Women's health employee resources
Articles and resources to share with your team
Share information about various women’s health topics, including periods, endometriosis and the menopause.
How to keep an endometriosis diary
If you suspect you might have endometriosis, or have already been diagnosed, it could be helpful to keep a record of your symptoms.
What is the perimenopause?
Often when people talk about going through the menopause they’re actually talking about the perimenopause. Learn more in our helpful article.
Menopause HealthLine
Menopause can be tough. But you don’t have to go it alone. Chat to a menopause trained nurse about your symptoms and get the support you need to start feeling like you again.
The menstrual cycle - your questions answered
No two menstrual cycles are the same, and it can be hard to know what’s typical and what’s not. In this article we answer common questions about the menstrual cycle.
Questions about women's health? Just ask
Hear from Dr. Samantha Wild, Women's Health Lead for Bupa Clinics.
Transcript
What is stress?
Stress is a natural response to a pressure,
a demand that we are facing,
and it prompts us to address the challenges or the threats in a certain way
to be able to cope with those situations.
We find that we can get stressed in certain situations, for example,
when we are having to face something that we've never done before and this
prompts the body to react in a certain way,
to be able to allow us to cope with that effectively.
The body releases hormones such as adrenaline into the body,
and that is known as the fight or flight response.
Certain amounts of stress can be really positive, really beneficial for us,
and they can allow us to effectively tackle the things that we're having to do.
However, if we have stress over an extended period of time,
and it's excessive for us, that can have negative health impacts on us.
What are the symptoms of stress?
There are a range of symptoms that are commonly associated with stress,
and everyone is a little bit different. We can have symptoms such as low mood,
irritability, feeling worried all the time.
We can have trouble concentrating and attending to things.
We can have physical health implications, for example.
We can struggle to sleep. We can have problems with our eating. For example,
we are overeating or we don't have an appetite.
It might be that we're not motivated at all to do the things we're asked to do,
and sometimes we do see that we've got existing physical health conditions and
they can flare up, for example, skin conditions.
What is depression?
Everyone in life will experience low mood,
and that is a common feeling that we can have as we go through day-to-day life.
However,
clinical depression commonly is all about having a persistent low mood
where we have certain other symptoms that are impacting on our daily
functioning. For example, feelings of worthlessness, hopelessness,
low self-worth and low self-esteem.
There can be things to do with our negative thinking around things,
how we view ourselves, the world, others,
there's lots of different negative thinking going on.
It can be about how we can struggle with sleep,
so we can either be sleeping too much or not being able to get to sleep.
There can be problems with eating,
so we are struggling to have an appetite or we are eating a lot excessively,
almost comfort eating. We can also find that people can have suicidal thoughts,
thoughts of not wanting to be here. They can have self-harm thoughts as well.
So there's lots of different things that people can experience and people can go
from the mild with those symptoms right through to the severe,
and it can impair them in so many different ways.
It's a very difficult situation to be facing for people.
One thing I would mention is that people can present very differently with
depression,
so they can lean into certain types of symptoms and one person with depression
isn't going to experience it in exactly the same way as another person.
What are the main symptoms of depression?
The main symptoms of depression are a consistent low mood over a period of time.
We also can see problems with cognition,
so it can be struggled to concentrate, to attend to things.
When we process information,
it can be we're having quite a negative filter on things.
We are having lots of negative thoughts around lots of different
situations. Also about ourselves, very critical thinking.
We can have feelings of worthlessness, hopelessness low self-worth.
We can struggle to want to engage with people, so we can have social withdrawal.
We can struggle with our sleep.
So we can either sleep excessively or not be able to get off to sleep and have
insomnia. We can have problems with our physical health,
so it's almost,
we don't feel motivated and energized to be able to do anything as well.
So there's a range of different symptoms commonly associated with depression.
What is anxiety?
Anxiety is something that we all experience.
It's a very common feeling to feel anxious day to day for various reasons.
We can feel anxious in work. We can feel anxious at home for various things.
It can include triggers such as a situation, a circumstance,
an event. We need anxiety almost to be able to perform at times,
and it's actually very helpful for us. When we do have anxiety,
it feels like worry, uncertainty, fear,
sometimes unease, and it might be about a future event, for example,
we're having to face and deal with,
and the body responds to anxiety by triggering this fight or
flight response where it releases hormones such as adrenaline and cortisol into
our body to be able to cope with whatever we are having to deal with in its
milder forms. It's something that we see day to day in our life. As I say.
However,
when it becomes chronic and actually it stays with us and it impairs
our functioning in some way,
we could be starting to see the evidence of an anxiety disorder forming.
Is it normal for people to feel anxious?
It's a very normal feeling to feel anxiety and it can be for lots of different
reasons. So it might be that we are doing something outside of our comfort zone.
We are going to face a difficult situation.
It might be that we are experiencing something in life, which is very difficult.
For example,
we are out of work that is natural to feel that anxiety around those sorts of
things. So it's to totally normal. And when we have anxiety,
we've then got this body response to it,
which is the fight or flight response where the body triggers the hormones such
as adrenaline into our body for us to be able to address the things that we're
having to face and tackle them and address them in a helpful way and
to be successful in whatever we're doing. However,
when it impacts us to a point where we can't do things and it is a struggle
then to cope with whatever we're having to face,
it then starts to become maybe something outside of that and potentially a
clinical condition.
And there are different clinical conditions within the umbrella term of anxiety
disorders,
and it just depends on our certain set of symptoms as to what that anxiety
disorder may be.
What is burnout?
In our lifestyle, particularly our working life and our working environment,
and our approach to our working environment,
we can have a situation where our physical and mental health is affected,
and that can lead to something. What is known as burnout.
Burnout is when we have excessive work related pressure and demands
placed upon us, or we're placing upon ourselves,
which is not successfully managed,
and it ends up in a situation where we're feeling burnt out by work.
In the world that we're in at the moment, which is all about technology,
everyone's on the go all the time, and we're also working a lot from home.
We often have a situation where the boundaries have become blurred between our
work life and our home life,
and people are starting to feel the pressure of all of that and starting to feel
quite burnt out by the situation.
What are the symptoms of burnout?
There can be a range of different symptoms associated with the syndrome of
burnout that we commonly see.
And everyone's a little bit different in how they present and how burnout man
manifests within them. However,
some of the typical ones can be things such as cynicism and negativity
around the demands that we've got on us or the workplace, for example,
or the role we've got in work or our employer.
We can have just negative thinking in general. Our perception of things,
how we're turning up to things as well.
So it might be that we are quite confrontational when we're not.
Usually we can be quite irritable, have low mood.
We can be worrying a lot of the time,
or actually not really caring at the same time.
So a real sort of contradiction in how we're seeing things.
We really want to do well and we want to do a good job. Well, at the same time,
we don't care and we don't really want to do it either.
So it's a real contradiction at times within the person.
We can also see that the person can struggle with sleep.
They can struggle with eating,
whether they're not having an appetite or they're eating too much,
they can have problems with energy and motivation.
They can feel physically and emotionally and mentally absolutely drained and
exhausted by so many different things that they've got going on.
When they go home, they might be getting feedback that they're not a good dad,
they're not being a good partner,
and that is just really hard for the person because they're not having the best
time at work.
Then they're going home and maybe they're getting the feedback that they're not
doing a good job there, and so they don't have that sanctuary in either camp,
and so life becomes extremely difficult and then it just continues to
maintain itself and manifest into a syndrome known as burnout.
What is insomnia?
Insomnia is a term used to describe sleep problems.
And it can be us getting off to sleep. We are struggling with,
or it might be staying asleep.
And what happens is by the end of the night's sleep,
we haven't had enough rest and recuperation to face the next day.
And so what happens is we all know what that's like when we go into the next day
feeling tired and we've got lots of different things to do and to deal
with.
We find the day then very grueling and it then starts to impact on our physical
health and our mental health even more. Maybe our social relationships,
maybe our workplace.
There's lots of different impacts from not having a good night's sleep.
What types of mental health conditions are there?
There are many different conditions in mental health and just like physical
illnesses, we have conditions that go from the mild to the severe,
from the acute to the chronic and the complex.
We have conditions that are commonly associated with each other. For example,
common mental health conditions of anxiety and depression.
There can be a range of different conditions that you may
feel like you might be experiencing,
and it's really important if you do feel you've got any of these symptoms and
you've been looking at this yourself to contact someone and speak to them about
the situation and get the help you need as soon as you can do.
And I would also say that conditions look very different for different people.
So just because maybe your friend has had depression and it looks something like
this, doesn't mean to say that your depression is going to look the same.
So that is a really important thing to consider too.
Is it OK to be open about my mental health?
It is okay to be open about your mental health.
We're not saying it's easy to do so for certain people it can be a very
difficult conversation depending on the circumstances,
depending on the person and obviously what they're going through. However,
we start to then think about, well, who am I going to open up to?
