Employee resources for muscle, bone and joint health
Resources for your team
It's important to give your team the right support when they need it. That's where our resources can help.

Do emotions affect back pain?
Sometimes back pain can last a long time and affect your daily working life. In this article, we explore how staying active and having a positive outlook can help manage your back pain.

Common running injuries and prevention
Although it can have many benefits, running also comes with the risk of injury if not done correctly. In this article we explore some common running injuries and ways you can prevent them happening.

Stretches to ease aches and pains
We might spend many hours sat at a desk, driving, or using devices that strain our upper body. In this article, we show some simple stretches you can do to help ease these aches and pains.

How to look after your back
Back pain and discomfort can affect everything from sleep to your activity levels, so it's important to try and prevent any issues developing. Learn more in our helpful article.
Got a question about muscles, bones and joints? Just ask
Hear from Mike Livesey, specialist MSK physiotherapist and clinical lead at Bupa.
Transcript
Who are you?
Hi, I'm Mike Livesey.
I'm a specialist MSK physiotherapist
and clinical lead at Bupa.
Come and ask me a question about MSK conditions
and injuries
What does MSK stand for and what are some examples of conditions?
So MSK stands for musculoskeletal, so
that's anything to do with our body.
So we're looking at the joints in our body,
the muscles in our body, and anything that acts on it.
So it's looking at your function and how that's adapted.
So classically in clinic, we'll see lots
of problems coming in with back pain, neck pain, shoulder
and knees, and they're our top four.
The main sort of breakdown of injuries we tend
to see is more acute injuries,
so they may be traumatic sprains and strains,
or more chronic persistent issues like arthritis.
What's the difference between a ligament and tendon?
A ligament is a structure that fastens bone to bone.
So we'll see these around joints
to help stabilise the joint.
These are inert structures so they don't move.
They're set at a limit
and they have a limit at what they can work to.
So what I mean by that is if you stretch the ligament more
than it can tolerate, it'll break down and cause an injury.
So for example, we'll see that regularly with ankle sprains.
If you roll your ankle off a curb,
the ligament will be overloaded
and it will go beyond what it can tolerate and it will tear
and you'll start to get pain, injury and loss of function.
Now, tendons are structures that fasten muscles
to bone, and these are more contractile structures,
so they're more active structures with the muscle.
They act upon the joint
and allow the joint to move for you to be functional
or do the desired exercise that you want to do.
These injuries
or the injuries with tendons we see tend to be more
with overload injuries.
When you do too much too soon
and the body can't cope with it and it breaks down.
What's the difference between a fracture and break?
So we do get asked this a lot between fractures
and breaks, and there is no difference.
They're exactly the same.
It's just a mix in terminology
and clinically, we'll use fractures as the word,
and these can be categorised into a
few different subcategories.
So the least bony injury we see is a stress fracture,
and that might be caused from more repetitive strains.
Maybe with running a more impact exercise,
you'll also get an undisplaced fracture.
These maybe could be known as a green stick fracture
or a hairline fracture, worsening fractures.
You can get a displaced fracture
where the bone actually has moved out of position
and may need realigning surgically,
and we get even worse from that is a communed fracture
where we find that the bone breaks into several pieces
and very often that does need surgical repair in order
to reduce the bone back into position for the body to heal
and repair.
What's the difference between a tear and rupture?
So tears can be really, really simply in sort
of three categories.
So a grade one tear is
where we tear a small number of fibres.
So that's normally about less than 10%
of fibres in the structure that are damaged and torn.
So functionally, this doesn't have loads of impact on us.
It can cause pain. It'll cause maybe some mild swelling,
but it's rare that it impacts your function
apart from causing pain.
These are injuries that tend to resolve quickly with rest
with activity modification.
And it's rare that you need
to see a professional for support with this.
A grade two strain
or tear, it's something that
causes more disruption to the tissue.
And we'll see that between anywhere between 10%
and 90% of our tissue is damaged.
So that can cause, as you can imagine,
significant amounts of functional change.
And with that, we see swelling, we'll see bruising,
we'll see inability to move
or even inability to load that structure
because of the pain.
And as you can imagine, with more tissue damage, it's going
to take longer for those tissues to heal.
They should still heal because there are structures
or the part of the structure is still attached.
However, you may find that it takes a little bit longer.
You may need a little bit of professional support
through a physiotherapist to aid your recovery
so you can get back to your function or your sport.
And then finally, we can have a complete rupture,
which would be a grade three tear,
and that's where the structure is completely parted
and we're left with two parts of the structure.
Classically, if that's caused with a trauma, we'll go
and see an orthopaedic surgeon to get advice
and support on that as to see whether they feel
that they should repair that surgically
or whether it could be managed conservatively
with physiotherapy.
Why is my desk setup at work important?
Desk setups are really important
because we can spend between 30 and 50% of our day working.
And so if your work is inactive
and you are desk-based, it's a lot
of time potentially in a sitting position.
What we need to look at is we need
to look at the equipment that we've got around us.
You should be sitting comfortably
with our feet flat on the floor.
Our knees should be around 90 degrees,
maybe a little bit less,
and our hips slightly higher than our knees. When we're
sitting, sit in a supportive chair to make sure
that you've got the ability to rest your back
and sit back at the back of the chair.
And what we want is we want your elbows
to be relaxed comfortably by your sides,
your shoulders relaxed,
and your forearms being able
to rest comfortably on the desk in front of you.
Try and avoid reaching out in front of you to your keyboard
and make sure your screen height is looking at about eye
level when you sat at the desk.
I think the main thing though for me is movement is
don't stay at your desk for too long.
There's several studies
that say actually just being inactive,
whether you're in a good posture
or a bad posture, can lead
to musculoskeletal pain and injury.
So it's really important that we get up
and we move regularly.
Movement is medicine. Don't sit for too long.
Keep your joints moving and keep yourself healthy.
How often should I move when I work at my desk?
I think the take home message
for when we're sitting at our desk
and how often we move is move regularly
and keep it flexible.
If people are tied to their desks,
we definitely recommend moving every 30 to 40 minutes
to make sure that you're changing your posture regularly,
but it's safe to slouch.
Don't be worried about sitting in an awkward position.
Just make sure you're not there for too long.
Make sure you stand for a short period.
If you've got the ability to be able to have a sit
to stand desk, to stand for a short period, then
that's great and sit.
Use the front of the chair, use the back of the chair
and vary your position.
I think the take home message is the next posture is your
best posture.
What are the best ways to prevent muscle stiffness?
So muscle stiffness is often seen after exercise.
So if you overload
or you do too much with exercise,
you can develop muscle soreness, which can lead
to muscle stiffness.
Now, delayed onset muscle soreness is very common,
and if you don't manage that well, that can lead
to more persistent stiffness problems.
So how do we negate that?
Now, the best thing to do is make sure you manage your
exercise with adequate warm-up and adequate cool down.
So what we want to look at doing with a warm-up is we want
to gradually increase the heart rate.
We want to put the body through more dynamic movements.
The aim of a good warm-up is
to get the blood flow into the muscles,
get the muscles switched on, get that link between brain
and body firing really quick, so we're reducing the risk
of the body not performing well,
and we know that that's going to mean
that you're less likely to fall or trip
and you're going to have better control of your movement.
The best way after exercise to cool down is
to gradually reduce your heart rate back to a resting level
and calming the tissues down.
So when we're performing,
movement muscles will naturally shorten to provide you
with movement and get the joints moving
so you can move forward or jump higher or move quicker.
What we want to do after that is we want
to return those muscles back to their normal length.
So that's where you can put in your static stretches,
stretching out all the muscle groups that you've used during
that activity to make sure it's specific to your sport
or to your activity,
and that will massively reduce the risk of
post-exercise stiffness and muscle stiffness.
Now, there's other things alongside managing exercise well.
So hydration's really important.
We tend to find when people are dehydrated,
they have a higher incidence of muscle cramps
and they're more likely to develop muscle
stiffness following that.
So keep yourself well hydrated if you know you've got a
performance or an activity or an event coming up.
There's a lot of research behind the effectiveness
of hyper hydrating, so putting plenty of fluid in your body
so it's able to perform well,
and the nutrition is supplied regularly through the body.
We classically see sort of muscle cramps at nighttime,
so good advice is to try
and keep flexible if you are prone to getting muscle cramps,
which we do see with people in later life is maybe look at
stretching before bed and waking up and trying to stretch it
and keep it moving in the morning.
But I think the main thing is adequate warmup,
adequate cool down, and keeping strength and flexibility.
How much should I exercise to prevent joint problems?
It is difficult to give you a generic answer on this
because we're all different.
So exercise is really individual.
Somebody who exercises regularly will need
to challenge their musculoskeletal system more in order
for it to adapt and get strong, as opposed
to somebody who's maybe more sedentary in their lifestyle,
who maybe will only have to exercise at a lower level.
The most important thing I think, is listen to your body.
