Diuretics
- Dr Joshua T Y Chai, Consultant Cardiologist
Diuretics are medicines that increase the amount of urine you produce. This allows your body to get rid of excess water and salts. Diuretics are often called water tablets.
Uses of diuretics
Your doctor may prescribe diuretics for you if you have:
- high blood pressure – diuretics are one of several types of medicine your doctor may prescribe
- too much fluid in your body tissues (known as oedema) as a result of heart failure
Diuretics are sometimes used for other conditions too. For the eye condition glaucoma, you may have diuretic eye drops to help lower the pressure in your eye.
Diuretics aren’t suitable for everyone. They might cause problems if you have certain other medical conditions. And they can interact with other medicines you may be taking. For more information, see our sections on side-effects of diuretics and interactions of diuretics. Always tell your doctor about any other conditions you have and any medicines you’re taking.
Make sure your doctor knows if you are or may be pregnant. Some diuretics can harm your unborn baby. If you’re breastfeeding, ask your doctor about which diuretic is safe for your baby.
How do diuretics work?
Your kidneys filter out water, salts, and waste products from your blood. Most of the water and salts are then taken back into your bloodstream. But some are passed out of the body in your urine (pee).
Diuretics stop the kidneys from taking salts and water back into your bloodstream. So you get rid of more water and salts in your pee. That means you’ll need to pee more often, which is why they’re often called water tablets.
Getting rid of extra salts and fluid in this way lowers the volume of blood in your bloodstream. This helps to lower your blood pressure and gives your heart less work to do.
Types of diuretic
There are different types of diuretic with different uses. The most common ones are listed below.
- Thiazide and thiazide-related diuretics. These are mainly used at low doses to treat high blood pressure. You may have them to treat heart failure. An example is metolazone.
- Loop diuretics, which are used in heart failure or chronic kidney disease. You may have them to treat a build-up of fluid or, along with other medicines, to treat high blood pressure. An example is furosemide.
- Potassium-sparing diuretics. These are usually used with other diuretics. They help get rid of fluid but stop you losing too much potassium at the same time. An example is spironolactone.
Over-the-counter or natural diuretics
Diuretic medicines must be prescribed by your doctor. But you may have heard of diuretics you can buy over the counter. These are sometimes called natural diuretics. These herbs or dietary supplements claim to have a mild diuretic effect. Some people use them for water retention linked to their periods. But there’s no evidence to show that they work.
If you think you may have water retention, talk to your GP rather than trying to treat it yourself. Some serious medical conditions can make your body hold on to too much water. Herbal remedies and supplements can cause problems with other medicines you’re taking. So it’s always best to check. Your pharmacist can give you advice.
Taking diuretics
Most diuretics are tablets that you swallow. But if you need treatment quickly, you may have a diuretic as an injection into a vein in your arm.
Diuretics make you need to pee more often and usually start to act within one to two hours of taking them. It’s worth thinking about when you take them, so that they cause the least disruption to your day. Taking them early in the day might mean that they’re less likely to cause problems with your sleep. Talk to your doctor to work out what suits you best. If you have a long journey to make, you may need to think about planning some breaks.
If you forget to take your usual dose of diuretic, take it as soon as you remember. If it’s nearly time for your next dose though, just take that one as normal – don’t take double. If you accidentally take too much, contact your doctor or pharmacist for advice.
Some diuretics can cause you to lose too much potassium. So alongside your usual diuretic, your GP may prescribe either:
- a potassium-sparing diuretic (for more information, see our section on types of diuretic)
- a potassium supplement
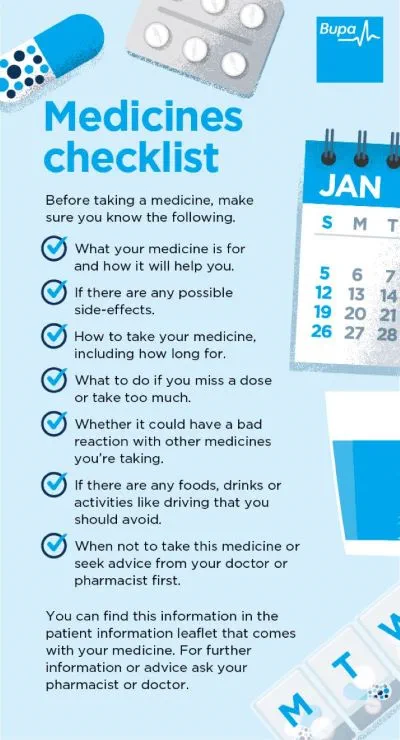
Always read the patient information leaflet that comes with your medicine. If you need advice about taking your medicines, ask your pharmacist.