And it's really important if you can do to open up to someone potentially in a
professional capacity like your line manager or the HR department,
or it might be a healthcare professional,
or if your employee's got an employee assistance program,
it might be speaking to a specialist there.
But we really encourage you to speak to someone as soon as you can do to get the
support you need. If that's in a professional sense,
that would be great because for example, in work,
they're looking after you there.
They would want to know about these sorts of things so that they can help you
and support you within that environment.
And then thinking about the other side of things,
which is your family and friends, and they are often the first port of call.
They are the people that we turn to for support. They love and care about us.
They would want you to be open with them and to share what's going on for you.
So if you do need some support and you're struggling right now,
please do reach out to someone as soon as possible. Don't delay.
Pick up the phone, send someone a text, book an appointment,
and get the help that you need.
How can I start talking about my mental health?
So it might be that you want to talk about your mental health with a colleague,
with a friend, with a family member.
And common things we often hear from people are that they feel worried about
having that conversation. They don't know where to start.
They wonder if it's going to change the relationship they've got with that
person.
They wonder about whether they're going to be judged because of it and
what people will think, will they be concerned about them? Will they be worried?
So there's lots of different things that go through someone's mind when they're
thinking about opening up and starting a conversation about their mental health.
And it might be that your preference is to speak to a healthcare professional in
the first instance,
or it might be that you want to actually speak to a family member or a friend.
And there's no right or wrong to that.
And it depends often on the circumstances and how you feel that conversation may
go. And what we would say is in terms of tips for going about that conversation,
it's things such as consider the mode of communication.
How are you going to share that information?
Is it going to be via a telephone call? Are you going to send a text?
Are you going to open up the conversation face to face?
Where is the place and time that you're going to do that?
Try and be as honest as you can be because that person needs to know what's
going on for you.
Thinking about you might give relevant examples of what's been going on.
You might give them some information about some of the things that you're having
to face and to experience.
It might be good to tell them about what helps and maybe if they're doing
something that doesn't help, maybe suggest that too.
And the last thing I'd probably say is if they're not a healthcare professional,
maybe give that person a break because it might have come like a bolt out of the
blue. They may not be expecting what you're about to say,
or it might be that they have thought it before and actually they want to ask
you lots of different questions about it.
And they may not necessarily navigate it exactly how you would want,
but revisit that conversation again with them when you're both ready to and
continue to have conversations about your mental health with whoever it is
around you that's closest to you,
because they're looking to help and support you as much as they can do.
I think someone is struggling, what should I do?
It may be the work colleague, they may be an employee,
they may be a family member or a friend, whoever they are.
It is important that you do speak to them and it's good to talk.
If we think about what that conversation looks like,
thinking about the fact that sadly,
there is still stigma in society around mental health in certain demographics,
cultures, families, generations.
And so whilst it might be okay for you to talk about your mental health,
that other person might not necessarily be that comfortable.
So just treading carefully,
seeing how they're responding to what you've got to ask and say is a really good
starting point. Then thinking about see it say it principle.
So if you see something and someone looks a certain way, mention it.
So it might be you seem like you've got the weight of the world on your
shoulders at the moment, and they can either say, well, yes,
actually that is the case this month. I've really felt like that.
Thank you for noticing that. Or they might say, well, no,
I felt like that last month, but now I don't feel so bad actually.
And they've put you straight and there's no harm done.
But you've gone out there and you've asked them something because that is what
you are sensing in how they're presenting to you.
And then thinking about that conversation about having open-ended questions
during the course of that conversation, that opens that person up.
It doesn't shut the conversation down,
and that person can go in any direction then with what they've got to say.
There's some tips,
but also just thinking about the actual conversation and making sure that person
is in a safe place. The environment is safe, it's private,
and they can spend some time with you and you can give them your full attention.
How can I talk to my children about mental health?
Giving our children and young people an opportunity to talk to us,
to open up and to share what they've got to say about their mental health and
wellbeing is some of the most important things we can do.
If we think about what that conversation might entail and how we feel about that
conversation.
The child is only looking for you to listen,
to hear them, to understand what they're going through.
You don't have to have all the answers.
You don't have to fix things for them because that is the pressure that we can
feel as parents and caregivers, that we've got to have all the answers.
No one has all the answers. No one gets it perfect every time.
The child will be reassured by you just listening to what they've got to say and
asking them questions about how they're getting on. So if we think about being,
rather than doing with a child, that is really, really,
really important to consider.
If we think about how we have that conversation with the child,
it can be sometimes helpful to just ask open questions about how their day's
been, how they've been getting on with things, how they feel about things,
and you are modelling to them how they should then connect with themselves and
how they should relate to themselves,
and also how they should regulate themselves.
If we think about then the conversation itself and when it can happen,
it might be that you're thinking, well, I don't know when the right time is.
I don't know what to say. I don't want to make things worse.
We really want you to think about maybe having the conversation when you're
doing an activity with the child,
because it can seem less intense for that child.
So it might be that you are making tea or you are driving along in the car and
there isn't that direct eye contact and that intensity then for that child to
then open up and talk to you about whatever they've got to say.
And then thinking about children and what it's like to be a child.
And we love them because they're so quirk and they say things that we don't
expect them to say a lot of the time,
and that's why they're so funny and endearing. So if you think about that,
expect the unexpected. When you ask questions, you get answers,
and we need to think about you having quite a neutral response to those answers
and not be over emotional if you can help it.
And so just giving that child that safe place to be able to speak to you and
disclose whatever it may be,
whatever they're thinking about and feeling that is really,
really important because that reinforces them to do that again with you.
And that is all the child is looking for you to do, is just to be hearing them,
listening to them, and understanding what they've got to say.
Why is there a stigma about mental health?
There is still a stigma in society around mental health.
I'm sad to say as a clinician, however,
it is improving and we're giving a lot of important attention to this subject
and it is work in progress and it is great to see. However,
there are still sections of society there are demographics,
there are generations,
there are cultures where there is still a stigma around speaking about mental
health and accessing mental health services.
And if we think about why stigma exists still, it is about, for example,
prejudice and misinformation and fear around the subject.
And what we need to do is continue our plight breakdown barriers for
people to be able to feel comfortable in sharing about their mental health as
much as they can do. Because if we don't do,
there's all sorts of staggering implications when we don't address our mental
health for us as individuals, the people around us and society.
And it leads to discrimination.
So let's break down the barriers and continue to do so together.
Is it important to look after my mental health?
It's very important to look after our mental health.
And if we think about that rather than anything associated with a mental health
condition for this question,
let's think about then what it looks like to just look after our mental health
day-to-day. And there's three things we typically would want you to think about.
The first one being our physiology.
So that is the foundation of everything really. So our diet,
our exercise regime, what we are drinking.
So are we drinking enough fluids? Are we using alcohol within reasonable limits?
Are we smoking? Are we using illicit drugs?
All of those things impact us as a person. Are we sleeping enough?
Are we getting rest?
These are the things that are the basis for us to exist and exist. Well,
and if you think about the link between physical and mental health,
it's really important that we get that basis right.
Then we think about the choices that we're making with our life.
And if we think about it, we've got 168 hours in the week,
how do you spend yours? And we really think about what that week looks like.
And have you got a good work-life balance?
How are you choosing to spend your time? Who are you choosing to spend it with?
Are you happy in the relationships you've got at the moment?
Are you happy with your finances?
Are you under stress in any way with regards to your social life,
your financial life, your physical health?
Are you doing things about them within your working week,
within the week itself?
And if you are struggling and you can't seem to get the time you need to be able
to go into these things that you want to enjoy. Let's look at that.
Let's take a massive step back and work out what you need to do about it.
Are you spending enough quality time with people?
Are you socially able to go out and enjoy yourself?
Are you taking regular holidays? Are you having breaks in work?
Things like that.
All of those things contribute to your wellbeing and your mental health,
and that is firmly about the choices. Life is a series of choices.
And let's look at the choices you're making.
And then the final thing is attitudes our beliefs, our perceptions,
how we see the world. It's often not the stressor,
it's the way we perceive the stressor. And if we think about,
are you looking at things in a negative sense or is it more of a positive lens?
We need to understand your attitudes, your beliefs,
your appraisals of things,
and whether they are negative or positive or balanced.
Are you able to have gratitude for the things you've got in your life or not?
Are you seeing things as a threat rather than an opportunity?
These are the things that we would expect you to consider when you are looking
to improve your mental health.
How can someone be a better listener?
Being a good listener is one of the most important skills we can have in life
because we are social animals and we are expected to listen to people so many
times throughout the course of even just one day.
And being effectively listened to is so therapeutic and so powerful for someone
emotionally. It has so much benefit for us as a person.
So in terms of mental health,
it is crucial that we are listened to and we listen to others too.
If we think about what it looks like to be a good listener and a better
listener, we think about things such as the way you go into the conversation.
So you are nonverbal body language. Are you having open posture?
So you look like you are the, to listen to what that person has got to say.
Are you giving them good eye contact so you are giving them your full and
undivided attention and they understand that.