If you start to exercise where you've not done before
and your body starts to give you signs of distress by pain
or getting aches, or you find it's affecting your function,
then modify your activities
and reduce what you're doing at that time.
Let your body build up slowly.
It takes about six to twelve weeks for our muscles
to get strong, and it's important that we have strength
around our joints to help keep them healthy.
We can avoid injuries to the joint
or problems to the joint by monitoring our weight as well.
There's a lot of strong research to say that people
that are overweight put more load through their hip
and their knee, and that can lead
to more degenerative conditions like osteoarthritis.
Should I avoid weight training exercise?
So weight train exercise is really important
in our weekly exercise routine, we talked about
physical activity recommendations, working aerobically,
but also there's evidence to say that we need
to be working with strength training.
Our bodies adapt to strength training by becoming stronger,
which means we can move our joints more effectively
and we become more functional.
The research shows that after the third
and fourth decade in life, we start
to lose muscle mass if we're inactive,
and that can range between three to 5%
of our muscle mass per decade.
So it's really important
that we keep regular strength training within our exercise
regime, and it's not too late to start.
There's research to show
that in later life if you still engage
with a strength programme, you can still
show strength improvements.
The key of it is ensuring that you do enough
that you do the high enough intensity in order for your body
to adapt and for it to change.
So take home message is stay strong.
Can too much exercise be bad for me?
So exercise is really important.
Too much exercise of course is bad for you,
but regular exercise isn't.
So when we get to a point
where we've done too much exercise,
our body start to tell us about it.
So what we find is we start
to get more post-exercise soreness
that doesn't resolve quickly.
So instead of your exercise soreness lasting maybe an hour
after exercise and having a little bit
of stiffness the following day, that you are in pain
for two days, three days,
and that recovery is taking longer then absolutely,
you've overloaded your body.
And that's when we tend to start seeing injuries
and people start to get pain,
and that affects their function.
So listen to your body as the take home message.
If you find that you're starting to get aches
and pains, adapt your exercise, modify it and reduce it.
Give your body time to adapt
and give your body time to recover.
I think the most important thing
with musculoskeletal adaptation is just being aware
that it is slow to respond.
Give your body time to respond, let it adapt,
and then we'll massively reduce the risks
of you developing any aches and pains from exercise.
Will repeated bending and twisting lead to a problem?
We get a lot of these questions,
particularly when people come in with back pain,
and that myth of bending
and twisting can cause pain, so I mustn't do it.
The problem with that is those myths create a fear,
and that fear prevents people from moving.
And the best way
and the strongest research behind managing back pain
is exercise.
So if we avoid exercise
and we stop bending, we stop twisting, we stopping provide
that rehabilitation that gets our bodies better.
So there's no link between bending and twisting
and recurrent injuries.
Is joint/muscle pain hereditary?
There's no consensus on this, whether the joint
and muscle pain is hereditary.
Age-related changes like osteoarthritis aren't hereditary.
However, there are certain autoimmune inflammatory
conditions that can be so for example,
rheumatoid arthritis is one of those.
So if you are close family members, if your mother
or father has rheumatoid arthritis,
you do have an increased predisposition to developing this.
The older I get, the more likely I'll develop a condition, is this true?
It is not completely true.
What you tend to find is there are age-related conditions
like osteoarthritis, which typically we'll see
the prevalence increases, age increases.
However, there are studies to suggest
that actually back pain reduces in prevalence in later life,
perhaps as our judge start to stiffen a little bit more,
they move less, so less likelihood of overloading them.
However, what we do see as we get older is
that our body's condition and our body's ability to move
and function and balance certainly does deteriorate.
Now, it's important that we help provide the body
with enough stimulus to stop that from happening.
So in later life, as our muscle strength reduces,
keep providing that your body
with enough resistance training, enough strength training
to prevent that deterioration.
It's really important as well,
that in later life you work on regular exercise
to help improve flexibility, to help improve balance.
Because if you are mobile and if you are more strong
and flexible, you're going to have less likelihood of slips,
trips, and falls, which can easily occur in later life
and cause significant impact to your function.
Can I prevent conditions like Osteoarthritis?
Osteoarthritis is typically an age-related condition
and a degenerative condition.
So as our bodies get older on the outside,
they also get older on the inside.
So what we can see in a mirror is grey hair and wrinkles.
And what we see on the inside is that smooth,
slippery cartilage that we have over our joint surfaces
that when we're in our younger years, is sort of glass like
and smooth becomes a lot more roughened,
a bit like a sandpaper.
And it can go through that gradings
of sandpaper as we get older.
And that can have more and more impact on
how your joint moves
and how your body functions,
which ultimately can result in pain
and you needing support to manage that.
So we can slow the progression of arthritis
by keeping good nutrition to our joint, keeping healthy
with a good weight.
So we know that people who are overweight
and carry more load have extra stress
thrown through their joints.
And there's a strong relation between high weight
and incidence of arthritis.
And can we ensure that our joints are kept active?
So regular exercise is another really good way
to help prevent the deterioration of the joint surface
and keeping the joint healthy.
And probably the best take home message with
that is strength training.
The stronger we can get our muscles around the joint,
the more that can offload the work
that the actual joint surface does and reduce that overload
and that deterioration in the joint.
So keeping an eye on weight,
making sure we keep our joints strong.
Also thinking about our other lifestyle choices.
So smoking, we know that has a deteriorating impact
of joint surfaces, so stopping smoking
and also excessive alcohol intake.
So try and make those lifestyle changes earlier on in life
and then we'll be able to keep our joints healthier in later
life.
Can a physiotherapist advise me on avoiding pains and injuries?
Physiotherapists are perfectly placed
to advise you on avoiding and preventing injuries.
Their advanced knowledge on injury management
and rehabilitation helps give them enough ingredients
and enough knowledge to help guide you back.
I think the most important thing is making sure
that you grade your exposure to exercise,
build it up gradually allow the body to adapt.
The research suggests it takes between six
and twelve weeks for muscle tissue to adapt, for muscle fibres,
to become more numerous, numerous, and to become fatter.
And that's what generates strength
and that is what will help keep us healthy, happy,
and functional.
How long should I self-manage any aches and pains?
A lot of injuries can be successfully self-managed,
and as physiotherapists,
we don't see every injury everybody has.
What you'll typically see is small sprains
and strains will resolve quickly within a couple of weeks
as long as you modify your activity and are sensible
and listen to your body.
However, anything that lasts beyond two weeks
that isn't showing signs
of improvement is when you should start
to seek some more support and some more advice,
particularly if your symptoms are deteriorating.
I wouldn't leave symptoms that are getting worse
for longer than 10 days.
However, if there are signs
that you're getting significant changes in muscle power
and you're finding that you're extremely weak,
really quickly seek advice very promptly.
And if you're noticing any abnormal symptoms, pins
and needles, or numbness, you're having difficulty sleeping
because you're waking regularly through the night
because of your pain, then seek some
professional advice soon.
It may be that some early simple intervention can help
manage your condition really quickly
and get you back to activity.
And if you ever find yourself in that stage,
if you're a Bupa customer,
contact our MSK Direct Access service.
Or if you're not a Bupa customer, get into your NHS GP,
or perhaps you can access some self-referral
to physiotherapy.
Does applying hot or cold therapy to aches or pains work?
It's a good question and it's something
that we're asked a lot about.
There's no real significant research to say
that one is better than the other.
However, I do give advice about it,
and I think the easiest way
to look at it is if you've got an acute traumatic injury
where you can see swelling
or bruising, that's a sign
that there's significant inflammation in that tissue.
You'll often feel that it gets hot.
And what does your brain tell you?
Put some cold on it, and that's what I'd go with is listen
to your body, get some cold on it.
Swelling is healthy because it brings nutrients to heal,
but persistent swelling, swelling that stays
around the joint for longer periods can have a big impact on
your recovery and how you function.
So get some ice on it, manage it regularly,
try and get movement back to it.
But ice is great for acute injuries like that
where we can see that swelling.
I'd use heat when we tend to see maybe more muscle injuries.
So perhaps you've overloaded the tissue in the gym
or exercising and it's feeling tight.
Maybe you've got a cramp or a spasm in the muscle.
That's where heat's really good.
Can we relax the muscle to get it back
to its original length and can we calm it down?
So ice in the acute period for those first sort of seven
to 10 days, calm down that swelling, then heat on it
to help try and warm up the muscles around it,
help return those muscles back to their original length
and regain the flexibility and ultimately your function.
How can I stop pains returning?
So management of an injury is really important
to prevent pains from returning as you engage
with the rehabilitation exercise
and get yourself back to normal function.
There's definitely an aspect of maintenance that's required.
Unfortunately, with musculoskeletal adaptations,
if we don't keep stimulating the body with that need
to get strong to help keep flexibility, then we can lose it.
So we hear the phrase that use it or lose it,
and there's definitely a bit of theory behind that.
So making sure you keep exercising regularly.
There are a few studies that say to maintain strength,
you can exercise a couple of times a week to help make sure
that the body doesn't deteriorate further.
