Osteoarthritis
Your health expert: Sundeept Bhalara, Consultant Rheumatologist and General Physician
Content editor review by Pippa Coulter, Freelance Health Editor, September 2023.
Next review due September 2026.
Osteoarthritis is a condition that causes painful, stiff joints, including hips and knees. It means your joint may not work as well. It’s the most common form of arthritis in the UK. It usually affects people from the age of 45 onwards.
About osteoarthritis
Osteoarthritis most commonly affects your knees, hips, and the small joints in your hands. It can affect other areas too, including your lower back, neck, and big toes.
It’s thought that around 1 in 10 adults in the UK have osteoarthritis of the hip, and nearly a quarter have knee osteoarthritis. You’re more likely to develop it as you get older. It’s uncommon in people under the age of 45.
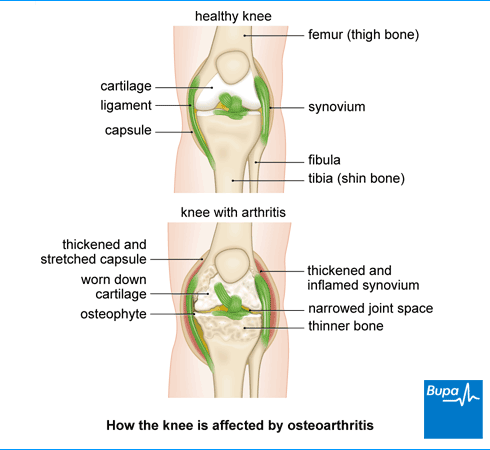
The condition is thought to develop following damage to your joints. This can happen gradually, if your joint becomes worn down through repeated stress over time. Or it can happen as a result of an injury or another condition. This leads to permanent changes inside your joint. These changes can cause pain and stiffness.
Osteoarthritis can affect different people in different ways. It can also affect one joint differently to another in the same person. It’s possible your symptoms may get worse over time, but this isn’t always the case. They may stay the same or even improve with time.
Causes of osteoarthritis
It’s not clear exactly what makes someone develop osteoarthritis. It’s thought to be down to a combination of several different things. The following factors are known to increase your risk of developing the condition.
- Being over 45. Your risk increases as you get older.
- Being female. Osteoarthritis can affect anyone, but you’re at greater risk if you’re female.
- Being obese. The extra weight puts more strain on your joints, especially your knees.
- Having a family history of osteoarthritis.
- Doing lots of activity that involves putting stress on your joints. Examples include manual work and sports such as running or football.
- Injuring your joint.
- Having other problems affecting your joints or muscles. These may mean you put more stress on your joints than usual.
Symptoms of osteoarthritis
Osteoarthritis symptoms include the following.
- Joint pain that’s worse when you’ve been active and tends to feel better when you rest. If your arthritis is severe, you may be in pain at night or when you’re resting too.
- Stiffness first thing in the morning or after resting. Not everyone gets this, but if you do, it usually wears off quickly (within 30 minutes).
- Not being able to use your joint or move it as much as before.
- Swelling around the affected joint.
- A crunching or grinding feeling or noise (crepitus) when you move the affected joint.
The pain and stiffness in your joint can make certain activities difficult. This depends on the joint affected. For example, if you have osteoarthritis in your fingers or hands, you may find it difficult to grip or pinch things. You may find things like opening jars, fastening buttons or writing difficult. If you have osteoarthritis in a hip or knee, it can make it difficult to walk, climb stairs or drive.
Sometimes you may feel pain in a different area of your body to the joint that’s affected. For instance, if you have osteoarthritis in your hip, you might feel pain in your groin, thigh, knee or ankle.
If you’re getting painful or stiff joints, contact your GP for advice.
Diagnosis of osteoarthritis
A GP will usually be able to diagnose osteoarthritis by examining you and asking about your symptoms. They’ll want to know where and when you feel any pain, how bad it is, and how long it’s been going on. They will also ask you about any risk factors you may have for osteoarthritis, including your medical and family history.
Your GP will examine your joint. This usually involves looking at and feeling your joint to check for any swelling or tenderness. They’ll want to see how well you can move your joint. If your knee or hip is affected, they might look at how well you’re walking or standing. They’ll also want to weigh you and take your height to work out your body mass index (BMI).
You won’t usually need X-rays or other tests to diagnose osteoarthritis. But your GP may sometimes recommend an X-ray to confirm a diagnosis or rule out other conditions.
Management of osteoarthritis
There isn’t a cure for osteoarthritis. But there’s lots of things you can do to relieve your pain and manage your symptoms. The main treatments for osteoarthritis include the following.
- Exercise
- Weight management
- Pain medicines
- Aids and devices to help in daily activities
- Surgery
Your GP will discuss which of these options may be relevant to you. We have more on each one below.