Are you picking up on their nonverbal cues?
So you're sensing how that person seems to be in that conversation and going
with that sense.
Are you thinking about the next question you're going to ask or are you just
going to go with the flow? Because that is really what we're looking for.
We don't want you to be interrupting,
to be putting your opinions out there and coming up with solutions when that
person hasn't asked you that.
This is really crucial because people just need to share sometimes and just need
to be heard.
Are you then thinking about being curious about what that person's got to say?
Remaining calm,
remaining quite compassionate to whatever they've got to say and share with you
to make sure that they feel that you,
they're not being judged in that conversation. And finally,
just thinking about the way you handle it. When you finish that conversation,
potentially you might want to thank the person for sharing the information with
you because they may have never shared that before.
So it's really important that you recognize people's efforts if they do start to
speak to you about their mental health particularly.
Should we break the stigma around mental health?
It's really important to start breaking the stigma down because stigma is the
and exists,
and it means that people aren't connecting with what's going on for them as an
individual. They are then worsening potentially in their symptoms,
soldiering gone,
potentially impacting on people around them so that their life is indirectly
affected by this individual.
But also society is the implications of not addressing mental health
and having stigma around mental health in a society are staggering.
They're staggering on many different levels. On an individual level,
on a societal level, on a financial level, on an economic.
There's all sorts of implications for us not addressing stigma
within society. If we go back to the individual as well,
we think about someone who has had worsening symptoms over time.
That is then likely to mean that the,
they are going to have less effective treatment potentially for the mental
health, and also recovery is less likely to be successful as a result.
So there are implications for the person,
particularly if they feel stigmatized when they think about accessing
mental health services or even discussing it and approaching it with other
people.
Can mental health affect my body?
Mental health and physical health are not separate entities.
They are completely combined. They intertwine.
There's a complex interplay between our physical and mental health.
If we are mentally well,
we are likely to be physically well in a lot of ways and vice versa.
When we have mental health conditions,
we can commonly see physical health conditions and
symptoms associated with those conditions. For example, we can have headaches,
we can have digestive problems, we can have aches and pains.
There's all sorts of things that can happen when someone has a mental health
condition in regards to their physical health.
And it's really important that we have parity within looking after our
physical and mental health because both of them are equalling as important as
each other.
Am I the only one struggling with mental health?
So like physical health,
we can see good and bad days so we can feel physically fit and well.
But then for whatever reason, we don't want to go to the gym that day.
We don't want to go for a run. We have aches and pains.
We can't really explain them.
But then the next day we bounce back and we go back into the gym.
We go for that run. Our mental health is just the same. So on any given day,
we might feel a little bit low that day we might be a little,
little bit anxious. No one is a hundred percent happy all of the time.
That is a definite fact.
And sometimes our mental health can be affected by all sorts of different things
for different reasons in different people.
And it's never the same for any two people in society.
Everyone experiences it very differently and is unique.
What we've got to realize is when it comes to mental health and struggles,
it is common and mental health conditions are common actually.
So one in four of us in a year will experience mental ill health,
and if it is you who's struggling with your mental health right now,
please do reach out and speak to a professional about it because they are there
to help you and they will welcome you to do so.
Does talking about my mental health make me weak?
Talking about mental health is definitely not a sign of weakness.
It's actually quite the opposite. Everyone cries at times.
Everyone needs help and support. That is the reality of our lives.
We all experience anxiety at times,
low mood and stress that is common on a day-to-day basis with us
all. When we think about,
when we do share about our mental health and our feelings,
it's actually empowering. We grow as a person.
We can elicit change within ourselves. We get a sense of relief from it.
So there's lots of different benefits from sharing about how we feel.
And it's definitely not a weakness. It's more a strength because if we don't,
we're impacting ourselves. We're impacting people around us.
And so to have the strength and the courage to address your mental health,
it says so much about you as an individual. And what I would say is as well,
it's really beneficial in so many different ways.
And when we do start to share things about ourselves with others,
it actually humanizes us.
It shows a bit of vulnerability and actually people connect with us and bond
with us on many different levels. We're all facing a battle of some form.
It's just what that is.
So I'd really encourage you to speak about your mental health with a trusted
person. With a professional if you need to,
because it's really life transforming.
How can I tell if someone may be struggling?
It really can depend on the situation and the circumstances,
the person themselves, and obviously the problems that they're experiencing.
But in very broad terms, the person has changed in some ways,
in the way they operate, the way they behave,
the way they are speaking to you, their outlook on things, the habits.
There's something that has changed in them as a person,
and you've noticed it as someone close to them.
And it can be things such as you've invited them to come to events and they're
starting to decline them, and that is not typical of them.
Or it might be that they are turning up to events and they're being,
for example, confrontational,
or they're not showing any emotional response to things and they seem quite numb
and detached. Or it might be quite the opposite,
and they're becoming quite tearful for no apparent reason.
But you've noticed a shift in them. You've noticed changes within them,
and I would encourage you to keep asking them how they're doing,
because it might be on one occasion they don't want to speak about it,
but the next time you ask them,
they do start to open up and tell you what's going on for them.
How can mental health affect someone's life?
There are so many ways in which mental health problems can affect someone's
life.
Their life is almost all about mental health that is
intrinsic to every single last thing that they do in their life.
It is about the way they perceive things, how they problem solve,
how they handle stress, how they feel inside themselves,
how they deal with others. There's so many things,
how they manage their finances,
that the implications of mental health are huge on a person.
And what we find is when one thing happens to them, another thing happens,
and things start to compound and manifest.
And the person can then be impacted by multiple,
potentially mental health problems, at least more than one.
And that can be very, very debilitating and difficult,
and has a significant effect on their functioning and reaching their potential
and their quality of life struggles significantly.
What may be negatively impacting my mental health?
Well, you are the expert on you. And when we look at this, we think about, well,
okay, when was the last time you felt, okay, well good in yourself?
And let's think about what was going on around that time.
Who did you have around you? What were you doing? Were you in work?
What was the work environment? How did you present in work?
How did you feel in yourself? How did you seem turn up to things?
And then what we start to do is think about, well,
what's happened since that time when you felt well, when you felt good,
when you felt better? And then let's think about what may have happened.
So has there been changes in finances in your working life,
in your personal life with the people around you?
Has something changed within you? For example,
have you got now a physical health complaint, for example?
There can be lots of different things that have happened along the way to lead
you to this point where you might be feeling that you might be struggling in
some way or something might be negatively impacting on your mental health.
And then we think about then breaking it down and really understanding
what might have gone on.
And if you are doing that and you can't seem to work out what might be the
factors at play and you're struggling to put things together and understand it
in your own mind, reach out to a healthcare professional,
reach out to someone and speak to them and get a fresh pair of eyes on the
subject and they will help you to look at what's been going on and guide you to
the right source of support.
What can I do to improve my mental health?
To stay mentally fit and well, or what we could use as the term mental hygiene.
We think about then what that really looks like in reality.
And I guess it's a bit like dental hygiene. We clean our teeth once,
twice a day. We don't really think too much about it,
but we've got to apply the same principles to our mental health.
Why do you do that every day with your teeth?
You do it because you don't want your teeth to become bad.
The same principles apply to your mental health or your mental hygiene.
So thinking about that, what does that look like on a day-to-day basis?
We've got to think about our physical health because that has a lot of interplay
with our mental health. So we need to keep physically well, for example,
our exercise routine, our sleep, our diet,
things like that are really important for our mental wellbeing.
And then we keep it almost hygienic within our mind. We've got a good mindset.
We've got a growth mindset every day.
We are keeping fit and well within our own mental capacity.
And then we think about what else do we need to do?
We need to have people around us that are good for us.
We need to enjoy our work. We need to have purpose in our life.
Things like this are really important. And also things such as,
are we having a good work life balance?
Are we getting enough play in association with how much we work?
So thinking about that, it's about booking holidays, getting out there,
having hobbies, having interests, and enjoying them as well.
Is it possible to prevent poor mental health?
In most cases, it is possible to prevent poor mental health.
We've got to think about things such as how we understand ourselves.
Self-awareness is so important as an initial step.
Do we understand how we operate, how we tick, what affects us? What helps,
what doesn't help? What are our signs of stress?
These are the things that we should understand about ourselves as we go through
life. And then we start to think about, well, how do we invest in ourselves?
How do we look after ourselves? How do we prioritize ourselves first?
Because before we do that, before we do anything with anyone else,
we've got to do that. That is really, really important.
Thinking about then about the activities that we engage in,
how we choose to live our life,
what choices are we making with regards to the people we're spending time with,
our relationships, our wellness? More broadly,
are we looking after our physical health, our financial health?
There's all sorts of things we can do to prevent poor mental health.
I'm busy, how do I engage with wellbeing services?
Nearly everyone's life is extremely busy.