So I always recommend when people have resolved their
injury, that there's an ongoing maintenance thing.
Now, that doesn't have to be continued with your exercises
that you've been given by your physio.
It may be get into an activity,
get into a sport that you want to do.
It's really important that you enjoy what you're doing,
and if you don't enjoy the exercise, it's very unlikely
that you're going to maintain it.
So enjoy your exercise.
Find something that you want to do
because you'll keep to it.
And if it's new, build yourself up to it.
Let the body adapt. Let the body change.
Try to listen to your body and don't overload it.
Give that body time to adapt and keep it strong
and that'll avoid any recurrence in your injuries.
What's the difference between acute and chronic pain?
So acute pain is pain
that typically will resolve within healing timeframes.
So what I mean by that is tissues responding
to the body's natural progression
and natural laying down of new fibres.
So that may be anywhere between six and twelve weeks timeframe.
Chronic pain is something that's classified as pain
that lasts beyond that timeframe,
and that's where it can become a little bit more complex.
Chronic pain isn't always linked to just the amount
of tissue damage that has occurred,
and chronic pain can be influenced by a lot
of bio-psychosocial issues.
So it may be your beliefs about your injury,
what your initial thoughts are of how to manage it.
It may be your consequences at home, at life,
your mental health at the time,
and all these very complex aspects
of pain can feed into your pain becoming more persistent
or becoming more chronic.
How long can back pain last?
Recovery for back pain can be really varied,
and this may be due to sort
of the amount of tissue that's damaged.
So if we are looking at a small injury, a sprain
or strain where not many fibres have been involved,
we expect those to resolve reasonably quickly
with modification of activities,
perhaps some pain relief in order to help get you back
to moving and functioning well.
Or maybe if there's more tissue damage
that has a more significant impact on your function,
that you need to let your body have a little bit
more time to adapt.
And those will normally occur between six and 12 weeks.
Now, after that 12 week mark, pain isn't always linked
to the amount of tissue damage that can occur.
And we can find that tissues are actually healing on the
inside, but there is no influence to our pain.
And so the research in the last five
to 10 years has very much looked at persistent
and chronic pain to say that there is no correlation
between pain and tissue damage.
And so what does that mean to you in your recovery?
Basically, listen to your body,
but don't be fearful of pain.
If we're fearful of pain, we're not going to move well,
which means we're not going to recover.
A movement is the best way to recover from back pain.
Our national guidelines recommend exercise
as the premier sort of activity in order
to manage back pain.
So exercising regularly is really important.
Understanding and taking on board that pain
and tissue damage at that stage
of your recovery isn't always linked.
So listen to your pain, but work with it.
Try and focus a little bit more on function.
If you are able to walk for five minutes, day one,
see if we can start to look at progressing that gradually.
And that's the important thing
with our musculoskeletal system.
Give it time to adapt.
So what we'd look at is say five minutes, day one,
let's try seven minutes at day three
and 10 minutes at day 10.
Build it up gradually let your body adapt.
You'll find that your function will improve
and in time your pain will start to reduce.
How can I keep my muscles, bones, and joints healthy?
So keeping our muscles, bones, and joints healthy.
The take home messages, keep active,
that's the most important thing.
Sit less and move more.
There are loads of physical activity guidelines.
The World Health Organisation recommends
we exercise around 150 minutes a week.
So that's looking at 20 minutes at least a day
of cardiovascular exercise.
So that's exercise of moderate intensity, getting you
to a level where you're slightly breathless, still able
to hold a conversation, but maybe having to take a breath
to continue that conversation.
And that should be done regularly
to help improve cardiovascular health,
to help improve muscle and joint health as well.
And I think one thing that's often forgotten
with exercise is strength training.
As we get older in later life, we tend to lose muscle mass
and we tend to lose strength.
So keep in part of that strength programme during your week
and during your exercise is so important.
So keep active, move more, stay less,
and that's the best way to keep your bones
and joints healthy.
What are the key tips for healthy bones and joints?
So keeping healthy bones and joints is really important.
The early we start this, the better the impact.
So we know that keeping joints healthy comes about
by keeping the joint strong.
So we need to make sure that the muscles around
that joint are strong, making sure
that we don't excessively load that joint.
So monitoring
and keeping an eye on your weight is really important.
And also giving the joint enough nutrition, calcium,
and vitamin D are really important.
If we go to the strength training, it's important
and we recommend to people
that they're doing strength training at least twice a week
to overload that muscle in order to keep the joint supported
and keep the muscles strong.
With weight. We know that people
who are overweight put more stress
and more load through the joint surfaces.
So if we look for example at running
where we are massively increasing the load
and the research suggests that can be up
to five times our body weight through our lower limbs.
If you've got an extra kilogramme
or three of weight going through that joint,
you can imagine the stresses
and strains that are going to go through that
and the impact that diet might have,
and also diet and nutrition.
So calcium is really important to make sure that
that's in our diet to help lay down good healthy bones.
As we get older, our bone density reduces
and we see that also in post-menopausal women.
The hormonal support in order
to help keep bone density isn't there.
And so we need to make sure that we have enough calcium
to help support that.
Now calcium doesn't help to provide strong bones on its own
and it needs vitamin D and we absorb that from the sun.
So in the summer months in the uk, we're okay.
We might be covered if there's enough skin exposure.
However, in the winter months when we not have
as much skin exposure, it's important
to supplement your diet with vitamin D
to help reduce the risks of changes in bone density.
So to summarise, keep strong,
make sure you're not carrying excess weight.
Keep nutrition to the joints.
And I think the other things to keep in mind of is
not taking too much excessive alcohol and avoid smoking.
Where can I go for useful information about muscles and bones?
I always recommend people look for sources
that are ratified and that are trusted, so go to Bupa.
We know that the literature
that's published on our website has been ratified
by professionals, and it's been reviewed to make sure
that it's in line with good recent evidence-based practise.
Of course, we've got lots of research
and sources through the NHS as well that you could look at.
So look at reputable names that
provide good sound health advice.
When should I seek professional advice and treatment?
So I'd always encourage people
to seek urgent advice if they're finding
that their symptoms are deteriorating quickly.
If you're noticing that you've got any neurological
compromise, what I mean by that is if you're seeing signs
that you're getting any numbness in the body part,
if you notice any pins
and needles, if you find
that you're getting any deteriorating muscle power
or urgent weakness, seek urgent advice.
Any other abnormal systemic symptoms as well.
So if you're starting to develop a temperature, a fever
that might be causing night sweats,
or you're starting to see a significant weight loss,
always go and seek urgent medical advice.
And that may be if you're a Bupa customer,
contacting us at MSK direct access service,
or if you're not seeking advice
and support through your NHS GP
or maybe your self-referral physiotherapy.
How do I access support through Bupa?
If you're a Bupa customer, we can help you
through our MSK direct access,
or you can speak to a physiotherapist
through our digital GP app,
or you can access our Anytime Healthline nurses
who are available 24/7.
Explore muscle, bone and joint care with our experts
Inside Health:
Joint health and movement
TV medic and presenter Dr Zoe Williams discusses joint health and movement with a panel of Bupa physiotherapists.
Hello, and welcome to our second inside health event of the year.
Today, we're got to be talking about musculoskeletal conditions, which we'll often call MSK for short.
And these are conditions that affect muscles, bones, and joints.
And they're conditions that affect millions of people every day.
So it's a really important topic to cover.
And today, we are joined by Joseph Askew, who is Bupa's advanced physiotherapy lead, discussing the huge issue of arthritis.
Different types of arthritis, how people living with arthritis can manage their condition.
But also importantly, we'll be talking a bit about prevention as well.
And I'm also joined by Emily Partridge, and we'll be discussing my favourite topic of exercise and movement.
Emily is Bupa's Clinical Lead for MSK.
And we'll also be talking about what you can expect from the physiotherapy service too.
We'll be answering loads of your pre-submitted questions, but if you do have any more specific questions that relate to you, then please do feel free to get in touch with the Bupa team.
What is arthritis So my first guest, Joe.
Joseph Askew, you are the advanced physiotherapy lead at Bupa.
So your role provides customers with effective care navigation to ensure that they access the right clinician to manage their problem first time, every time, which is so important.
So welcome, Joe.
Thank you very much, Zoe.
So let's talk about arthritis.
It is a huge topic that affects so many people.
It affects in fact, more than 10 million people just in the UK.
And that includes people of all ages.
So it's a big concern for our viewers.
We chose to focus on this topic today, because it does affect so many people.
And I think let's start off.
First of all, can you explain what arthritis is?
We can.
So arthritis, the definition of the word just means inflammation of a joint.
And so we classically think of arthritis as being a problem that causes pain and swelling and inflammation affecting a joint or in most cases, several joints.
And historically, we've always thought of arthritis as being a process of thinning of the cartilage, where the cartilage is gradually affected and starts to narrow.
And we commonly see that with age.
One of the problems that we always encounter with medical language is that we use lots of different words interchangeably.
So you'll hear people describe arthritis as arthrosis or as arthralgia, that's quite common.