Exercise for osteoarthritis
Exercise is one of the most beneficial things you can do if you have osteoarthritis. Exercise can help to keep your joints working well and reduce your pain. It will also help to build up your muscle strength and improve your fitness. Keeping active can help to boost your mood too.
Sometimes, your GP may recommend a structured exercise programme you can join. Or they might give you some advice about what to try. You might want to consider seeing a physiotherapist, who can help to create an individual exercise programme that works for you.
Aim to do a variety of different types of exercise, including the following.
- Strengthening exercises, to help strengthen the muscles that support your joints. You can use light weights or a resistance band for strengthening exercises. You can also just use your own body weight.
- Aerobic exercises, to increase your heart rate and make you breathe faster. This is good for overall health and fitness, and to help lose or maintain your weight. You might find it best to do a low-impact aerobic exercise that doesn’t put too much strain on your joints. Examples include swimming, cycling or walking.
- Flexibility/stretching exercises, to help improve the range of movement of your joints.
Try to find something that you can stick with and enjoy. It’s important to build up the amount of exercise you do gradually. It might feel painful when you first start exercising. Try taking a painkiller such as paracetamol beforehand. You can also use a heat pad or an ice pack to help relieve pain. Don’t put either of these directly on to your skin as they may damage it or even give you a burn. Wrap them in a towel first.
Weight loss and diet
If you’re overweight or obese, losing excess weight can make a big difference to your symptoms. Losing even a little weight can help. Use our BMI calculator to see if you’re a healthy weight.
The best way to lose weight is to make changes to your diet. Make sure you’re following a healthy, balanced diet , and limit foods high in saturated fat or sugar. Being more active will also help with weight loss.
It’s been suggested that making the following dietary changes may also be helpful for osteoarthritis.
- Eating at least one portion of oily fish a week, or taking fish oil capsules. Oily fish include sardines, mackerel and salmon. They contain omega-3 fatty acids, which are known to have anti-inflammatory properties. Scientists are looking at whether this may help in osteoarthritis.
- Reducing high cholesterol. There’s some evidence of a link between blood cholesterol and development of osteoarthritis. It’s been suggested that reducing your cholesterol if it’s high could help with osteoarthritis.
- Getting enough vitamin K. Vitamin K is important for healthy bones and cartilage. It’s possible this could help with osteoarthritis. Good sources of vitamin K include green, leafy veg, chicken and eggs.
More evidence is needed to say for certain how helpful these measures are for osteoarthritis. But they’re all important for your health in other ways, so it makes sense to follow them if you can.
Medicines
Medicines won’t cure osteoarthritis, but they may help to ease your pain and any stiffness. You should take any medicines for as short a time as possible, and to help you keep active. Your doctor may suggest trying some of the following.
- Creams or gels containing a non-steroidal anti-inflammatory drug (NSAID). You rub these directly onto your joint. You can also get creams or gels containing a substance called capsaicin.
- NSAID tablets. These include standard NSAIDs, like ibuprofen or naproxen, and newer types like celecoxib or etoricoxib. Your GP may suggest these if creams or gels haven’t helped. You might need to take proton-pump inhibitors alongside these medicines to help protect your stomach.
- Paracetamol. This isn’t usually recommended as it doesn’t seem to work very well for osteoarthritis. But your doctor may suggest it on occasion for short-term pain relief. You should usually only take it if you can’t take any other medicines for pain relief, or they haven’t worked for you.
- Codeine. This is one of the weaker opioids – a group of strong painkilling medicines. Like paracetamol, you should only use it occasionally, and for short periods of time.
Always read the patient information leaflet that comes with your medicine. If you have any questions, ask your pharmacist for advice.
Your GP may suggest having a steroid injection into your joint. These can help to provide short-term pain relief, for up to about 10 weeks. They may suggest this if other painkillers aren’t working or aren’t suitable for you. Your GP may refer you to a musculoskeletal clinic to have the injection.
You may also be offered treatment with hyaluronic acid injections. There’s some research suggesting that these injections can improve osteoarthritis symptoms. But evidence about how well they work is quite mixed, so they’re not recommended for use on the NHS.
Aids and devices
There are various aids and devices that can make everyday life easier for you if you have osteoarthritis. Your GP may refer you to other health professionals to get more help and advice with this. These may include the following.
- Braces, splints and joint supports to protect your joint. These can help to reduce stress on your joints, or help with joint instability. A physiotherapist or occupational therapist can help with this.
- Adaptations you can make in your home, such as installing stair rails or grab rails in your bathroom. Raised toilet seats and a bath board/seat may also be helpful. An occupational therapist can advise you about what’s available.
- Walking sticks or other aids to help you walk and reduce pressure on affected joints. This is also something an occupational therapist can help with.
- Gadgets and aids that can help with osteoarthritis in your hand. Examples include tap turners, kitchen utensils with padded handles and automatic can-openers.
- Insoles and other devices to use with footwear. You can see a podiatrist (a specialist in foot care) to help with this. They can also give you advice on the best footwear to use.