But it's essential that we engage with services that are there designed to help
us with our mental health and wellbeing. And within any lifestyle,
any schedule, any diary,
we can accommodate one of those services or one of those resources or one of
those facilities. Let's think about what is open to us. We've got things online,
digital, we've got telephone-based services,
we've got appointments and consultations that are face-to-face.
There's so many different things.
There's something for everyone with regards to our mental health and wellbeing
and keeping it in check. And then we've got to think about, well,
what is the first step? And often the first step is the hardest step,
which is planning even to just access that first service or that
resource page. So let's think about how we do that.
We've got to form healthy habits within our life,
and we've got to prioritize our own wellbeing.
And so it's really important that we take stock,
we look at our diary and we work out where can we fit this in?
And we might need to say no to things,
to be able to say yes to things that we need to.
And that is the reality of this.
We've got to invest in ourselves to sustain our mental health and wellbeing.
Is it OK to use mental health support services?
There is still stigma in society around mental health services and people have
sometimes fears around, you know,
what it's going to be like to go through the process of speaking to someone
about their mental health. There can be fear, there can be fear of judgement,
there can be fear of change of what they're going to discover.
There can be the male traditional stereotype of, this is weak.
If I go and access this help. The pride stops them from doing that.
It can be that someone is wondering how it will impact them.
For example, from a career perspective,
there's lots of different things that go on in a person's mind,
and there are also opinions such as, you know,
are mental cell health services going to actually help me? Are they effective?
What do they do to help me in these sorts of situations?
There's lots of questions being asked of us as clinicians,
as people start to access mental health services.
Is it okay to ask access mental health services? What is it going to be like?
And people when they have access services say,
why didn't I do this 10 years ago, 20 years ago, 40 years ago?
And I have that as a clinician on a day-to-day basis. So what I would say is,
if you are struggling, reach out. Pick up the phone,
contact someone today, book the appointment.
We are here as mental health clinicians to support you.
We care deeply about you and we want to get you fit and well,
and to have that quality of life back that you deserve.
Can you have multiple mental health conditions?
Like physical illnesses,
people can have more than one mental health condition at a time,
and this is known as comorbidity.
And we can typically see that certain common mental health conditions can come
hand in hand, for example, anxiety and depression. And so yes,
people can experience more than one mental health condition at a time.
What causes mental health conditions?
There are so many things that affect mental health and therefore can cause or
can be associated with mental health conditions.
The list is pretty endless really. But if we just think about some of them,
they are things such as our genetics, our personality,
our life experiences,
our social and economic status things that happen to us
during the course of our life.
There's lots of different things that can impact on us as a person and can
lead and cause mental health conditions.
Who can experience mental ill health?
Mental health cuts across every sector of society.
It does not discriminate.
And we find that we can all experience mental ill health at times,
and it might be that we are certainly more likely to experience certain common
mental health conditions such as anxiety and depression.
Some of us are more vulnerable to mental health than others for different
reasons. It could be our genetics, it could be our life experiences.
It could be our physical health problems that we may be facing or our
upbringing.
There's lots of different reasons why we might be more vulnerable than the next
person to experiencing mental health problems,
but definitely we can all experience them.
How common is it to experience mental ill health?
So it is common to experience mental ill health, and in the uk,
one in four of us will experience a mental health problem in the year.
And if we think about then within England,
one in six of us will experience a common mental health condition such as
anxiety and depression in any given week.
So if you think about a typical family household,
we're either indirectly or directly going to be affected by mental health
problems on a weekly basis.
How can I keep my employees mentally healthy?
As a manager, we've got a key role.
We are often the first port of call for our employees,
so it's really important that we consider how we keep our team mentally healthy.
And if we think about that,
it could be things such as creating a sense of cohesion, of connection,
of belonging.
It might be about reaching out to people and having a sort of a non-problem
talk conversation. So it's not about work,
it's not about anything to do with their role within that working environment.
It's actually about them as a person, as an individual.
And now with this remote working,
it's harder and harder to be able to connect to people on that personal level.
So just reaching out and just starting the first part of the conversation,
maybe in a one-to-one by talking about them and how they're getting on and what
they've been up to,
and just sharing something about yourself as well that can really start to
create that sense of connection with your employee.
Then thinking about the wider team and thinking about raising awareness of
particular subjects and issues and then people get more used to and more
comfortable in talking about ensuring experiences and things that are going
on for them and really connecting on different subjects.
Thinking then about how you practice what you preach.
So if you are asking them to clock off and make sure they take breaks and make
sure the booking holidays, make sure that you are modelling the same things.
Creating that sense of psychological safety so that people can turn up and show
up to work however they would like to in the sense of they are them,
be you wherever you are in your work because that is really important that
we're not excluding people.
We are inclusive as an employer and as a manager,
you recognize whatever they're bringing to the party and you value them
dearly.
Thinking about then how you communicate with them and thinking about making sure
that you've asked them how they're doing, making sure that you check in,
you're detecting if there's any issues, say what you see.
So if you do notice something, a change in someone,
make sure that you put it to them and see if you can help them to understand
what's been going on for them.
And maybe you need to make some adjustments for them.
But having that open conversation and having that safe place for them to be able
to do that with you as their manager is going to be really beneficial for their
mental wellbeing and work.
Who are you?
Hello, I'm Dr.
Naomi Humber and I'm a clinical psychologist and also head of Mental wellbeing
at Bupa Health Clinics.
Please feel free to ask me anything you want about your mental health,
how to support others with their mental health,
and how to access some of bupa's mental health services.
How can Bupa support me with my mental health?
Bupa,
we've got a range of different resources and services to support you with your
mental health and wellbeing needs.
You can call our mental health specialist support team and they will provide you
with information about what your policy covers.
You can also look at if you have access to an employee assistance program,
and if you're unsure about that,
please do speak to your HR team and they will allow you to understand whether
that is something you have available. And finally,
we have lots of information on our Bupa website too.
How do I access the Bupa mental health services?
If you have a GP referral,
please do feel free to contact the Mental Health Specialist Support Team and
they will guide you through that process to accessing treatment.
If you don't have a GP referral letter,
please do contact the Mental Health Specialist support team and they will talk
you through what is available on your policy.
You may have access to an employee assistance program or access to digital gp,
however,
please do refer to your certificate about those things or speak to your HR
team who will be able to help you and guide you through that process.
What types of mental health treatment are there?
In the main treatments available for mental health conditions are either
medication or a talking therapy or a combination of both.
And people will find that they have a preference for one or the other usually.
And we find that sometimes one treatment is more effective than another for
various reasons, and it's not necessarily about the treatment.
It can be about the person's circumstances, their particular preferences,
what's going on for them at that particular point in time,
or the complexity of different issues and symptoms that they are experiencing.
Do I have a choice of mental health professionals?
You absolutely do have a choice of mental health professionals at Bupa.
You can access our consultant and facilities, find a website,
and there you'll have access to all our Bupa approved clinicians.
And you can have a look there yourself if you'd like to,
or you can contact our Bupa mental health specialist support team,
and they will be able to guide you through that process with an informed
understanding of the right clinician,
with the right training and the credentials that are required for you to get the
right treatment. And also look at your preference.
It might be a personality preference, it might be something to do with,
for example, a gender of the therapist that you are looking for.
And also make sure that that consultant or therapist is covered on your policy.
What if I don't like the therapist I have chosen?
As a clinician and at Bupa, we understand that that can happen on occasion,
and we want you to have the right person for you for that really important
mental health journey.
So we'd encourage you to contact the Bupa mental health Specialist support team,
and they will be able to guide you through that process and make sure that you
have the right person for you,
whether that's the personality fit or there's another preference that you're
looking for,
and they will ensure as well that that person is covered on your policy.
Who can I talk to about my mental health?
At Bupa,
we have a range of different professionals and services available for you to
help with your mental health.
You can call our mental health specialist support team at Bupa and there are a
range of advisors for you to speak to about what is covered on your mental
health policy and also a team of mental health nurses too.
You may have access to an employee assistance program at Bupa,
and I would encourage you to speak to your HR if you're unsure and that goes for
digital GP two,
you may have access to a digital GP as part of your policy. Again,
if you're unsure,
please do contact your HR team and they will be able to guide you.
How are mental health conditions diagnosed?
Mental health conditions are typically diagnosed by a doctor,
and the process is usually something where we talk through the person's
presenting issues and their symptoms, the history of the complaint.
We look at the person's circumstances and needs and the severity of the
situation and how much the symptoms are impacting on their functioning to be
able to make that diagnosis.
Will I see my therapist online or in-person?
Most consultants and therapists these days offer both remote and face-to-face
consultations.
It may be because of the type of mental health condition you have and the needs
associated with that.
The consultant or therapist recommends that you have a face-to-face
consultation. However,
I do encourage you to speak to the clinician about this and they will be able to
guide you on what is best for you.
Will I have to pay towards my treatment?
If you have excess on your policy,
you may have to contribute towards your treatment costs. However,
if you call the mental health specialist support team,
they will be able to explain those costs to you before you go on to any
treatment.
