Knee osteoarthritis
Your health expert: Mr Damian McClelland, Trauma and Orthopaedic Consultant, and Clinical Director for Musculoskeletal Services at Bupa
Content editor review by Rachael Mayfield-Blake, Freelance Health Editor, June 2023
Next review due June 2026
Knee osteoarthritis is a common health condition that causes pain and stiffness in your knee. You can get osteoarthritis in other joints too, but knee osteoarthritis is one of most common types of osteoarthritis.
About knee osteoarthritis
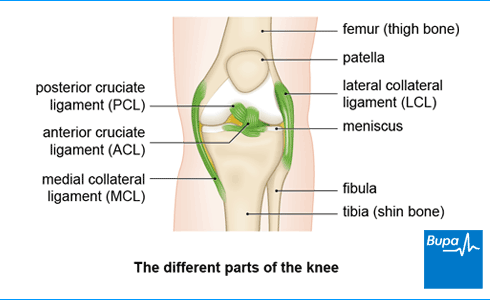
If you have knee osteoarthritis, the different structures that make up your knee joint will have been damaged over time. You lose some of the cartilage that normally allows your bones to move against each other. The shape of your bones can change too, and they may develop bony growths, called osteophytes (bone spurs). The membranes that line your knee joint can also become inflamed. These changes affect how well your knee works and can lead to symptoms such as pain and stiffness.
Osteoarthritis mainly affects people over 50, and you’re more likely to have it the older you are.
Causes of knee osteoarthritis
Doctors don’t know why some people develop osteoarthritis in their knee. But there are some things that can increase your risk. You’re more likely to develop osteoarthritis:
- as you get older
- if you’re a woman
- if you’re very overweight
- if you have worked in a manual job such as farming, or have always exercised – if you’re a runner, for example
There’s also thought to be a genetic risk because knee osteoarthritis can run in families.
Knee osteoarthritis seems to develop after an injury or a series of minor injuries to your knee joint. It may be that the things above combine to make your knee more susceptible to injury or to developing osteoarthritis afterwards.
Symptoms of knee osteoarthritis
Knee osteoarthritis usually affects both of your knees and symptoms include the following.
- You may have knee pain in and around your knee. The pain is worse when you’re active. You won’t usually feel pain in your knee when you’re in bed at night, unless you have severe osteoarthritis.
- Your knee may feel swollen.
- Your knee may be stiff for a while after you’ve been resting or when you first get up in the morning. If you have stiffness in your knee in the morning, it will be for less than 30 minutes after you get up.
- You may find that your knee sometimes gives way. Sometimes it may lock and you can’t straighten it.
- Because of the pain, stiffness and swelling, you might not be able to move your knee as much or as easily as you would usually.
- Your knee may creak or grind when you move it – this is called crepitus.
Diagnosis of knee osteoarthritis
A GP will ask about your symptoms and your medical history and will examine your knee. They’ll usually diagnose knee osteoarthritis from examining you and how you describe your symptoms. But they may refer you to have an X-ray and a blood test to help make the diagnosis and to rule out other things.
Looking for physiotherapy?
You can access a range of treatments on a pay as you go basis, including physiotherapy.
To book or to make an enquiry, call us on 0370 218 6528∧
Self-help for osteoarthritis
There are many things you can do to reduce the pain and stiffness in your knee, and to make living with osteoarthritis a bit easier. Some of the main ones are listed below.
- Try to maintain a healthy weight for your height. This may mean losing weight if you’re overweight. Being overweight puts more stress on your joints and can make osteoarthritis worse.
- Exercise regularly. Exercise can help to strengthen the muscles around your joints and improve your general fitness. Ask a doctor or physiotherapist about the best type of exercise to do.
- Use a walking stick to ease any stress on your knee joint.
- Make sure you wear appropriate shoes – trainers are a good option.
- Use a heat pad or an ice pack to help ease pain. Don’t put either of these directly onto your skin because they may burn – wrap them in a towel or dishcloth first.
Treatment for knee osteoarthritis
There’s no cure for osteoarthritis but there are things you can do to manage the condition and control your symptoms. The main aim of treatment is to reduce your pain and stiffness. This will improve the way your knees function and restore your quality of life.
A GP may refer you to various health professionals, including a physiotherapist. If you have severe pain and stiffness, your GP may refer you to an orthopaedic surgeon (a doctor who specialises in bone surgery).
Devices and physiotherapy
A physiotherapist will assess your knee and plan an individual programme of rehabilitation exercises to help strengthen your knee and leg muscles. It’s important to follow these exercises because they may help to keep your knee working well.