Historically, people have often referred to arthritis as wear and tear as well.
And you often hear people describing crumbling joints and degenerative joint disease.
And this is a really important thing for us as healthcare professionals to try and overcome, because the language that we use is so important in framing things for people, and the message that we're trying to confer.
And using that language around generation and where in tear, you risk instilling fear in people.
And particularly, fear about activity.
When activity, we know is really advantageous for people with arthritis.
Types of arthritis - Yeah, it's interesting, isn't it?
I think in a lot of the work I do, working with healthcare professionals, I'm encouraging people to stop saying, wear and tear, and talk about wear and repair.
Absolutely.
Because actually we know that activity, well, it's one of the main treatments for arthritis, isn't it?
It is.
Yeah.
And there are different types of arthritis.
So can you talk us through what are the many different types, but the main types of arthritis?
Yeah, so there's over 100 types of arthritis that's affect people right the way from childhood and early adolescents, right the way throughout our lifespan, by far the most common is osteoarthritis.
So we actually know that of that population of people with osteoarthritis, two out of every three of them will report that they will last pain free over a year ago.
So this has a huge effect on people, and it's a very disabling problem.
And osteoarthritis is this process of inflammation and swelling within the joints that causes pain and disability.
And we can think of this in two different ways, really.
We can think about it as a disease.
And so as healthcare professionals, we like to define things and we like to stage them.
And so disease helps us as healthcare professionals to talk about arthritis.
It's more important to think of it as an illness though, and that's the way that it affects people.
And so these are the symptoms that people experience of loss, of quality of life, of pain at night that stops 'em from sleeping, and of not being able to participate in the activities that they like to do.
And so that's by far the most common type of arthritis.
And that's kind of, I think when you were talking before about rheumatoid arthritis the less helpful language that might be used for the joint crumbling or wear and tear.
That's kind of we were talking about osteoarthritis there weren't we?
We are.
Because we see a very different picture- - Yes.
Yes.
In what I think you're probably got to say next.
Oh yeah.
Which brings us onto rheumatoid arthritis, which is by far the more common of the inflammatory arthritis.
And this is a very different type of problem to osteoarthritis.
So and rheumatoid arthritis, is what we call an autoimmune disease.
Which is where the body's immune system starts to attack the joints themselves.
And this can cause quite marked erosion and destruction of a joint.
The inflammatory process, it goes alongside it.
And that's a huge problem.
We don't really know what triggers rheumatoid arthritis.
We know that there are some potential links, and some of these around lifestyle.
And we know that smoking is a potential real contributor to developing rheumatoid arthritis.
But there are also things like viral illness.
There are some links with diet that we'll discuss a little bit later.
There are also other kinds of inflammatory arthritis.
So there's psoriatic arthritis that's linked to people with psoriasis.
And then most people will have heard of gout.
And gout is also an inflammatory arthritis, where people have too much uric acid in their system.
And that starts to get deposited into the joints as a crystal structure.
And sometimes if that process is happening, they might knock their joint and stub their toe, is a common one, and that can disturb those crystals, and that causes a significance inflammatory response that's extremely painful, and is associated with a hot, swollen joint.
And I guess the big difference there is rheumatoid arthritis tend to usually affect a number of joints, whereas gout tends to just affect one joint at any one given time.
And usually it's the one that connects the foot to the big toe most commonly, but not always.
Okay, and I think one thing that is in common with all those, maybe not gout actually, but with osteoarthritis and rheumatoid arthritis, is that actually exercise and other elements of lifestyle are quite important management.
Very much.
So, really important.
And we know that there are lots of lifestyle contributors particularly to osteoarthritis.
So what we see is that obesity is a real contributor to developing osteoarthritis.
Just, it's the load, isn't it?
The extra load that the joints are carrying.
It is, it is.
And also obesity tends to go hand in hand with other, what we describe as metabolic syndrome.
So you see more commonly raised levels of cholesterol.
You see more commonly diabetes, and you see more commonly high blood pressure.
And we know that all of those things are linked to developing osteoarthritis, as well as contributing to the symptoms that people experience from osteoarthritis, and also with rheumatoid arthritis.
And so anything that we can do to help with those and impact those, is a huge benefit for people with arthritis.
So obesity is a risk factor, age is a risk factor.
Although it can affect people of all ages, I think that's probably the number one as well, isn't that?
It can.
And with osteoarthritis, we tend to see that developing in people over the age of 45, really, because under the age of 45, that repair process that's happening in all of our tissues is able to keep up.
Whereas once we start to mature, the repair process can't keep up as well.
And we see that in all of our collagen tissues.
That's why we develop wrinkles and that's why we can start to develop issues within our joints.
diet and arthritis - Now, you mentioned earlier that you'd share with us more info on how diet is important when it comes to arthritis.
So can you tell us a bit more about that?
Yeah, so we know that with rheumatoid arthritis, that high caffeine diets, diets that are high in red meat, are potential contributors.
Seem to contribute to potentially developing rheumatoid arthritis.
We also know that obesity, as we've discussed is, has a huge impact on osteoarthritis, both developing osteoarthritis, and making the symptom profile that people experience worse.
And so anything that we can do to help to impact that can have a profound effect.
There was a relatively recent research study that showed that in people who were obese.
So in people who have a BMI of over 30, if they could reduce their weight by 10%, with a combination of diet and exercise, that their pain levels improved by 50%.
So you don't have to have a huge impact on BMI to start to have a big impact on the symptoms that people experience.
exercise doesn’t cause harm - Yeah, I think there'll be many people who will be thinking easier said than done, especially when your joints hurt, but also, I think for a lot of people, just having that knowledge, that can be a real motivator.
That can be the thing that makes them think maybe they've tried things before they want to have another go.
Absolutely, and I think one of the key messages from this is for people to understand that exercise doesn't cause harm when you have osteoarthritic joints.
Obviously it can be really difficult for people, because everyone's experience is different, and pain can be a real limitation for people.
But we know that with physiotherapy, we know that with exercise, and we know we've got good strategies to treat the illness.
And so if people reach out to healthcare professionals, there is a lot that can be done.
And people shouldn't be fearful of moving and exercise and activity.
I think the other thing in my experience joint replacement surgery is people are aware of joint replacements for needs and hips in particular.
And I think, sometimes people delay coming to the doctor or to the physio and seeking help, because they think that that's the only option and they don't feel ready for that.
They kind of think, "I've got another couple of years in these joints.
" But actually as soon as you're having problems that are impacting your quality of life, stopping you doing the things you want to do, there are so many things working with physiotherapists and other members of the team that can be put in place to help and support them, and maybe even prevent that surgery being required down the line.
Absolutely.
And I think there's a real perception that having a diagnosis of osteoarthritis, inevitably leads to a joint replacement surgery.
And that there's nothing that you can do in that middle ground.
You've just got to wait it out until your symptoms are such that you are offered surgery.
Whereas we know that's absolutely not the case.
It's actually, if we look at knee arthritis, knee osteoarthritis, it's actually quite a small percentage that progress to having a knee replacement.
Less than 10% in some studies.
So there's a lot of people out there that manage really well without surgery.
And some people do need surgery, and surgery for those people it's incredibly effective.
It's a great operation.
It really is.
Yeah.
advice for younger people I think a lot of people are worried about that operation.
But it's such a wonderful operation.
I remember an orthopaedic surgeon when added my orthopaedics rotation, the surgeon saying, "Tell your patients that the day after their operation, yes they'll feel pain, yes they might feel a bit woozy, but that joint, that's the best joint.
That's the best their joint's been for years.
And that joint's ready to get up and go.
" And to give them that confidence that actually, for so long it's felt unhealthy, but that joint is now good to go.
Joe, one of the common misconceptions is that arthritis is a condition that only affects older people.
But what advice can you give generally to younger people?
So arthritis much more commonly affects people over the age of 45, but we see it in younger people also.
And often that's as a result of injury.
So one thing that people can do is take part in injury for prevention activities, and people can guide that from a physio point of view.
There's also really important lifestyle considerations.
So healthy lifestyle, reducing obesity, reducing blood pressure, reducing cholesterol, we know contribute to reducing the lifetime risk of osteoarthritis.
symptoms of arthritis - When we're thinking generally about arthritis, and we're talking mostly about osteoarthritis here, we know pain.
Pain in the joint, and that pain can be in different places, can't it?
People can have arthritis in their knee, but they can feel the pain in their hip or the other way around.
What other symptoms do people report?
It's often such a broad thing, because people's experience of pain and people's experience of disability that can come with osteoarthritis can be really varied.
And so classically, it's pain and stiffness and a feeling of restricted range of movements.
So quite often, one of the things that people start to notice with hip arthritis, is that they can't bend forward to put their shoes on or their socks on because their movements starts to become a little bit restricted.
With people who develop arthritis in their shoulder, they can't get round to their back pocket or tuck the shirt in round at the back.
And so it's that restricted range of movement that then starts to lead to functional loss.