How long do mental health therapy sessions last?
A therapy session typically lasts between.
50 And 60 minutes.
I am scared of having therapy sessions. Any tips?
I think it's a really normal and natural thing to be quite scared about going
into a therapy session. It's the unknown.
It's something maybe you've never done before. It's a stranger,
and you're going to be talking about some very personal things potentially,
and so we understand that as clinicians. It's a big,
brave thing that you're doing, and it's a courageous first step.
Thinking about other appointments that you've been to in your life and how they
went, and typically they've all gone very well and the person who's led that
appointment has guided you through that process.
The same will happen with a mental health therapy session,
particularly an initial session.
It might be that you want to prepare for that session and make some notes before
you go in thinking about what you'd like to convey and what you'd like to say in
that initial session. If you don't want to prepare, that's absolutely fine too.
It might be worthwhile telling your therapist on that initial session how you're
feeling and they will be able to reassure you and support you through that
initial conversation.
Will my manager know if I use my Bupa policy?
No, any of the support you receive through Bupa will not be shared with your
employer and your treatment will remain confidential.
Can I refer employees for Bupa support?
You can signpost your employee to Bupa as a support tool,
and they can come to us and get guidance, advice, and support.
You can also signpost them to the mental health specialist support team and you
may have access to an employee assistance program for your employee.
And if you are unsure about this,
please do contact your HR team and they will be able to help you.
Do I need a GP referral in order to get treatment?
You might not need a GP referral to get access to treatment.
You may have access to an employee assistance program via your employer or
access to digital gp. However, if you are unsure of this,
please do check it with your HR team as it will be subject to your policy.
You may want to contact the Bupa mental health specialist support team who may
be able to provide you with access to a pathway called the Direct Access
Service, where you can get a mental health assessment.
How do I find a therapist?
You can call our mental health specialist support team and they will be there to
guide you through that choice of clinicians who are suitable and appropriate for
your needs, and also to ensure that they are covered on your policy.
And you can also go onto the consultant and facilities finder to look at those
choices.
I have a GP referral. What do I do?
If you call the mental health specialist support team,
they may be able to guide you to an appropriate specialist and also ensure that
that person is covered on your policy and discuss next steps.
Does it take long to treat MH conditions?
The intensity and the duration of treatment for mental health conditions vary,
and it will depend on the level and the type of need for that person and the
symptoms that they are experiencing.
What we often find is that the person and their situation, their circumstance,
what's going on for them at the time of treatment will all play a part in how
effective that treatment is,
and so treatment might be extended because of those reasons. We do align,
though,
with nice guidance and regulation to ensure that we approach treatment in the
right way and we give people the treatment as the evidence base does suggest.
Can I access Bupa services if I leave my role?
Speak to us and we can discuss options with you.
That might include continuation of your insurance policy once your employment
ends. We can also discuss potentially pay-as-you-go services at Bupa,
and also anyone is able to access the health content on our website
and that is free and available for everyone.
Can I find a therapist myself?
You can find a therapist yourself,
and we do encourage you to look on the Bupa Consultant and Facilities Finder
website to ensure that they are Bupa recognized. However,
what we really recommend is that you contact our mental health specialist
support team who can guide you through that process.
Look at clinicians who have the right credentials, qualification,
and training to be able to support you and also ensure that that person is
covered on your policy.
Can Bupa support me without health insurance?
We may be able to support you on a pay as you go basis with your mental health
needs, and you can also access content through our website where there's lots of
information that is free and available to everyone.
My child is struggling. Can Bupa support them?
Bupa may be able to support your child with their mental health if they are
covered on your policy.
And if you call our mental health specialist support team,
they may be able to guide your child to an appropriate specialist depending on
their needs and situation.
You can also contact our family mental health line and speak to a team of nurses
who are there to guide and support you in regards to whatever problems or
difficulties or challenges your child is facing.
If you have access to the Employer Assistance Program at Bupa
by your employer,
they will be able to support your child if your child is 16 or 17 years old
themselves. And if not,
you can speak to your employee assistance program about your child too and get
support for yourself should you need to as a parent or caregiver.
Where can I find information about mental health?
There's lots of information out there from really trusted websites and
resources. I would encourage you to go to the Bupa website.
There is the JA platform. There is the N h S website,
and there's also charities such as mine that have lots of different information
that is free and available to everyone.
Guidance and support from our experts
Our experts are joined by some familiar faces as they discuss signs and symptoms as well as tackling some well known misconceptions.
Inside Health:
How to check for breast cancer
Self examination is the key to detecting breast cancer early.
In this Inside Health episode, Dr Zoe Williams shows us how to
carry out a breast cancer self check. It’s important to do these
checks around once a month.
Here's a quick demo of one way you can self-check so starting off by looking with your top off.
Looking from the front.
Different hand positions, hands behind your head and also pushing onto your hips.
And then do the same from one side.
And the same from the other side.
And next, you're going to feel.
So start with one breast.
Use the pads of the fingers and use whatever technique works for you.
This is the spiral technique.
So as long as you feel every single area of the breast.
Doesn’t matter how you do it.
Some people use the lawnmower technique.
Some people imagine the breast is in four quarters and feel one quarter at a time.
To complete the examination, you can also feel the front of the chest wall all the way up to the collarbone.
It doesn't matter which hand you use, whatever's easiest, and then also feel all of the areas in the armpit and once you’ve done one side, the same on the other side, and then you're done.
The Doctor Will Hear You Now Podcast:
Endometriosis
Endometriosis is as common as asthma, and yet an incredibly huge number of people haven t heard of the condition. Dr. Zoe is joined by TV broadcaster Michelle Ackerley to hear her journey to diagnosis and beyond.
(gentle intro music) Every topic that this podcast series covers has a lot of thought put into the why.
So why shine a spotlight on this particular topic?
And I think the topic we're gonna talk about today, when thinking about health conditions that have a lot of misunderstanding and misinformation and stigma, this one has to be very close to the top of that list.
Today we're gonna talk about endometriosis, and I'm so grateful to our lovely guest, Michelle Ackerley, who is here to talk to us about her experience of living with endometriosis.
So Michelle is a very successful TV presenter, she's presented "World's Strongest Man", "The One Show" and "Crime Watch.
" But today, so grateful for you to coming on, Michelle.
We've met once before, haven't we?
We have.
But I feel like I should've met you more.
I feel like we have so much in common.
Yeah, totally.
But the question we always start off with, and the question I'd like to ask you, first of all, is, what is the one thing you should never say to somebody who's living with endometriosis?
For me, that would be comparing it to just a normal stomach ache and dismissing that pain.
So when I was in real pain with endometriosis, sometimes people would say, "Oh yeah, tummy aches, they're really bad, aren't they?
Put a hot water bottle on it.
" And I would just feel like my experience with the condition was really dismissed and comparable to other forms of pain, which weren't as bad.
That's how I felt.
Well, I guess that that's one of the real difficulties of understanding somebody else's experience of pain is that you just don't, you don't know how severe it is.
You don't know how it feels, the nature of it, and you don't know how it impacts on their life.
Yeah.
So you kind of, I guess people are assuming therefore, that the pain you're experiencing is not what you're actually experiencing.
And that's totally true, 'cause when I first started having the symptoms, I didn't really know what was going on.
So, you know, as a young woman, I'm thinking, well, maybe this is just what stomach aches are like, or, you know, bad period pains are like, this is normal, and it's only when you've been through that process and you can reflect on it, that you understand a bit more about not only yourself, but about a condition, how it makes you feel physically, how it makes you feel mentally, but also how what other people say to you impacts within that process as well, you know?
Okay, so that's really helpful to know.
Something for all of us to bear in mind, you know, never make assumptions about somebody else's experience of any type of pain.
But I think it's particularly true when we're talking about endometriosis.
I wanna ask you, when did you first hear the word endometriosis, and did you understand what it was immediately?
And also, I'm gonna put you on the spot and ask you to define what endometriosis is.
I thought you were gonna ask me to spell it then, Zoe.
I was thinking, oh, my God, I'm gonna be out.
I wouldn't do that.
Straight away, I get it wrong every time.
But the first time I actually came across endometriosis was through my mum.
Right.
She ended up having to have a full hysterectomy because her endometriosis was so bad.
So it was kind of on the radar for me through her experiences.
I kind of followed in her footsteps in a weird way in terms of having really bad period pains, very heavy pain, very heavy period pains, and when she was going through that kinda stage, she went to her gynaecologist and was having, you know, various checkups and then, you know, got told that she had this condition, endometriosis, and went for a laparoscopy.
Another word that I can't spell very well.
And was going through this kinda thing.
So I'd always, I'd heard about it through her.
And then when, you know, I started growing up and I was having what I thought was similar kind of experiences to my mum, I would say to her, you know, "I'm in real pain here.
" You know, "The stomach aches are really bad.
" And she was the one that actually first said, "You know what?
We should get you checked out properly because this could be something that you're going through.