You may be eligible for some help towards the cost of any aids or adaptations you need in your home. Contact your local authority for a free assessment.
If you’re in work, ask if your employer has an occupational health department. They’ll be able to look at how you can make changes to how you work, or your working environment to make things easier.
Surgery
If your pain is significantly impacting your quality of life, and other treatments aren’t helping, your GP may refer you to an orthopaedic surgeon. The surgeon will talk to you about whether surgery on your joint may be an option for you. Surgery may involve replacing all or part of your joint with an artificial one (a hip replacement or knee replacement ). Another type of surgery involves joining (‘fusing’) bones in your joint together. You may have this for osteoarthritis in your foot or hand. Your surgeon will explain what surgery will involve.
Complementary therapies
Many people with osteoarthritis try complementary therapies to ease their symptoms. These include acupuncture, massage and dietary supplements, such as glucosamine and chondroitin.
There’s not always a lot of evidence to support these therapies. But some people do find a benefit from using them. Therapies like aromatherapy and massage may also help you to relax. If you decide to give them a try, be aware of possible side-effects and risks. They shouldn’t replace any treatment your doctor recommends. If you’re planning to try a supplement or herbal medicine, speak to your pharmacist first. It’s possible they might affect other medicines you’re taking.
Physiotherapy services
Our evidence-based physiotherapy services are designed to address a wide range of musculoskeletal conditions, promote recovery, and enhance overall quality of life. Our physiotherapists are specialised in treating orthopaedic, rheumatological, musculoskeletal conditions and sports-related injury by using tools including education and advice, pain management strategies, exercise therapy and manual therapy techniques.
To book or to make an enquiry, call us on 0345 850 8399
The most important link between diet and arthritis is the effect it has on your weight. Being overweight or obese can increase the stress on your joints, making symptoms worse. It’s important to follow a healthy, balanced diet so you can keep to a healthy weight. It’s possible that certain foods, such as oily fish, may be helpful for osteoarthritis. Read more in our management of osteoarthritis section.
If you’re overweight, this will put a strain on your joints, particularly your knees, hips, and lower back. If you’re overweight or obese, losing even just a little weight may significantly help to reduce pain and stiffness in your joints. The best way to lose weight is to make changes to your diet. Increasing your activity will also help. See our management of osteoarthritis section for more information.
The main symptom of osteoarthritis is pain in your joint. The pain tends to be worse when you’ve been active and better when you rest. You may also get stiffness in your joint, and not be able to move it as much. Sometimes you may also notice a crunching or grinding in your joint. See our symptoms of osteoarthritis section for more information.
Knee osteoarthritis
Osteoarthritis is a disease that causes pain and stiffness in your joints. Your knee is one of the joints that’s most commonly affected.
Knee replacement
Hip replacement surgery and hip revision
Hip replacement surgery is a procedure to replace your hip joint with artificial parts (prosthesis) if it’s been damaged or worn away.
How to start exercising
We should all be getting active – and it may be easier than you think. Here we give you tips and advice for getting started
Did our Osteoarthritis information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Osteoarthritis. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised October 2022
- Osteoarthritis. Patient. patient.info, last updated 21 November 2022
- Osteoarthritis (OA). Versus Arthritis. www.versusarthritis.org, accessed 6 September 2023
- Osteoarthritis. BMJ Best Practice. bestpractice.bmj.com, last reviewed 6 August 2023
- The state of musculoskeletal health 2023. Versus Arthritis. www.versusarthritis.org, accessed 6 September 2023
- Osteoarthritis in over 16s: diagnosis and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 19 October 2022
- Hurley M, Dickson K, Hallett R, et al. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: a mixed methods review. Cochrane Database of Systematic Reviews 2018, Issue 4. Art. No.: CD010842. DOI: 10.1002/14651858.CD010842.pub2
- Fransen M, McConnell S, Harmer AR, et al. Exercise for osteoarthritis of the knee. Cochrane Database of Systematic Reviews 2015, Issue 1. Art. No.: CD004376. DOI: 10.1002/14651858.CD004376.pub3
- What types of exercise should I do? Versus Arthritis. www.versusarthritis.org, accessed 7 September 2023
- Lu B, Driban JB, Xu C, et al. Dietary fat intake and radiographic progression of knee osteoarthritis: data from the osteoarthritis initiative. Arthritis Care Res (Hoboken) 2017; 69(3):368–75. doi: 10.1002/acr.22952
- Osteoarthritis and diet: food fact sheet. BDA – The Association of UK Dietitians. www.bda.uk.com, published October 2021
- Thomas S, Browne H, Mobasheri A, et al. What is the evidence for a role for diet and nutrition in osteoarthritis? Rheumatology (Oxford) 2018; 57(suppl_4):iv61-iv74. doi: 10.1093/rheumatology/key011
- Hyaluronan injections. Versus Arthritis. www.versusarthritis.org, accessed 7 September 2023