So you start to struggle with your normal day to day activities, and that can then start to impede quality of life.
But it's really important for us to remember that arthritis and any kind of arthritis is a whole person disease.
This isn't just centered on the joint itself, per say.
We've got to think about the impact that not sleeping has on people.
Because one of the really common symptoms of arthritis is night pain that wakes people up, and not sleeping can have a really profound impact.
These are often working age people, and that can have a really profound impact on work.
Can have an impact on your ability as a parent, and all the other things that we have to do day to day.
when to seek help - Joe, I think what the viewers would find quite helpful would be, how do you differentiate between the sort of normal aches and pains of getting older versus early signs of arthritis, When you should seek help and go and see someone?
There is some overlap between what would be early arthritis, and what would be normal aches and pains associated with starting to get a bit older and periods of increased activity.
I think the really important thing is for people to know and understand when to get help, and when to access help from their doctor, their GP, or when to access help from another healthcare professional, like a physiotherapist.
And really, that comes down to quality of life and their ability to function.
We tend to go off the patient's experience, and if they're starting to struggle with normal day to day things, and it's starting to impact their life and it's impacting their quality of life, that's the time to access help.
Because we know that we can put some strategies in place to help deal with that and do something about it.
The same goes for night pain.
I think, there can be several different things that can cause night pain.
But if people are experiencing night pain, then I think really they need to get in touch with their GP and have a chat about that.
stigma - And I will say if in doubt, just get it checked out.
I think that there's a lot of stigma, I think, associated with aging and a lot of acceptances of arthritis is just a condition that you get when you get older and you should just put up with it.
And I think, our main message here would be, don't put up with it because there are things that could be done to help.
So don't suffer in silence.
So what are the various treatments available there?
So really, the first line treatment with this is education, and advice, and understanding is speaking to someone to frame things in the right way and discuss what you can do, and what help you can access to manage these symptoms.
And that should be the first line treatment.
It can make all the difference to someone actually benefits of exercise just understanding more about their condition and what they can do themselves.
If exercise was a pill, everyone would take it.
Because it's not just the impact that this has on reducing your likelihood of developing osteoarthritis or reducing the symptoms of osteoarthritis that you experience.
Addressing those things also reduces your lifetime risk of developing dementia.
It reduces your lifetime risk of cardiovascular disease, heart attack, stroke- - Breast cancer, bowel cancer.
Yeah, mental health.
There are a myriad of things that this influences, and it's so important.
And so at the basic level, it comes down to that advice, education and exercise.
And it's that whole spectrum of care, isn't it?
Emily Partridge Available from the advice and understanding all the way through to surgery.
And that's why it's so important in your role that you are helping the individual person find the right clinician to help them right at the beginning.
That's it.
And to see where they fit along that spectrum.
Thanks, Joe.
That's so helpful.
So I'm now joined by Emily Partridge, who is Bupa's MSK Clinical Lead.
And Emily's a strong advocate of promoting health and wellbeing and providing a holistic approach to client care.
Hi Emily.
Hello.
So we're got to start by talking about exercise and movement, because there's this common belief that if you have a condition that's affecting your muscles, bones, and joints, then the best thing to do is to stay still.
Now, I definitely disagree with that one.
Yeah, it can be a common misconception actually.
That if someone's diagnosed with a problem with their muscles or bones or joints, that they think, "Oh, I better rest.
" Going back many, many years, that probably was the advice about, for example, if you hurt your back to lie down, actually as physios now, that's the absolute opposite of what we'd be saying.
It's the worst thing you can do about.
Actually, it really is.
And actually, yeah, exercise is really good for you, and it's got to have lots of benefits.
While the lack of exercise could potentially cause some harm, really.
There's so many benefits of exercise.
So you keep your joints nice and lubricated, moving freely.
You keep your muscles nice and strong, your stability, your balance.
But also, it's so much wider.
There's just so many benefits of exercise.
Things like improving your mood, your energy levels, your sleep, which we all know is super important.
Exercise can boost your immune system.
It's great for confidence.
It's great for maintaining your independence, and great for socializing as well.
So I'm definitely a massive advocate of exercise in all its benefits.
Absolutely.
How can you be sure you're doing the right types of exercise if you have particular condition, or maybe even if you have an MSK injury?
Yeah.
I mean, it depends on what that is.
And I'd always say, seek advice from a healthcare professional, such as a physio.
I'm going to be biased for physio, and Joe is too.
But we are very, very good at guiding people into the right type of exercise.
But generally, I'd say listen to your body.
If things are aching after exercise, actually that's a good sign.
It probably works.
It's working, it's doing something.
The changes that you want to happen are happening.
Absolutely, if suddenly your pain's getting significantly worse, I'd suggest we might need to adapt some things here.
That's not to say that we need to stop the exercise that you are doing, but there may be some things we just need to adapt maybe, the time that you're exercising, or how often, or let's say, if you' a runner, runners are quite notorious for just running.
And I get that, 'cause there's lots of advantages.
You just literally put on your stuff, go out the door and run for half an hour.
But I always say to runners, try and vary up a little bit.
Do some cycling or swimming.
Do some strengthening stuff, maybe bit of stability, mindfulness stuff as well.
So my general advice is seek help from a professional first of all.
Don't be disheartened by having an MSK condition, and really kind of think of it as motivation go forwards with it, listen to your body: aching spine.
If something's quite sore afterwards, don't worry.
Maybe just seek advice and adapt it a little bit.
So generally then, I think, we've all agreed that for most people getting moving is definitely advisable.
Does it matter how old we are, or how active we've been in the past?
Is it ever too late to get started?
Never.
Never, no.
Absolutely, no.
It doesn't matter how old you are, whether you've exercised before, hand or whether this is something new that you want to start doing, it's never too late.
I'd just say, look forward, try it, try different types.
Make sure you choose one that you enjoy, and then just reap all the benefits from it.
And if people are apprehensive, maybe because of their age, or it's been a long time since they've done anything, or because they do have joints that are sore, how can they get started?
Or how can you give them the confidence to take that first step?
What sort of things can they begin with?
Yeah, so I think that's where seeing someone like a physio is really helpful.
That might give you that confidence.
'Cause if you are worried that you're going to cause harm, for example, then already you're starting on the back foot a little bit.
You want to feel really positive about it.
So I definitely sort of seek that guidance, first of all.
Talking to people as well.
Again, I talk about socializing with exercise.
Speak to friends.
See what they like, go and join with them.
Sometimes if you're walking into a class on your own, that can be quite daunting.
Well, if you're going with a friend, it's a great chance to catch up as well and you can join it.
Your friend might like it and you might not like it, doesn't matter.
Nothing's been lost as it you've given it a go.
Also means you're committed as well, doesn't it?
Once you've made that plan with a friend.
Yeah, once you've said it out loud- - It can work out.
Yeah, absolutely.
So it's a good way of making a commitment.
So moving on then Emily, are there any exercises that you should absolutely avoid if you have an MSK condition?
I think running is an example, I hear lots of patients say that, "I've been told I shouldn't run anymore, I should cycle instead.
" Yeah.
So you hear quite a lot about how running causes arthritis.
And actually that's really not the case.
Evidence these days shows that if you are running, enjoy running and you've got arthritis, please continue to run 'cause actually it can reduce your pain.
That's interesting, isn't it?
Really interesting.
A lot of people will be, I think, confused by that.
Yes, and I think I was actually at spin class the other day and there was a gentleman next to me, and he's got sore knees, and he's like, "Oh, it's all the exercise I've done in the past.
" And I had a good chat with him about actually, "No, that exercise didn't cause your knee problems.
In fact it probably prevented more knee problems than you've than you've got now.
" So I think running gets a bit of a bad name, and actually there's no reason for that.
If you are a runner, or you want to start running and enjoy running, please do, go ahead.
That's also to say running isn't the answer to everything.
Again, try a different.
If you don't want to try running, try something else, try this.
The beauty of exercise is there's so much variety.
Whether that's outdoors, whether it's indoors, whether it's at home, whether it's in a gym, whether it's in a class.
So yeah.
I wouldn't say there's anything particularly to avoid.
Again, depending what that condition is, I'd always caveat that if you are seeing a health professional, they may be able to guide you and say, "Maybe just right now, maybe don't do this just while you're recovering.
" That's not to say you can never do it.
But there might be just some adaptations that you need to make short term.
So in summary then, Emily, all of us can benefit from exercise.
Irrespective of our age, irrespective of what MSK conditions we might have.
And I think sometimes getting a bit of advice from a professional like yourself, can really help give confidence and guide people further.
Yeah, and it might just be just a one off appointment with someone like a physiotherapist, that can absolutely be your key aim for going for physio, can be just, "I'm okay with whatever my condition is, but the purpose of why I've come here is I just want some guidance about what exercise do.
" Physios will love that.
They will absolutely embrace that a person has come with that motivation.
So yeah, they'll be more than happy to see you.
Brilliant, thank you very much.
