Anterior cruciate ligament (ACL) reconstruction
- Kathy Francis, Physiotherapist at Bupa
Anterior cruciate ligament (ACL) reconstruction is a type of knee surgery to replace one of the main ligaments in your knee. You may be offered this surgery if you have torn (ruptured) your ACL. It can help to get your knee working properly again.
About ACL reconstruction surgery
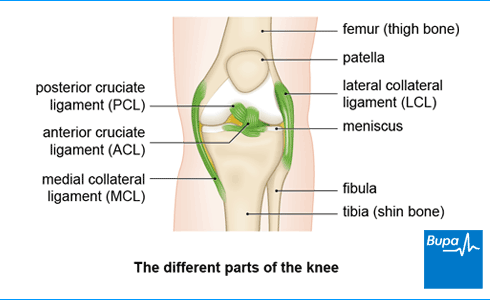
Your anterior cruciate ligament (ACL) connects your thigh bone to your shin bone and helps to keep your knee stable. If you’ve torn or sprained your ACL, ACL reconstruction surgery can replace the damaged ligament with a graft. The graft is a replacement tendon from another part of your knee. It’s usually done as a keyhole procedure. This means your surgeon will perform the operation through tiny holes in your skin, rather than make a larger cut.
Not everyone with an ACL injury needs surgery. But you may need surgery if:
- you play sports that include a lot of twisting and turning – for example, football, rugby or netball – and you want to get back to it
- you have a very physical or manual job – for example, you’re a firefighter or police officer or you work in construction
- other parts of your knee are damaged and could also be repaired with surgery
- your knee gives way a lot (this is known as instability)
It’s important to think about the risks and benefits of surgery and to talk this through with your surgeon. They’ll discuss your treatment options and help you to consider what would work best for you.
Your surgeon will also explain exactly what to expect before, during and after the procedure, and any risks involved. Take your time before you decide, and make sure you ask your surgeon if you have any questions. If you decide to go ahead with the procedure, you’ll need to sign a consent form. This is why it’s important to make sure you fully understand what’s involved.
Preparation for ACL reconstruction surgery
Preoperative rehabilitation (prehabilitation)
Your surgeon is unlikely to do an anterior cruciate ligament (ACL) reconstruction before any swelling has gone down and you’ve got movement back in your knee. This might be within a couple of weeks after your ACL injury, but it varies from person to person. Your surgeon will usually ask you to follow a preoperative rehabilitation programme during this time. This may include:
- exercises designed to strengthen your leg muscles
- exercises to improve your range of motion
- general light activities such as walking and swimming
Getting ready for surgery
Your surgeon will explain what else you need to do to prepare for your operation. For example, if you smoke, they’ll ask you to stop. This is because smoking increases your risk of getting a chest or wound infection, and can slow your healing time.
You’ll usually have ACL reconstruction surgery as a day case, which means you won’t need to stay overnight. You may have it under general or spinal anaesthesia. If you have a general anaesthetic, you’ll be asleep during the operation. If you have a spinal anaesthetic, you’ll stay awake, but the lower part of your body will be numb. Sometimes, you may have a sedative with spinal anaesthesia to help you relax. This may also make you feel drowsy, so you might not remember much about your operation. You’ll need to arrange for someone to drive you home and stay with you overnight.
You’ll usually be given a time to stop eating and drinking before your operation. Follow the advice from your hospital and if you have any questions, just ask.
At the hospital
On the day of your procedure, your surgeon will meet with you to check you’re well and still happy to go ahead. Your healthcare team will do any final checks and get you ready for surgery. They may ask you to wear compression stockings or have an injection to help prevent deep vein thrombosis (DVT).
The ACL reconstruction procedure
Anterior cruciate ligament (ACL) reconstruction usually lasts between one and three hours.
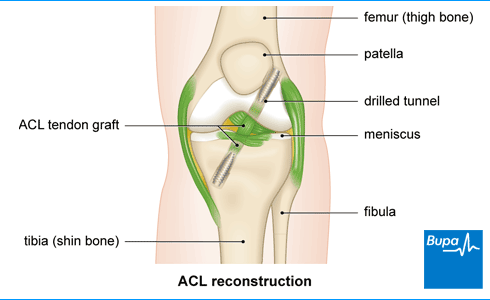
The procedure is usually done by keyhole (arthroscopic) surgery. This means it’s done using instruments that are put through several small cuts into your knee. To see inside your knee, your surgeon will use an arthroscope. This is a thin, flexible tube with a light and camera on the end of it.
