on self-help for inner knee pain and treatment for inner knee pain.
Your doctor will assess how serious your knee pain is by asking you questions and examining your knee. If necessary, they’ll arrange for you to have some scans too. Go to see a doctor if your symptoms are severe or don’t start to gradually improve within a few weeks.
For more information, see our section on when to seek medical help.
Bursitis is a condition where the area around a joint or bone is painful, red and swollen due to inflammation. A bursa is a protective thin pocket of jelly-like fluid that sits between your bones and tendons, and acts as a lubricant. Pes anserinus bursitis is one type of bursitis that can cause inner knee pain. Anything that puts additional stress on your knees, such as obesity and certain sports, may cause it.
For more information, see our section on conditions that cause inner knee pain.
Medial collateral ligament (MCL) injury
The MCL is the most commonly injured knee ligament. It often gets injured during sports such as rugby.
Anterior cruciate ligament (ACL) injury
An ACL injury can be a partial or a complete tear, an overstretch, or a detachment of the ligament.
Meniscal tear
Tears of the menisci are a common injury. When people talk about a ‘torn cartilage’ in their knee they usually mean a meniscus injury.
Knee osteoarthritis
Osteoarthritis is a disease that causes pain and stiffness in your joints. Your knee is one of the joints that’s most commonly affected.
Patellofemoral pain syndrome
Patellofemoral pain syndrome is sometimes called ‘runner’s knee’ because it’s particularly common in people who run or do other sports.
Other helpful websites
Discover other helpful health information websites.
Did our Inner (medial) knee pain information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Assessment of knee injury. BMJ Best Practice. bestpractice.bmj.com, last reviewed 16 July 2023
- Knee pain. Versus Arthritis. www.versusarthritis.org, accessed 16 August 2023
- Medial collateral ligament injury. BMJ Best Practice. bestpractice.bmj.com, last reviewed 16 July 2023
- Meniscal tear. BMJ Best Practice. bestpractice.bmj.com, last reviewed 23 April 2023
- Ligament. Encyclopaedia Britannica. www.britannica.com, accessed 17 August 2023
- Anterior cruciate ligament injury. BMJ Best Practice. bestpractice.bmj.com, last reviewed 17 July 2023
- Osteoarthritis. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised October 2022
- Patellofemoral syndrome. Medscape. emedicine.medscape.com, updated 9 January 2023
- Bump JM, Lewis L. Patellofemoral syndrome. StatPearls Publishing. www.ncbi.nlm.nih.gov, last update 13 February 2023
- Patellofemoral pain syndrome. BMJ Best Practice. bestpractice.bmj.com, last reviewed 23 July 2023
- Pes anserine bursitis. Medscape. emedicine.medscape.com, updated 15 June 2023
- Medial synovial plica irritation. Medscape. emedicine.medscape.com, updated 22 July 2022
- Knee sprains and meniscal injuries. MSD Manuals. msdmanuals.com, reviewed/revised July 2023
- Naqvi U, Sherman Al. Medial collateral ligament knee injuries. StatPearls Publishing. www.ncbi.nlm.nih.gov, last update 19 July 2022
- Raj MA. Knee meniscal tears. StatPearls Publishing. www.statpearls.com, updated 18 July 2022
- Osteoarthritis. BMJ Best Practice. bestpractice.bmj.com, last reviewed 16 July 2023
- Osteoarthritis. Versus Arthritis. www.versusarthritis.org, accessed 24 August 2023
- Knee pain – assessment. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised August 2022
- Solheim E, Grøntvedt T, Mølster A, et al. Milestones in the early history of arthroscopy. J Orthop Rep 2022; 1(3). doi: https://doi.org/10.1016/j.jorep.2022.100060
- Meniscal injury. Medscape. emedicine.medscape.com, updated 19 November 2021
- Knee ligament injuries. Patient. patient.info, last edited 10 February 2023
- Bezuglov E, Khaitin V, Shoshorina M, et al. Sport-specific rehabilitation, but not PRP injections, might reduce the re-injury rate of muscle injuries in professional soccer players: A retrospective cohort study. J Funct Morphol Kinesiol 2022; 7(4):72. doi: 10.3390/jfmk7040072
- Bursitis. BMJ Best Practice. bestpractice.bmj.com, last reviewed 25 July 2023