I want to move on now to talking a little bit more about physiotherapy, your role as a physiotherapist, what it entails, what people can expect when they go to see a physio, and also what sort of treatments that you might do if somebody is referred for having issues with their bones, muscles, and joints.
First of all, physios are health professionals who specialize, if I talk about MSK physios, specialize in the assessment and treatment of conditions affecting muscles, bones, and joints.
And what we do, is we work very closely as a partnership with the patient to help to restore movement and function and reduce pain.
A variety of different tools that we use are very much education, exercise prescription.
There may be some hands-on.
So joint mobilizations, massage techniques, were appropriate.
But it's that real partnership between the clinician, the physio and the patient, to really set goals according to what the patient wants to achieve.
And then working together with them to achieve them.
So if I, for example, get referred by my GP for a course of physiotherapy, what can I expect to happen?
Okay.
So you'll come and see the physiotherapist.
And first of all, they'll have a really good chat with you.
So that will be all about.
They'll be asking questions about the condition or the symptoms that you're getting, how they affect you?
what makes them worse?
What makes them better?
But really importantly, we find that about the person.
So you never just a knee or just a back, you're a person with knee pain or a person with back pain.
And I think physios are very, very good at that.
And often we have the time to do it in the appointment, as well to really find out about that person.
So what do they do if they're working?
What do they do work wise?
What do they do in their leisure time?
Have they got any dependents?
What's their sleep like?
What's their stress levels like?
Are there any past medical history, so other conditions to do with their health that might be contributing?
So we find out all about the person, first of all.
And I think really importantly, what makes them tick?
As well What do they think's going on?
What do they think's causing it?
And what would they like to achieve from physiotherapy?
So once we've had a good chat, then have a look.
So again, depends on what the person's coming with.
Overall, we look at posture, we look at movement, we look at muscle length, muscle strength, stability, balance, and get a really nice overall picture.
And from there, we try and formulate a clinical impression as to what we think might be going on.
We'll then sit down with the patient and talk to them.
And again, this bit's really important as well.
Talk to them about what we think might be going on, but in a way that someone can easily understand.
To try and sort of de medicalise things as well to normalize things, I think, is really important.
And also give the opportunity for the patient to ask questions as well.
That's super important.
From there we'll work.
So we'll put it all together.
It's like a jigsaw puzzle.
So finding out, if the patient is worried about something or actually, can we talk about that?
Are there only reassurances that we can give to them?
From there, we'll start to formulate a treatment plan.
And that's very much just shared decision making.
So not one size doesn't fit all.
So there may be different treatment techniques available.
We might give those sort of choices to the patient, and then work together as to what we might try first of all.
We set goals as well.
So functional goals, realistic goals.
So that there's a real sort of target to aim for.
So the aim is when the patient comes out, they know what's sort of going on.
Its sort of a clinical impression.
And feel quite empowered by that, and quite comfortable in that they've had their questions answered, they've got a plan, and they know sort of what they can do about it going forwards.
This is quite a lot then that goes on in that first consultation.
Really is.
And that really holistic view where there are two experts.
There's physiotherapist, but also the patient, and recognizing the knowledge and the ideas that they have.
It's much, much more than the physio's got healing hands and can cure you after few appointments.
Oh, no, no, no.
Sadly that's not the case.
So what should a person consider, or how can they prepare as well prior to coming for a physio appointment?
So the main thing, I would say, is that commitment and making sure that they they've got the time and the motivation to be involved with physio.
So yeah, physio is absolutely a partnership.
You mentioned there about the healing hands.
So I mean, I'm sure I've had many experiences and Joe, I'm sure you have as well, where you get a patient coming in and they sort of dive for the bed.
(Zoe laughing) - Thinking that you are going for- - Is this where I lay for my massage.
Yeah, exactly.
And these wonderful magic healing hands are just going to sort of touch you and make you all better.
We're not magicians.
It's not that easy.
There is a place for hands-on therapy, not for everyone, but for some there is.
In the world of physio, there's all sorts of debates that go on about sort of hands on or not hands on.
And I personally think that there's a room for everything and it's that individualized approach.
But I think it's that commitment.
You could do some massage techniques or joint mobilizations.
Likely the patient's going to feel, "Oh, I feel nice.
" And walk out the door and think, "Oh, how wonderful that was.
" But if they then don't do their exercises, or change their lifestyle, or change their posture, they might feel better for the rest of that day, but it's likely, to be honest, that after that day, their symptoms will probably return.
You've got to get to the root cause of things.
And joint stiffness or a tight muscle, is often a symptom rather than the cause.
So yeah, if you're going to go down the physio route, I think it's knowing that from the start.
Don't dive for the bed and expect a magician's healing hands.
Be committed to it.
But actually know that that partnership can work really well and really long term benefits.
I think it's so important that people know that this does require work.
It requires effort.
And sometimes it might not be the best time to therefore be going to physiotherapy.
If you're got to be traveling abroad a lot or whatever, but actually having said that, physiotherapy, because it's actually predominantly not hands on, it can be delivered in lots of different ways.
You don't actually physically need to be with a person in the room, do you?
You can do it virtually.
And I think probably the pandemic has shown as just what is possible.
So what different ways could you treat somebody?
So this is really exciting, I think.
So traditionally, physio has been face to face.
There will always be a place for face to face physio, and rightly.
So there's certain conditions or certain assessment techniques that we would like to do as a physio, or treatment technique for certain people that we'd like to see them face to face.
However, much of what we do in face to face physio, we can actually do now virtual.
And you're right, the pandemic really brought that to the forefront.
And actually Bupa works at the head of the curve on it.
We've had telephone triage physios for about 10 years now.
The fantastic customer feedback too.
But definitely now post pandemic, the video capability, as well as apps that come in.
So if you think a normal physio session is, as I say, finding out about the person, you can actually do that over the screen.
You can look at their posture, their movement, their balance, you can even assess muscle strength by getting them to lift certain things.
Look at the way they're moving those sorts of things.
You can talk about a treatment plan.
You can set goals all virtually.
The beauty of virtual is, let's say your appointment's half an hour.
Well actually, literally virtually it takes 30 minutes of a day.
If you go to face to face, you've got to travel somewhere.
We all think, "what if there's traffic, we leave time.
" "Oh, I better get there a bit early if there's any-" - Okay.
Yeah.
And actually, that half an hour might be an hour and a half, two hours of your day, while there.
Exactly what time, you can go about your daily business.
You log on, you do your stuff, have a great conversation with the physio, know exactly what you do, log off and carry on with general life again.
So another change in the physio world as well, is I think, historically people think that they're going to come for a course of physiotherapy and that can put people off thinking, "I've just not got time to go to five sessions of physiotherapy.
" So actually a lot of people can come now for maybe one session, maybe two sessions, where they just want that expert advice for the guidance.
We can then send them some exercises via email.
They can either read the script of which explain tells to the exercises and there's pictures, or they can play a video as well.
And I think talking about exercises, it's really important to say that physios are humans as well.
I think at times, people think physios are sports mad, and eat super healthily all the time.
And they may feel a little bit intimidated by coming, or think we're got to give 20 odd exercises.
Now that's not the case too.
We are, as I say, humans.
We are short for time, just like anyone else.
We have dependence just like anyone else.
So we will, on the whole, set maybe three or four exercises to do.
It's way more about quality rather than quantity.
We'd rather be realistic and know that the patient's going to feel on board and empowered, and feeling good about those exercises, than we give them 20 odd things to do that they may be really good at doing day one, and then life gets in the way, and they don't quite get round to it.
And then they're dreading coming back to the physio thinking, "Oh, crikey, I've not done my exercises.
" And all that side.
So yeah, physio's changed a lot, but I think my main message with it is, as I say, that real partnership, it's a really positive experience, I would say.
And it's really that empowerment of the patient.
And it's just your experience as well.
You've worked with so many different people from so many different backgrounds, that whatever anyone shares with you, whether it's the lack of time, you've heard it all before.
Absolutely.
You're able to adjust an amend to fit a person.
Yeah.
Yeah.
I think it's a real honour to be a physio actually, because we get to spend- - Same as a GP.
Yeah, we get to spend a lot of time with people.
And I've always found really learning about the person in front them being really interesting.
And at university, you think that these patients all fit really nicely into boxes.
If you're this about the knee, you treat it this way, and this is exactly what's got to happen.
You soon realize that that is not the case because different characters, there's different stress levels.
And I think, the beauty of it and the real, it's finding that sweet spot of giving a patient something that they really feel excited about, empowered by, and that it's realistic and that they see results as well.
Because now as interesting as folk, as they say.
But I think now you've outlined all of that.
My question is, what would you then say to somebody who feels afraid or is holding back from seeking help if they've got pain, and instead they're choosing to Google it and self diagnose and self treat, is that advisable?
I mean, the world we live in is fantastic, isn't it?
The information is just at our fingertips.
When it comes to health, though, I think it really depends where you are looking, and why you are looking.
So if you are trying to get a diagnosis, I'd probably steer away, because it's likely you'll find something, and I will put my hands up.
I have done it myself.