After your surgeon has examined the inside of your knee, they’ll remove the piece of tendon to be used as a graft. The graft is usually a piece of tendon from another part of your leg, for example your:
- hamstrings, which are tendons at the back of your thigh
- patellar tendon, which holds your kneecap in place
- quads tendon at the front of your leg
Tissue from a deceased donor can also be used.
Your surgeon will then create a tunnel through the upper part of your shin bone and the lower part of your thigh bone. They’ll thread the graft in through the tunnel and fix it in place, usually with screws or staples. Your surgeon will make sure there’s enough tension on the graft and that you have full range of movement in your knee. Then they’ll close the cuts with dissolvable stitches.
Aftercare following ACL reconstruction surgery
After your operation, you’ll need to rest until the effects of the anaesthetic have passed. You’re likely to have some pain, stiffness and discomfort as the anaesthetic wears off, but you'll be offered pain relief as you need it. Your hospital team will encourage you to get up and move around, and to put weight on your leg as soon as possible. You may need crutches and a knee brace to help support you.
You can usually go home once the anaesthetic has worn off. But you’ll need someone to drive you home and stay with you overnight. You’ll have dressings over the wounds around your knee.
Before you go home, your nurses will give you advice about caring for your healing wounds. They’ll also talk to you about any possible complications to look out for – for example, signs of infection. For more information on these, see our section on complications. They’ll also discuss pain relief you can take at home. They may give you a date for a follow-up appointment, including any physiotherapy sessions you’ll need.
A general anaesthetic can make you feel very tired. You might find that you’re not so co-ordinated or that it’s difficult to think clearly. This should pass within 24 hours. In the meantime, don’t drive, drink alcohol, operate machinery or make any important decisions.
Recovery from ACL reconstruction surgery
It usually takes about six months to a year to make a full recovery from anterior cruciate ligament (ACL) reconstruction.
You’ll see a physiotherapist within the first few days after your operation. They’ll give you a rehabilitation programme with exercises specific to you. This will help you to get the full strength and range of motion back in your knee. You’ll usually have a series of goals to work towards. This will be very individual to you, but a typical ACL reconstruction recovery timeline may be similar to this:
- 0 to 2 weeks – building up the amount of weight you can bear on your leg and its range of motion
- 2 to 6 weeks – by this time you can begin to walk normally without pain relief or crutches
- 6 to 14 weeks – your full range of motion should be restored, and you’ll be able to climb up and down stairs
- 3 to 5 months – you’ll be able to do activities such as running without pain (but you’ll need to still avoid some sports that your surgeon will tell you about)
- 6 to 12 months – by this time you can return to non-contact sport – for example, tennis or badminton
- 12 months – you can return to contact sports such as netball, rugby or football
The exact ACL reconstruction surgery recovery time varies from person to person and depends on many things. These include the sport you play, how severe your ACL injury was, the graft used and how well you’re recovering. Your physiotherapist will ask you to complete a series of tests to see if you’re ready to get back to sport. They’ll want to check that you feel mentally ready to return too.
During your recovery, you can continue to take over-the-counter-painkillers such as ibuprofen. It’s important to read the patient information that comes with your medicine and if you have any questions, speak to your pharmacist for advice. You can also put ice packs (or frozen peas wrapped in a towel) on your knee to help reduce pain and swelling. Don’t put ice directly on your skin because ice can damage your skin.
Your surgeon will advise you when you can return to work, drive, and do other activities.
Complications of ACL reconstruction surgery
Most people recover well from anterior cruciate ligament (ACL) reconstruction, but any surgery carries a risk of complications. The main complications of ACL reconstruction surgery are listed here.
- Your knee might keep on giving way (instability). This may happen if there’s a problem with the placement of your graft. The graft is at its weakest around 6 to 12 weeks after surgery. It’s important to follow your physiotherapist’s advice about how to progress with exercises during this stage.
- Your knee might continue to feel stiff, and it might not move as well as it did before. This may be caused by arthritis or arthrofibrosis (when scar tissue forms in your knee joint).
- You may continue to feel pain in your knee. The pain will often settle within the first couple of weeks but sometimes it can continue for a little longer – it’s not known why.
- A break (fracture) in your kneecap.
- You may get a tear in your graft and need further surgery.
- Your knee graft wound could get infected. This can be treated with antibiotics.
- You might get a blood clot in your leg (deep vein thrombisis) .