GP Subscriptions – Access a GP whenever you need one for less than £20 per month
You can’t predict when you might want to see a GP, but you can be ready for when you do. Our GP subscriptions are available to anyone over 18 and give you peace of mind, with 15-minute appointments when it suits you at no extra cost.
Interactions of diuretics
Medicines
Diuretics can sometimes interact with certain other medicines. This can affect how well your medicines work or make side-effects more likely.
There will be a patient information leaflet that comes with your diuretic. This includes a list of medicines that might interact with it. It’s important to read this list. Diuretics may interact with other medicines you may be taking for high blood pressure or heart failure. Over the counter painkillers such as ibuprofen can also affect diuretics.
Your pharmacist or doctor will be able to tell you if any medicines you take may be affected. Make sure your doctor knows what you’re already taking when they prescribe you medicines. Your doctor may adjust your dose or suggest an alternative if needed. Don’t stop any medicine without talking to your doctor first.
Food and drink
Too much salt in your diet can counteract the effects of some diuretics. So you might have to reduce the amount of salt you eat. Always follow your doctor’s advice and read the information that comes with your medicine. Ask your doctor if you’re not sure how much salt you can eat.
If you’re taking potassium-sparing diuretics, you should avoid salt substitutes. Most of these are high in potassium, so they could make the potassium level in your blood too high. Try using herbs and spices to add flavour to your food instead.
Be careful when drinking alcohol while taking diuretics. Alcohol and diuretics together may make your blood pressure fall too low.
Vitamin and mineral supplements
Don’t take potassium supplements at the same time as potassium-sparing diuretics. Taking the two medicines together could make your potassium level dangerously high.
You may also need to be careful if you take calcium supplements. Taken with some diuretics, these can make the level of calcium in your body too high. Make sure your doctor knows if you’re taking any supplements when they’re prescribing medicines. Always read the patient information leaflet that comes with your medicine.
Side-effects of diuretics
Side-effects are unwanted effects that you may get from taking a medicine. There are many different diuretics, and each can have different side-effects. The best way to find out about any side-effects is to read the patient information leaflet that comes with your medicine. Alternatively, you can ask your pharmacist.
Common side-effects of diuretics include:
- dizziness
- feeling very tired
- headache
- feeling sick
- low blood pressure, especially when standing up
- losing too much potassium or sodium, which can cause muscle weakness and cramps
Diuretics can sometimes affect other medical conditions you may have. If you have gout, some diuretics can make your symptoms worse. If you have diabetes , they can make your blood sugar level higher.
Taking diuretics can also make you dehydrated, which means you don’t have enough water in your body. Your doctor can advise you about how much fluid to drink.
Contact your doctor if you feel thirsty, lightheaded or dizzy while on diuretics. These may be signs of dehydration. If you have diarrhoea and vomiting, you may need to stop taking your diuretic for one to two days. This will help to stop you becoming dehydrated. If your symptoms go on for more than two days, contact your GP.
In very hot weather or if you travel to a hot country, you’re more at risk of dehydration. Monitor the colour of your pee to give you an idea of how hydrated you are. But if you’re on high doses of diuretics, you may also need to talk to your GP.
If you’re having mild side-effects, wait a few days to see if they ease. If they continue or you’re feeling unwell or concerned, contact your doctor or pharmacist.
Check-ups
Once you’ve started taking a diuretic, you’ll have regular health checks. These will monitor your blood pressure and kidney function along with your salt and potassium levels. Checks may be fairly frequent to begin with. How often will depend on which diuretic you’re taking. Eventually, you’ll need these checks less often – around every six months to a year. Your doctor will also check your kidney function if your dose changes.
Medicines checklist
Our handy medicines checklist helps you see what to check for before taking a medicine. Bupa's medicines checklist PDF opens in a new window (0.8MB)
Diuretics are medicines that increase the amount of urine (pee) you produce. They get rid of excess water and salts and are often called water tablets. Your doctor may prescribe diuretics if you have high blood pressure or heart failure.
For more information, see our sections on uses of diuretics and how diuretics work.
There are several types of diuretic. Depending on why you need them, your doctor may suggest:
- thiazide and thiazide-related diuretics (for example, spironolactone)
- loop diuretics (for example, furosemide)
- potassium-sparing diuretics (for example, amiloride)
For more information, see our section on types of diuretic.
High blood pressure (hypertension)
Low blood pressure (hypotension)
Keeping hydrated
We explain why you need to drink enough and offer some tips to help you stay hydrated
Did our Diuretics information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Liz Woolf, Freelance Health Editor