Where you sort of, you Google something and you suddenly think, "Oh my goodness, I've got some horrendous disease going on.
" Well, for example, Google chest pain, first thing that'll come up is a heart attack.
Exactly.
Exactly.
It's not communis causing chest pain.
Which is going to increase all your symptoms and worry.
And it's just not a healthy way to go.
So I would say from a sort of diagnosis point of view, I'd always advocate going to a healthcare professional.
So it may be just a one off appointment that's needed to give that reassurance expert advice set you on your way.
If you are going to sort of access healthcare via the internet, Just make sure it's a reliable source.
So things like the NHS websites, very good, things like patient info versus arthritis, if you have had that diagnosis of arthritis.
And things like the Bupa website, it's full of health content that's written by clinicians, it's reviewed regularly.
So it's all up to date as well, because otherwise you can really convince yourself that you've got something horrible, when actually, it really might not be.
Yeah, and of course, for Bupa customers as well, if there is something more specific, they want advice or they're not sure where best to go, they can contact Bupa and just put an inquiry and find out what to do from there as well.
What about kind of the more small and niggles and pains, the things where we don't need to seek help, how should we tackle those?
Yeah, so if it's a niggle that you've experienced before, and you've sort of self-managed before, I'd try whatever you tried beforehand, and see if that works again.
If it's something where you think, "Oh, my back's got a bit of a niggle but actually when I think about it.
It's probably because yesterday I was all day on the laptop on endless conference calls, and/or I moved to house last week.
" Have a think about what you've been doing and see, if I give the example at that laptop, well, for the next few days, I mean, ideally forever more, but particularly the next few days, really have a think about your posture.
Get up regularly, do your work calls walking around, for example.
And just see if it's settled.
And most of the time, those small niggles and pains will settle.
If they don't settle, then I'd say, yeah, go and go and get that reassurance.
Get someone to look at it, give that reassurance.
And particularly you're worried about it.
I think, worry can make symptoms so much worse than they are.
And it can sort of create quite a snowball.
So if you worry, just go and seek help, and have a chat with a healthcare professional who can reassure you.
Yeah, definitely.
I think it's important that, isn't it?
Thinking I think often we accept these niggles that, "Oh, my back's sore again.
" Thinking about the root cause, "Why is my back sore?
" It's fine taking painkillers every now and again, and doing some exercise and stretches as to remedy it.
But it's also worth just having that thought about, well, what could be causing this.
I never used to get this problem, what's changed.
Final question, can you tell us what support is available to Bupa customers?
Okay, Lots, lots is my answer.
So the great news about if you are Bupa customer and you want to access physios, you don't need to go to your GP first of all.
Which is, I mean, it would've been great in sort of normal times, particularly right now.
We all know how difficult it is at times to get to seek GP advice.
And one in three GP consultations apparently are about musculoskeletal conditions.
So the great news with Bupa, is you don't need to go down that route, you can self-refer.
When you ring Bupa insurance, they will then book you in with one of our virtual triage physiotherapists, which is normally within about 24 hours as well.
So that's great.
You can speak to someone really quickly, really experienced physiotherapists.
They will triage you.
So that is sort of deciding what the best next steps are.
That might be in a very small number of cases, but might be that you have to go to.
They might recommend you go to an accident in emergency department.
It may be to see a consultant.
The vast majority will be either sort of physio, osteopathy sort down the therapies line, or this self-management group as well.
And we actually find now with our virtual triage physios, that about 20% of people who are calling, actually go down that self-management route with really fantastic, as said before, customer feedback about, great I access someone really quickly, I nipped it in the bud, I feel empowered.
I've got my exercises to do.
That's all I wanted, really.
So that's our sort of virtual physiotherapy route.
Then if you have seen a GP and they've recommended you that you see a consultant.
So for example, a trauma and orthopaedic surgeon or a neurosurgeon, when you ring up to get your authorization code, they will offer you a call with Joe's team, our advanced physio practitioners.
And that's amazing service that we've started about a year ago with amazing customer feedback.
Where actually it's, again, a talk with an expert to really delve down a little bit deeper into this issues, and really make sure that the consultant referral is the right referral.
As you were saying earlier, about seeing the right clinician at the right time.
And sometimes- - Well, I think a lot of.
Everybody's energy and time can be wasted and conditions can deteriorate if you're seeing the wrong person in the first instance.
Exactly, yeah.
So they'll have a really good discussion.
If the advanced physio practitioner thinks that you still need to see the consultant, fine.
And actually you are then, still seeing the consultants, you're still getting on the same line, but you're armed probably with a bit more information.
They may give you sort of a bit of stuff that you can be starting to get on with while you're waiting for the consultant.
But there's also a big proportion now, actually they have that conversation, and they decide together that something like physiotherapy might be a good route if they've not tried it before.
So that's a really good service that we've started now.
We've got the Bupa website, as I mentioned earlier, which has got a wealth of content on about all sorts of musculoskeletal conditions.
So have a look there, and then we've also got our Bupa health centers as well.
So these are centers dotted all around the country with regards to MSK.
We have teams there of physiotherapists, osteopath, podiatrist, and our MSK physicians who are consultants who specialize in sports and exercise medicine.
So you mentioned the start about that holistic view that I love.
And that's what I love about working in the Bupa center is that real sort multidisciplinary team, we work as a team treating that individual person with them at the center, and them involved in their care.
So our Bupa customers can access those Bupa health centers as well.
Well, thanks for that, Emily.
Obviously a great range of help available for people.
And next, I'm got to bring Joe back in.
Actually, I'm got to chat to both of you 'cause we've got some questions from our viewers.
So as ever with these events we've received a whole bunch of questions from customers.
So we're got to get through as many as we can in 10 minutes.
And the first one probably for you, Emily, I'm a runner.
Is running on certain types of surfaces better or worse for your joints?
For example, is grass better than running on a road?
Okay, so it's a question that's often asked, that one.
There's pros and cons of different running surfaces, to be honest.
So road running.
The advantages are, most roads, although I caveat out that with potholes, are smooth and they're sort of even generally.
So that's an advantage.
The downside is that there's less shock absorption when you road run.
So potentially you're putting more stresses through your body, which may potentially cause more injuries.
If you then consider something like grass, it's softer.
So you've got the advantage of more shock absorption, but then you get into the realms of, is it uneven?
if it's been raining, then the grass is slippery.
So I wouldn't say that there's an ideal running surface out there.
As a general rule, probably vary it up.
Because actually when you're running on different surfaces as well, you're using slightly different muscles.
So that's good.
It gives a more overall sort of workout, I would say, and potentially prevent injury, rather than just pounding in either just purely on ground or purely on grass.
Okay, I love that.
Mix it up.
Mix it up.
Yes.
What advice can we give about coping with managing sciatica pain?
Who wants that one?
I'll take that one.
I would say, seek help from a health professional in the first instance, just so that.
There are lots of different causes of sciatic pain, so pain down the back of the leg.
And I think that's really important as a starting point.
Is to work out what's causing that.
So go and see GP physio for that sort of expert assessment, and then sort treatment techniques.
They'll be able to guide you on with regards to sort of pain management strategies, exercise you might need to do, adaptations to your daily life.
And then that'll set you on the right road that potentially you can then do things at home by yourself, but get that expert opinion first of all.
Yeah, I agree with that.
And I think sometimes, the typical over-the-counter painkillers can be less effective at treating this sciatic pain because it's actually from irritation of the nerves.
The GP can sometimes support with prescriptions where appropriate as well.
Why might I have one hip joint that is so bad, it needs to be replaced, yet the other hip joint is in perfect condition?
Oh, so I might take that one.
So this is something that we see quite commonly.
And I think quite often as clinicians, it's equally as confusing for us as it is for our patients.
And sometimes, there's no real rhyme or reason to it.
Sometimes all of our joints are shaped slightly differently.
My hip joints will be shaped slightly differently with hip joints, for example.
And we also see within people that sometimes their joint called morphology, the structure of their joint, is slightly different on one side to the other.
And that in combination with their occupation or in combination with injury in the past or activity, can result in one side being affected, and the other side not being affected by arthritis.
But again, sometimes we just don't know sometimes.
Yeah.
Next question.
What might be causing inconsistent shoulder pain which comes and goes?
So we've spent most of today talking about osteoarthritis, and osteoarthritis does affect the shoulder joint as well, but we see it less commonly than we do in some of the other big joints, like the hips and knees.
Inconsistent variable shoulder pain, is much more likely to be related to what we call tendinopathy.
And this is something that we see affecting younger people, as well as older people for slightly different reasons.
And so tendinopathy is a problem.
The tendon is the part that's attaching the muscle onto the bone.
And so it transmits all of the force generated by the muscle, into the bone.
And it's constantly responding to that load on a day to day basis.
And sometimes that cycle become affected.
And the structure of the tendon changes a little bit.
And sometimes, that's due to what people call repetitive strain or overload.
And we see this in people, for example, with tennis elbow who type a lot or in the shoulder, it can be, we see it in decorators and window cleaners and people like that.