Your risk of complications may be higher if you have other problems with your knee. These include an injury to the meniscus (cartilage) in your knee.
Alternatives to ACL reconstruction surgery
The alternative to having anterior cruciate ligament (ACL) reconstruction surgery is to continue with physiotherapy. Your physiotherapist will give you exercises to work on your strength and control of your injured knee to help you recover to achieve your goals. It may take some months to get back to activity. You may find that physiotherapy is enough, especially if you’re not planning to do high-level sports or activities. Your doctor or physio might suggest you wear a knee brace to give your knee some extra support during weight-bearing exercises such as skiing or tennis.
You can also decide to delay surgery and see how you get on with physiotherapy first.
Looking for physiotherapy?
You can access a range of treatments on a pay as you go basis, including physiotherapy.
To book or to make an enquiry, call us on 0370 218 6528∧
If you have an anterior cruciate ligament (ACL) injury, your knee is likely to be very swollen and painful. You may hear or feel a pop when the injury happens, and you may feel as if your knee might give way. You won’t be able to move your knee as much as usual and may find it difficult to stand and walk. Seek urgent medical advice if you have these symptoms.
Yes, you’ll be encouraged to put weight on your leg and to move around as soon as possible. You may need crutches to support you at first. But you should be able to walk normally after a couple of weeks (unless you have meniscal repair surgery at the same time as your ACL reconstruction).
For more information, see our sections on aftercare following ACL reconstruction surgery and recovery from ACL reconstruction surgery.
ACL reconstruction can be considered major surgery because you may have the procedure under general anaesthesia, but you may have spinal anaesthesia instead. While most people recover well from ACL reconstruction, there are some risks. Complications of ACL reconstruction surgery include your knee continuing to give way (instability), which may happen if there’s a problem with the placement of your graft. And you may continue to feel pain in your knee.
For more information, see our section on complications of ACL reconstruction surgery.
The recovery time for ACL reconstruction is usually about six months to a year for a full recovery. A physiotherapist will give you a rehabilitation programme with exercises to help you to get the full strength and range of motion back in your knee. You’ll usually have a series of goals to work towards, and this will be very individual to you.
For more information, see our section on recovery from ACL reconstruction surgery.
Did our Anterior cruciate ligament (ACL) reconstruction information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Evans J, Mabrouk A, Nielson JI. Anterior cruciate ligament knee injuries. StatPearls Publishing. www.ncbi.nlm.nih.gov, last updated 19 February 2021
- Knee ligament injuries. Patient. patient.info, last edited 16 February 2022
- Types of surgery. Royal College of Surgeons of England. rcseng.ac.uk, accessed 3 June 2024
- Anterior cruciate ligament injury. BMJ Best Practice. bestpractice.bmj.com, last reviewed 30 April 2024
- Aryana IGNW, Febyan F, Dimitri D, et al. Functional outcome of ACL reconstruction following pre-reconstruction rehabilitation vs. none rehabilitation: A systematic review and meta-analysis. Rev Bras Ortop (Sao Paulo) 2024; 59(2):e172–e79. doi: 10.1055/s-0044-1779327
- Anterior cruciate ligament injury. Medscape. emedicine.medscape.com, updated 26 February 2021
- Preparing for surgery – fitter better sooner. Royal College of Anaesthetists. www.rcoa.ac.uk, accessed 23 May 2024
- Smoking and surgery. Action on Smoking and Health. ash.org.uk, published April 2023
- You and your anaesthetic. Royal College of Anaesthetists. www.rcoa.ac.uk, reviewed April 2023
- Important complications of anaesthesia. Patient. patient.info, last updated 14 February 2024
- General anaesthesia. Patient. patient.info, last updated 15 August 2023
- Caring for someone recovering from a general anaesthetic or sedation. Royal College of Anaesthetists. www.rcoa.ac.uk, reviewed November 2021
- Orthopaedics. Oxford Handbook of Operative Surgery. Oxford Academic. academic.oup.com, published online June 2017
- Anaesthesia explained. Royal College of Anaesthetists. www.rcoa.ac.uk, published 1 March 2021
- Adhitya IPGS, Kurniawati I, Sawa R, et al. The risk factors and preventive strategies of poor knee functions and osteoarthritis after anterior cruciate ligament reconstruction: A narrative review. Phys Ther Res 2023; 26(3):78–88. doi: 10.1298/ptr.R0028
- Rachael Mayfield-Blake, Freelance Health Editor