Your physiotherapist may suggest you give a transcutaneous electrical nerve stimulation (TENS) machine a try. It’s a device that sends mild electrical currents through your skin to stop or reduce the pain signals that come from your nerve endings. Some people with osteoarthritis find it useful, although it doesn’t work for everyone. You may be able to borrow a TENS machine from your physiotherapist to try, before you decide to buy one.
A physiotherapist can also assess whether or not knee braces and supports would be useful for you. You can use these as well as other treatments to help keep your knee stable and provide support.
An occupational therapist is a health professional who can give practical assistance to help you manage with everyday tasks. They can advise you on changes you can make to your car, home or workplace to ease any stress on your knee. These may include fitting bath aids, chair and bed raisers, grab rails and extra stair rails.
Medicines
Painkillers can help to ease pain and stiffness, and improve your quality of life. Your doctor may recommend them if you’re still in pain after trying self-help measures. Creams and gels are usually the first painkillers that your doctor will suggest. These contain non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or a painkilling substance called capsaicin. You put these creams and gels directly on your knee.
If these medicines don’t work, your GP may suggest NSAID tablets as well as, or instead of, creams and gels. Your doctor will usually prescribe another medicine to take alongside NSAID tablets to protect your stomach and reduce the risk of side-effects.
If you can’t take NSAID creams, gels or tablets, or they don’t work for you, a GP may suggest you take paracetamol or prescribe weak opioids for you. This will only be for a short time – ask a GP for more information.
Although many people take supplements that contain glucosamine or chondroitin to ease their symptoms, there is limited evidence that these work. Ask your doctor if you’d like more advice about these.
Surgery
If you have osteoarthritis that causes severe pain or has a significant impact on your daily life, your doctor may suggest you have surgery. This will usually only be after you’ve tried the other treatments but they haven’t helped.
There are different knee osteoarthritis operations, which include the following.
- Knee arthroscopy. This isn’t usually recommended for most people with osteoarthritis because it doesn’t tend to have much benefit and there are some side-effects . But your surgeon may suggest you have this keyhole surgery to remove injured parts such as meniscus (cartilage). This is more likely if your knee has been locking.
- An osteotomy. In this procedure, your surgeon will cut and re-align your bone to avoid putting stress on the damaged part of your knee. This may be an option if you’re under 60.
- A partial or total knee replacement. Your surgeon will replace damaged parts of your knee joint with artificial parts.
A GP will refer you to a surgeon to discuss your options. They’ll give you advice on what the best treatment is for you.
Yes, there is treatment for osteoarthritis in the knee. While there’s no cure for osteoarthritis, there are things you can do to manage the condition and control your symptoms. The main aim of treatment is to reduce your pain and stiffness, which will improve the way your knees function and restore your quality of life.
For more information, see our section on treatment for knee osteoarthritis.
The best treatment for osteoarthritis in knees depends on how severe your osteoarthritis is. There are things you can do to reduce the pain and stiffness in your knee, to make living with osteoarthritis easier. Physiotherapy can help strengthen your knee and leg muscles to keep your knee working well. Painkillers can help to ease pain and stiffness, and improve your quality of life. If you have severe osteoarthritis, your doctor may suggest you have surgery.
For more information, see our section on treatment for knee osteoarthritis.
Osteoarthritis in the knee feels painful. The pain will be in and around your knee, and it can be worse when you’re active. Your knee may sometimes give way or lock so that you can’t straighten it. Because of the pain, stiffness and swelling, you might not be able to move your knee as much or as easily as you would usually. It may creak or grind when you move it.
See our symptoms of knee osteoarthritis section for more information.
While knee osteoarthritis can affect everybody differently, it doesn’t always continue to get steadily worse over time in stages. You may find that it reaches a peak a few years after your knee osteoarthritis symptoms start and then stays the same or even gets better. Or you may have several periods of moderate pain with improvements in between. But it’s also possible that it will get progressively worse and you may eventually need surgery.
Did our Knee osteoarthritis information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Osteoarthritis. BMJ Best Practice. bestpractice.bmj.com, last reviewed 11 April 2023
- Osteoarthritis. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised October 2022
- Osteoarthritis: Care and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 19 October 2022
- Musculoskeletal problems. Oxford Handbook of General Practice. Oxford Academic. academic.oup.com, published online June 2020
- Managing osteoarthritis of the knee. Versus Arthritis. www.versusarthritis.org, accessed 22 May 2023
- Electronic pain relief (TENS). Versus Arthritis. www.versusarthritis.org, accessed 22 May 2023
- Osteoarthritis (OA). Managing symptoms. Versus Arthritis. www.versusarthritis.org, accessed 22 May 2023
- Knee replacement surgery. Do I need surgery? Versus Arthritis. www.versusarthritis.org, accessed 22 May 2023
- Osteoarthritis. Medscape. emedicine.medscape.com, updated 30 November 2022