" If it hadn't been for that, Yeah.
I think it would've taken a lot longer.
Yeah.
As well, you know?
Yeah.
Well, I guess in some ways you did have a bit of a head start in that your mum, of all people, you know, somebody really close to you had been through it, so therefore there was some level of understanding and someone to say, "Right, we need to get this checked out.
" Yeah.
"Early on.
" Yeah, exactly.
And, you know, trying to explain exactly what it is from a medical point of view, it still kind of baffles me.
It still blows my mind a bit in terms of what is actually happening.
Yeah.
And I think growing up, my focus was just trying to stop it from happening rather than really drilling down and understanding exactly what is happening.
Yeah.
And in my mind visually, I liken it to like having some kind of lining growing on the womb.
And when I had like laser treatment, they were trying to get rid of that, they were trying Yeah.
To get rid of, there's some kind of lining that's there.
Yeah.
Does that make any sense?
Yeah, so, you know, I'm not really here, I'm here to listen to you, but I think it is with this one important for people listening to understand what endometriosis is.
So the lining of the womb in a woman is the endometrium, and it's made up of endometrial tissue, and it's very special tissue because it responds to our hormones and, you know, with our monthly cycle.
If we don't get pregnant in a monthly cycle, then that tissue sheds and we bleed.
So endometriosis is when you have that endometrial tissue in somewhere else other than the lining of the womb.
So most commonly it's around the other pelvic organs.
So in the peritoneum, which is the tissue that lines the pelvis, but strictly speaking, it can be just about everywhere.
So it can be in the bowel, it can be on the bladder, it can be in the ovaries, it can be in the muscle of the actual womb itself.
And it can also be, you know, the rare case we always hear about in medical school, which I've never seen a case of, but it can be in the lungs Really?
So people can actually cough up blood, so it is possible to have, Gosh, I've never heard Endometriosis of the lung Of that before.
So that's what it is, which is why you can imagine that if that tissue is responding to your hormones in the same way as the lining of the womb does, if you are having, say you're having regular periods once a month, once a month that tissue will bleed and that blood will cause inflammation and can cause scarring and damage.
Yeah.
So what age were you when you first got the diagnosis, and what was the route to that diagnosis for you?
'Cause we, Yeah.
You know, we hear this really concerning statistic, which is one of the reasons I wanted to discuss this topic, that it takes on average eight years for somebody to get the diagnosis of endometriosis.
Which is so scary really, when you think back, I feel kind of lucky in a way because I think it probably would've taken a lot longer if it hadn't been through, you know, my mum's experience and her being quite pushy with me at the time and saying, "We need to get this checked out, Michelle.
" Yeah.
It was around my early twenties, so probably 23, 24.
But in the lead up to that, you know, every month when I was having my periods, I'd be in so much pain, and as I say, bleeding so heavily and nothing would work.
You know, you pop two paracetamol.
It was just like eating sweets, it didn't do anything.
Yeah.
It didn't literally didn't do anything.
And I'd go back and forth to the doctors and, you know, have conversations and try different forms of the pill, anything that might kind of help with that experience and nothing did.
And it was almost, as my mum's situation progressed, and it kind of coincided with her having a full hysterectomy, whilst my kind of pain was getting worse, that it kind of reached that point of I actually went to her gynaecologist, and he was the one that diagnosed me with endometriosis.
Right.
And then it was the start of, okay, well, how does this journey unfold, you know?
And for me, it was just a case of wanting anything that was going to stop that pain, Yeah.
To be able to enjoy a normal life.
You know, I'd just started work experience at the BBC, and I was going in every day.
And, you know what it's like.
You're trying to put a face on, you're trying Yeah.
To show the best part of you.
And I'd be sat at my desk just trying to psych myself up, and trying to ignore this part of my physical body that was, you know, just not functioning, you know, and carry on with my everyday life.
So when I eventually got that diagnosis, I felt better for it.
But to be completely honest with you, I actually felt really scared as well because I could see up front Yeah.
What my mum Well, that's it.
Had been going through.
You know?
Yeah so, on the one hand, you had this, I guess, you had an inkling as to what it was, and you had your mum there to inform you, but also, you were seeing your mum, what she was going through.
Yeah.
She'd already had the laparoscopy.
So that's keyhole surgery, which is actually what's required for a definitive diagnosis of endometriosis.
And then she's gonna go ahead and have a hysterectomy.
So had you had a laparoscopy, Yeah.
This time as well?
Yeah, I'd had the laparoscopy, and I remember the first time I had that, you know, 'cause the little thing down your belly button.
So it was a general anaesthetic, isn't it?
Yeah.
It's an operation where they have to put you to sleep and they usually do two, sometimes three, small cuts where they can put tubes in and have a look with cameras- That's it.
To see if you've got endometriosis there.
And I remember waking up and kind of, obviously, they put the stitches in and seeing, you know, these little stitches in my belly button and thinking, okay, so.
Even at the time I was like, well, "Is this gonna make me better?
" Do you know what I mean?
Is this something that's actually gonna sort it out?
Maybe this is a step of the process where I'll start to feel better now.
But obviously, upon reflection that, you know, that wasn't the case at all.
At this stage, obviously I knew then what it was, but it was very much a long process after that to start feeling better and start, well, not necessarily better, but it being managed.
So I actually went on Zoladex injections.
So Zoladex injections sort of, they kind of block the female hormones somewhat because they are contributing to the issue of endometriosis, but tend to have some nasty side effects.
And that was the thing, Zoe, you know, on the one hand, I was happy that something had been given to me to stop the pain, but then all these other side effects kept coming through.
It almost, you know, someone likened it to you almost going through like a mini menopause at a young age.
And the symptoms that I was getting, whilst I was, you know, going to work every day, hot flushes, really bad hot flushes.
My skin completely, completely changed, getting really bad breakouts, and also just having really bad anxiety because I could feel things were changing in my body.
And whilst I wasn't getting the same kind of pain, I was getting all these different symptoms.
And as a young woman, you're trying to, you manage that.
And I feel like now if it was to happen, the added thing that I would be thinking about is am I ever gonna be able to have kids?
You know, I think in my early 20s, I wasn't thinking about that as much as being in my late 30s now.
It was more just prevent the pain, prevent the pain, prevent the pain.
And now it's good the pain's prevented, but how much has this actually impacted on my body overall?
And what does this mean?
Especially, you know, as I keep coming back to you, my mum, you can see a woman that has had to have a full hysterectomy.
You know, she'd had myself and my brother Jonathan at the time.
So she actually had had children, even dealing with a condition.
But yeah, there was a lot going on and sense still does go on within my mind of how it impacts you in the short term, but also in the long term.
And really feeling like there was no one to speak to about it in the real world, outside those gynaecologist appointments or thankfully to my mum.
Whilst something that actually really surprised me, whilst I was researching for this conversation, I knew endometriosis was common, but I didn't realise that it's almost as common as asthma in women.
One in 10- That is crazy.
Women in fact, if you were to take a female population, adult population at any one time, about one in 10 of them would be suffering from back pain.
And one in 10 are suffering from endometriosis.
In clinic, I see patients about back pain all the time.
My friends are always telling me they've got back pain, yet endometriosis is just as common.
But yet you felt as I know, many other women do, you felt alone and like there was nobody really you could talk to about it.
And this is what's extraordinary.
'cause me and one of my friends, I'd spoken about endometriosis recently, probably like, you know, one of the first time I'd spoken about it a bit more openly, and she happened to watch it, and she messaged me and she said, "Michelle, I never knew you had endometriosis.
I've got it too.
" And she's like, "Isn't this crazy?
" We've known each other for 15 years, and we've never once spoken about it.
And we were both actually really disappointed in ourselves in the sense that we could have actually had these chats- you could've supported each other Supported each other.
Yeah, let's go back a little bit, and I think I want to, as somebody who has not had this condition, I've had some painful periods, but this is something that's on a completely different level.
And also, you know, in some people it affects them during the time of their period, but some people have pain all of the time with endometriosis because of some of the sort of scarring and inflammation and damage it can cause.
What was it like for, I mean it might still be, we haven't got there yet, but talk us through, I guess, how you would feel when you, at whatever given time of the month, your symptoms might start, what you would think and how it would feel and just share with us the experience.
It's almost like a dark cloud, really.
Because once I knew what it was, and, you know, you can define what's there, it's almost having like this foreign thing in your body that's changing everything about you.
So I'd constantly have this dragging down feeling and stomach pain.
But, you know, sometimes when you think of stomach pain, you think it's an isolated pain.
You could put a hot water bottle on, put your feet up, relax and it might try and help the pain.
Bit like what happens with normal period pain, yeah.
Yeah, exactly.
But this, for me, it didn't feel like an isolated pain.
It started in the stomach, but it felt like it just was all encompassing.
It was everywhere.
I couldn't get away from it.
I couldn't escape from it.
And it was almost like started in the, you know, the stomach area.