But also just people who maybe go out one day and start throwing a ball for the dog, or throw a stick for the dog, and that overload tendon and that generates pain.
And again, this is something that we can really successfully treat from a physiotherapy point of view.
Excellent, if I'm having muscle or joint pain, which is best, warm or cold?
That good old question.
So heat increases blood flow to the area.
Tends to be good for relaxing muscles.
It feels nice if you're feeling all sort of tense from your aches and pains, then a nice, hot bath, a hot water bottle or a heat pad that you sort stick to your skin, would tend to give symptom relief.
Cold tends to restrict the blood flow to the area.
So if somethings sort of hot and angry, if you put heat on it, it can sort of aggravate it.
Yeah, make it more throbby and- - Exactly, Yeah.
So you might want to sort of cool that one down with an ice pack.
If it's for generalized aches and pains, I'd say people have got their preference, they tend to.
I'd definitely be one for the warmth, but I've definitely had patients in the past who love putting an ice pack on their back.
They say it gives it relief.
Personally, I think it would make me more tense.
So individual preference for generalized aches and pains.
But if something's inflamed, I tend to go down this sort of cooling it route.
If something's more, a bit tense, I'd tend to go down the heat route.
So I think people probably then, depending on what their symptoms are and how they feel, use their intuition and it's the one that they feel will be most comfortable.
Try both of them at different times, or you may find if you like both, than one day put heat on.
Yeah, the next day put cold.
Excellent answer.
I've been told I have plantar fasciitis.
How do I best manage this slash curate?
Okay, so you're plantar fascia, the thick band of tissue that runs along the soul of your foot into your heel.
So most people who have problems in that area, complain of sharp pain after a period of rest.
So classically, as they get up and put their foot to the floor first thing in the morning, or if they've been sat for a long period of time, then when they go to stand up, they tend to hobble a little bit for the first few steps.
Things tend to then sort of warm up and relax.
And then they tend to their symptoms calm down a little bit.
But then if they do prolonged walking, prolonged running, prolonged standing, it tends to bring it on again.
So from a self-management perspective, there are things like, I tend to tell people to put small water bottle into a freezer and then roll your foot along it.
And you'll sort of.
It's of a double impact there that you've got the cold, but also the massage can tend to help.
Looking at your footwear is really important.
So good supportive footwear, calf stretches, plantar fascia stretches, are good to do.
Trainers are important.
If you are one that exercises, then I'd always recommend going to somewhere like a running shop.
You don't need to be a runner to go to a running shop, but the great thing there is to have a vast array of trainers.
You can go on the treadmill and try them out.
And different makes have just got different shapes to them as well.
And then even within one make, you've got different levels of control.
And when I talk about control, it's sometimes with plantar fascia problems, it can be that someone's foot over pronates.
It means that they roll a little bit too much inwards before they push off through their toe and propel forwards.
When you start getting into those rounds, I'd probably recommend you go and see a physio or a podiatrist.
They can have a good look at your foot posture, they may get you on a treadmill, or they may get you walking along what we call like, a gait analysis pattern, which looks at where you sort of wait there.
And from that, they may either give you trainer advice, where advice, or they may start to talk about insults or orthotics either over-the-counter or made ones.
Individually made ones.
They will also look at you higher up as well.
So we're all connected.
So what's going on in our knees.
What's going on in our hips as well, or likely have an effect on what's going on in our foot.
So they'll look at your muscle strength and your muscle length, all the way up, and see if there's any imbalances there that could be contributing.
Weight as well.
So the more weight you've got going through, can irritate your plantar fascia.
So think that's where exercise comes in, again.
It's like keeping that healthy weight.
So not too much weight is going through our bodies than needs to.
Okay, so a whole diverse range of things there.
Thank you, Emily.
What about tennis elbow, what can somebody do for that?
So tennis elbow, again, is a tendinopathy.
And by far the most common cause for tennis elbow that we see is this repetitive strain.
Well, it does affect quite a high percentage of high level tennis players, yeah.
But it's much more common just in people who spend a lot of time at a keyboard.
People who spend a lot of time using a mouse.
We see it really commonly in electricians, people who use screwdrivers and do a lot of gripping.
And this occurs because in order to be able to grip properly, our wrist needs to be cocked back a little bit.
That puts the muscles into the right position to be able to generate force.
You can't grip something if your wrists flex down like this.
And so if you are doing things that require gripping and require finger activity for long periods of the day, that can start to overload the tendon up at the top of the elbow here on the outside of the elbow where all of those muscles attached.
So as four muscles come up and attach into one single point here.
When people get tendinopathy, it's a change in the structure of the tendon.
And we know that with work and efforts and exercise, what we call loading-based exercise, we can change and remodel the structure of that tendon.
There's a lot of evidence about this looking at this process.
And so from a physiotherapy point of view, there are two core treatments for how we look at managing tendinopathy.
One is trying to modify the activity and what we call optimize the load.
We need to exercise it, but we need to tinker with things a little bit to try and make sure that we reduce the activities to aggravate things.
And the final question is, if there was one thing you would recommend people do to prevent problems developing with their muscles, tendons, and bones, and actually let's say also to treat any problems that they have that are musculoskeletal, what would it be?
It's regular exercise.
100% regular exercise.
I would also say regular exercise.
Emily, Joe, thank you so, so much for joining us.
And if you do want any more information about what you can access from a physiotherapy point of view or general advice on musculoskeletal care, do go to the Bupa website.
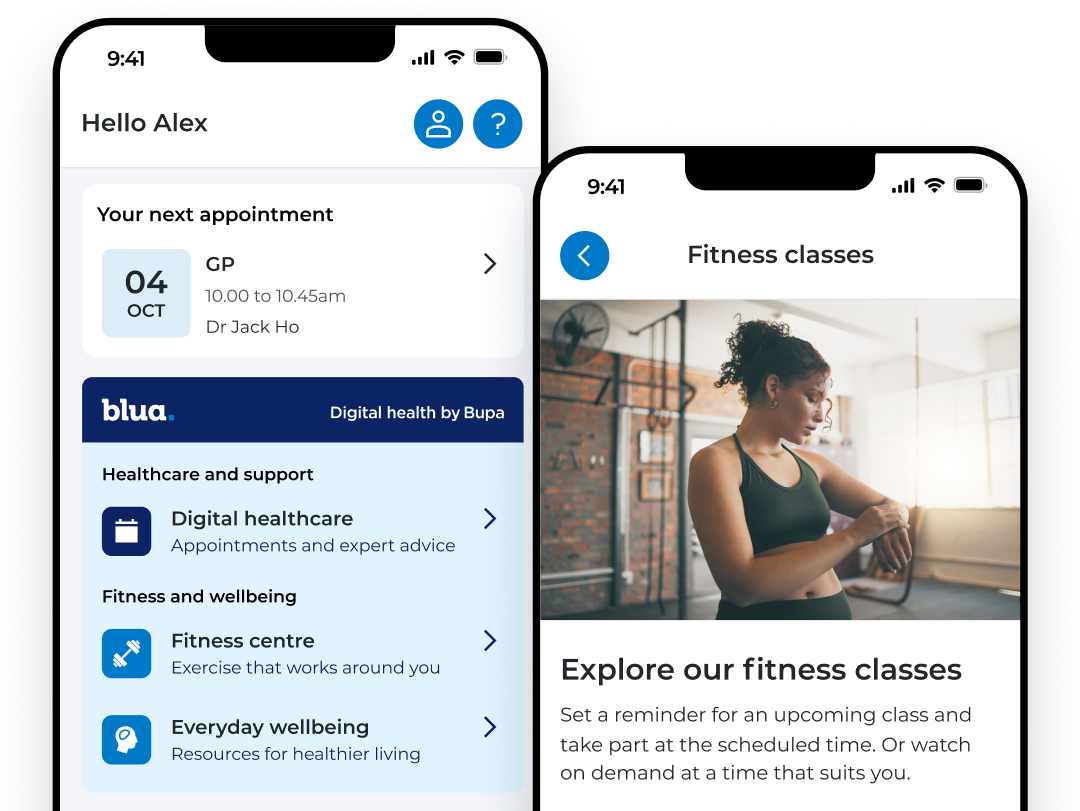
My Bupa, everything your people need in one place.
A digital account provides a convenient way for your people to get the support they need. Personalised to your employees level of cover, they can access a range of resources and services available to them.
To sign into the My Bupa app, your employees can use their existing Bupa account, or by creating a new digital account. It's the same app employees use for private health cover, dental insurance or health assessments.
Scan the QR code with your phone camera to download the app.
Further resources

Muscles, bones and joints hub
Browse for information and get expert advice. Find guidance on a range of conditions, treatments and explore how to prevent injuries whilst enjoying an active and healthy lifestyle.

Knee pain
Whether you have niggling pain, an existing knee condition or a new injury, we can help. Find expert advice on types of knee pain and conditions, as well as symptoms, causes and treatments.