But it's journeying all the way up to my head in terms of affecting how I feel mentally, just feeling really low because you're not feeling yourself.
Yeah.
Feeling incredibly anxious because I didn't talk about it enough, you know?
If I was at work in this new job, trying to prove myself, but at the same time, trying to disguise that I'm going through all these, you know, painful experiences in my body and I'm just not feeling, almost feeling like this is taboo, you know?
My boss was a, you know, a male producer, and how do I even start that conversation when I'm still kinda coming to grips with what's happening?
So it was, yeah, it was just kind of that general feeling of being low and also just feeling a bit sorry for myself in like, why is this happening to me?
Especially as a young woman, you're going through so many changes anyway within your body.
Oh yeah.
And your sense of identity, for me, just that sense of identity and how you feel as a woman, how attractive or unattractive you feel, and how you're making your mark within society.
And it felt like this condition, endometriosis just clouded all of that.
And the focus very much was on, okay, how do I start to find those moments day to day where I can feel a bit more normal and never really getting to that point.
So how does someone like you, so, you know, you talked to us about, you were just getting work experience initially at the BBC and now obviously, you've developed this amazing career in presenting, and there are long days sometimes when you're presenting, you can be stood outdoors for hours and hours, you know, it can be really arduous.
How have you managed to do what you've done whilst having this condition?
And whilst, I don't know, was it throughout your whole period you'd have symptoms?
Or would it- Yeah.
It would be throughout my whole period, really- So that's kind of about a quarter of the time.
Well, that's it.
'Cause sometimes the whole period for me would be like seven to 10 days.
It wouldn't be like, you know, four days.
It would, yeah.
It's a big chunk of your month- More than a quarter of your month.
Yeah, exactly.
You are suffering these, you know, awful symptoms.
Yeah.
I mean- You've gotta go to work and stand in a field or stand in a studio or- That's it.
You know, meet all these new people and talk to all these, how did you do it?
Yeah, well, to be honest, it made me feel like I had a split personality, and probably a lot of the time I was acting, you know, 'cause I would go to the toilets and stare at myself in the mirror after having a cry.
And then I remember so clearly I'd look in the mirror and then I'd smile at myself.
I'd like force myself to smile to try and get myself, one, like to try and make my eyes look less, you know, red and puffy after crying.
But try and like just get myself in the zone where okay, things are okay.
And then- Just put your mask back on.
It's like, put your mask back on.
Put that back on.
Yeah.
And again, when I reflect on that, I think back, it makes me feel quite sad.
I almost feel sorry for that person.
Like, God, it's exhausting doing that.
It's exhausting doing that.
And sometimes, you know, I'd get home at the end of the night, I remember we were filming in studio for "Mastermind," which was for four weeks.
And we'd be doing like four or five shows a day.
It'd be 12 hours a day.
Drive to home in the dark 'cause it was in the middle of winter, come back in the dark 'cause of winter.
I'd get home and just wanna pass out, you know, just not wanna speak to anybody and just lie there and try and decompress before starting all over again.
So yeah, it was kind of trying to block out a lot of those mental emotions and then trying to deal with the physical, any which way I could, you know, at work.
And you're just trying to segment things, as much as possible.
So let's pick up then from, you've received your diagnosis of endometriosis.
You are having a pretty terrible time of it, at least three quarters of the month.
And the rest of the month, you're probably dreading what's coming and your mum is now gonna have a hysterectomy.
Let's pick up from there.
So how was that experience then of witnessing, I guess, witnessing your mum going through what she went through and knowing that you have the same condition as her?
It was a really scary time.
You know, I remember going to see my mum in hospital after she'd had the full hysterectomy and- So when you say full hysterectomy, did she have the ovaries removed as well?
Yeah, like the, I mean- The tubes and- Everything.
Might actually- Everything, no, no.
Yeah.
Like, yeah, I mean, she'd just call it a full hysterectomy.
So in my mind that was just everything was taken out.
Okay, is there sometimes where you can have- So sometimes, they'll take just the womb, sometimes and leave the ovaries behind.
Oh, yeah.
Sometimes they'll take the womb, the fallopian tubes.
Right.
Sometimes they'll take the cervix and sometimes leave it behind, so- I see- There are lots of different types of hysterectomies, Got you.
And- In my mind, yeah.
You think she had everything with everything- Yeah, exactly.
But yeah, just seeing her in hospital after having that, which is obviously a big operation, and you know, she was completely out of it in a lot of pain.
She was in hospital for quite a while after the surgery.
It was two things.
Obviously from, you know, a daughter's point of view, just wanting to see my mum well again and just focusing on her and then, in those moments, when now I was by myself or back at work and, you know, experiencing the pain again, it was like, "Is this the destination for me?
Is this what's gonna happen to me?
" And then having pockets of time thinking, well, when could this potentially happen to me?
Is that gonna mean that if I don't have kids at the same time my mum had kids, then I won't be able to have them, you know?
And how does this actually impact on the rest of my life and what I want in certain points of my life as a woman, you know?
And it became just quite overwhelming, and a real inducer of anxiety trying to plot out how I navigate my life in a different way from seeing that kind of end result on what it's done to my mum and her body.
Then after time, you know, when my mum recovered, she felt so much better as a result of having that operation.
So for me, it was good to see that.
Yeah.
But, you know, obviously having that type of operation that affects what you can, you know, affects having kids, doesn't it?
Yeah, yeah, of course.
So as I, you know, as I grew older and dealing with the condition.
And it's still, you know, it makes me think in a different way.
And my, going back to the Zoladex injections, my symptoms got so bad that I couldn't continue on that route.
It just wasn't realistic, you know?
So actually, I came off them and then ended up going on the Mirena coil, Yeah.
Which I'm still on at the minute.
And that was something that actually really helped to control the condition and make me start to just realise what a normal life without that kind of pain or focus on the condition or labelling myself as much as, you know, having that condition Yeah.
Was.
and that kinda started to change my thought process going forward as well.
So when was that?
So when was the Mirena coil- Gosh it was years ago now.
Probably around a decade ago.
Okay.
Yeah.
Okay, well good.
Yeah.
That's good.
And I guess it's important to highlight that with this condition, endometriosis, there's different things work for different people.
The Zoladex injections, a lot of people have side effects, but some people they work well for.
And some people, you know, the combined or contraceptive pill or even the progesterone only pill, they get relief.
Some people Mirena.
So what's the outlook then now?
'Cause you did, you mentioned fertility.
We met our partners at a similar time.
Yeah.
Just before Just before pandemic, right?
Yeah, yeah.
Just before, yeah, yeah.
And you are younger than me, but very excitingly you are engaged now.
Yes.
Congratulations.
Thank you.
And, you know, one of the things we know, which you've touched upon is that endometriosis can affect fertility.
So what are your thoughts when it comes to fertility?
Do you want to have children or- I do and I get quite emotional about it 'cause I feel like I'm in this point at the minute where it's like, there's two sides of me.
So I really want to have children, but I'm also really scared to take the coil out and then go through that pain again.
And I almost makes me feel really bad about myself 'cause, you know, sometimes I think when you get to this stage, you're judged a bit more if you don't have kids.
And I feel like, am I being really selfish?
because I'm too scared to really face up to how that condition is affecting my body now as a 30 year old woman.
And if I, you know, if I take the coil out, will I be able to conceive, you know, how much has it affected me?
And so, it's kinda feels very raw and a very, I'm like literally at that point where I need to make a decision.
Do you know what I mean?
And what do I do?
So yeah, that's how kinda things stand at the minute.
And it's something that I think about every day.
Do you?
And I know I just need to get on with it and do something about it, you know?
What do you kinda see as your options?
You thinking about it every day, and I guess what I'm hearing is that, whichever way you turn, there's something that's quite scary facing you.
First of all.
Well, the first thing I need to do is have the coil removed.
Yeah.
Because if I don't have the coil removed, there's no chance of me getting pregnant, you know, at all.
What I'm scared about is the process of having that removed, is it gonna take me back to that stage of having really painful periods and issues with endometriosis, and my symptoms that I used to have, I haven't had for a long time.
And I've been able to just get on with having, you know, a nice normal life and, you know, have really happy times.
So it's kind of, yeah.
It's thinking about that.
It's the fear of the unknown.
Yeah.
And it annoys me that I'm doing that because I'm just wasting time, you know, I just need to grow some balls and get on with it.
But yeah, that's it.
I dunno, I feel silly saying it really, but that is some kind of what I feel at the minute.
There's absolutely nothing silly about saying it.
I think, you know, what you've really kindly shared with us is that from being young, early twenties, you've really suffered.
It's been really hard, not just physically, but emotionally through your work, socially, you know, also seeing what your mum's been through before you.
So it's no wonder that actually, psychologically, you know, it makes complete sense that there is fear of doing anything that could make that come back.
But equally, there's this other thing that you want to explore.
And sometimes, fear can be crippling.
Yeah.
Can't it?
That's it.
But I know I need to, you know, I know I need to make that change.
And it's confronting, I feel like, you know, Mentally, physically.
And it is, as you rightly said, the fear of the unknown in terms of not knowing how my body is going to react.
Yeah.
Before we bring on Sam, who, I'd love for her to give a little bit of input onto what we've just been talking about in fertility and maybe she can give some advice on that.
One of the things I really want to ask you about is, you know, I find it fascinating that it takes on average eight years for a diagnosis to be made.
And I'm so glad in your situation that it was much quicker than that, largely because your mum had had an experience herself of going through it.
And it's not just here in the UK, you know, it's around the world.
This condition does take a long time to diagnose.
I wondered what you think the reasons are for that, having lived through it.
Why do you think it takes so long?
And I guess, for all of us who aren't living with it, how can we be a little bit more understanding and a little bit kinder?
Yeah, I think that's a really interesting question.
And it makes me think of, say if my mum didn't have it, and I was just going through this experience myself, how would I have approached it?
And I think, you know, on the one hand, I'm not sure I would've been as vocal going to the doctors because I feel like I wouldn't have really known what I was talking about.
I had a bit of prior knowledge.
But if I didn't have that prior knowledge, would it have been a bit more of a needle in a haystack getting to the point of the diagnosis?
And I think as women sometimes, you know, and our bodies, our bodies are changing all the time.
We deal with a lot even, you know, when I had painful periods for years and I just thought, well, this is just a part of what we have to deal with.
This is just part of the experience and, you know, maybe I don't need to go to the doctors and have a conversation about this because it just is what it is.
And also, you know, when I think growing up outside of talking to my mum, I didn't speak to anybody about anything to do with like, female reproductive or anything that, you know, connected to the womb or bleeding or the word periods.
It just didn't talk about it.
So I think that might have a part to play 'cause it does really feel like now, there's so much more of an openness now more than ever to talk about all these kinda things.
Yeah.
So I feel like that plays a massive part in it.
And I totally agree, we do need to be kinder to each other in terms of, well, none of us really know what's going on in anyone's life and, you know, what they could be dealing with.
So yeah, a massive thing is, you know, respecting our own bodies and through that, talking about what we're going through, especially to, you know, a GP or friends or family can really help.
But respecting other people as well within that same process and appreciating.
We might not know what they're going through.
I think that all kinda feeds into, as you said, you know, being kind and supporting each other.
Yeah.
And I think, if we are kind and we're willing to listen, and we're willing to understand, then that empowers people.
You know, we're talking about a female condition here, but empowers people to share so much more.
And I think sharing what you're going through, whilst it doesn't fix it, it doesn't take away the physical pain, it can actually not only mean that people can have better mental health, despite what they're going through, but, you know, it fascinates me that you went through what you went through, yet you've managed to succeed because you've had to grit your teeth.
You've had to put that mask on, and you've had to endure like horrendous symptoms without letting anyone around, you know, what's going on.
And, you know, there's obviously something in your personality that has allowed you to be able to grit your teeth and get through it.
But how many people out there don't have that additional, whatever it takes.
And therefore perhaps, you know, there are girls and women out there who aren't fulfilling their dreams, who aren't getting this, you know, getting to the point in their careers or otherwise, or, you know, holding back when it comes to relationships and things like that.
And- Yeah.
it seems very, very unfair.
And it's one in 10, you know, it's common.
This is it, you know, it's astonishing, that figure.
And we shouldn't be going through life with that feeling of, "Despite of I'm doing this despite this," especially if something can be done about it, and we can have more support and more awareness.
It would be nice to get to the point where you're doing something, and you know this is going on in your life, but you do, as you say, you know, have that feeling that you're really grasping at those opportunities, and you're not having to hide a whole part of you because of a condition or something else that might be going on.
So it's, you know, looking forward, it's really heartwarming to know that that could change.
Yeah.
And that might be a massive positive for so many people out there that might be going through, you know, similar kind of condition.
Yeah, well, thank you so much for sharing like all of that information, like such a in-depth information about what your experience has been.
I think this is really good time for us to bring Sam in who's our wonderful GP, Sam Wild, who has a lot of experience in this condition, I think both personally and professionally.
So let's speak to Sam.
(gentle bright music) So Dr.
Sam Wild, GP, clinical lead for women's health at Bupa.
Thank you for coming back and joining us again on the podcast.
Having me again.
And let's start off by hearing a little bit about both your professional and actually also your personal experience of endometriosis.
So I'm a GP of over 20 years now and always had a special interest in women's health and been working as a women's health clinical lead at Bupa for the last few years.
But I was at medical school actually when I was diagnosed with endometriosis.
So I have that lived experience too, can really empathise with everything that Michelle was saying.
You know, exactly the same experiences but had the Zoladex as well.
Absolutely hated it.
I remember having to go onto the ward where I was working as a surgical house officer and asking the nurse to inject me each month, and it was just horrendous.
I dunno how I got through my time doing that.
So I had loads and loads of different hormone treatments.
Got married as soon as I could.
I was lucky I met my husband when I was young, so I had my children really easily, actually, no problems at all.
Had two kids and ended up having a hysterectomy in my mid thirties.
So I've been through it all, which I think that's really driven my passion towards what I do now.
Yeah.
You know, really trying to empower women to get that support that they need.
Yeah.
And just out of interest, being a medical student, how long did it take you from first, I guess, going to seek help to getting a diagnosed, having the laparoscopy and getting a diagnosis?
So again, I was really lucky.
So I think I probably had it, they used to say it didn't happen in teenagers.
I went on the pill when I was about 14 because I was suffering my period.
So right from the very start.
And so, suffered all the way through and then it was at medical school and it got really bad.
And actually, I was really lucky that I had private medical insurance then.
So I was able to go to a GP and get diagnosed very quickly.
I don't think it was particularly because I pushed it, I don't know how great my awareness of endometriosis was at that time.
I think I was just very lucky that I was able to get seen quickly.
One thing I just have to say, I notice how we all sit here, and we're really good at identifying ourselves as being lucky, aren't we?
You know, "I'm lucky"- Oh, yeah.
"I've got diagnosis quickly" Not really.
Yeah.
It's the way it should be- Not really lucky.
It's just the way it- Um, and another thing, I'm just gonna flag that you said is, you know, which I really appreciate and I'm sure Michelle does too, that you were really lucky that you met your life partner so early in life and- Yeah.
Because you mentioned earlier, Michelle, about people do judge.
Yeah.
You know, when you get to, so I was 40 when I had my little boy, but people do judge that, you know, "Oh, you don't have children yet.
" And it's actually, if you haven't met the right person to do that with, it's not always a choice.
You know, people assumed with me it was, I prioritised career, I didn't.
Yeah, same.
Just hadn't met the right person.
Yeah, that's it, isn't?
You're lucky if you do.
Yeah.
And I think I felt that pressure that I, you know, I wanted to start to see if I could have children.
Yeah.
Yeah.
So thank you for sharing that and also for sharing the personal journey.
Firstly, I always ask our expert when they come in who's just listened to our conversation to pick up anything you've heard.
Like, feel free to correct me if I've said anything wrong or, you know, anything that came up that you'd like to comment on, correct or add something to.
Yeah, so I mean, to start with, just to add to the start.
So as you said, "One in 10 women in the UK.
" So I always compare to diabetes, but yeah, you're right with asthma as well.
So it's one and a half million women in the UK, that I was listening to that that's like basically one whole continent of the world.
It's crazy isn't it?
Wow.
It's crazy.
Yeah.
And yet 64% of women between the ages of 16 and 24 have never heard of it.
Wow.
64%?
Never even heard- Never heard of it.
The words.
And 45% of women can't name any of the symptoms of it.
Wow.
So we're going wrong somewhere, aren't we?
It's shocking, yeah.
Definitely, we're just not talking about it enough.
But that's fascinating isn't it?
That the majority, well, one in 10.
Now imagine sitting here and saying that 64% of people have never heard of asthma or diabetes, That's crazy.
Yeah.
So that's, I mean, that's number one, that's where we're going wrong, isn't it?
That people aren't aware of this.
I believe it should be taught in school.
You know, this is so common.
Everybody should know about it, not just girls.
Girls and boys should know about this in school.
Absolutely.
I've included it in my books for girls age nine to 13 and it's called "You Grow Girl.
" And I think, you know, knowledge is power, or it might be a little bit scary to know that these things can happen, but it's much more important though we're aware of it.
And then if they do happen, you can get the right support straight away.
Exactly.
Totally.
People suffer in silence.
But as Michelle said, I didn't talk to people about it.
Did you not?
I don't think I talked to anybody about it during my twenties and thirties.
Wow.
Even though you were working as a junior doctor?
Yeah.
I just felt I had to just get on with it and, you know, I'm quite happy, I'm open, I'm an open person.
I'm quite happy to talk about other things.
I don't know why, but I just felt, I just need to get on with this.
Maybe I thought people weren't gonna understand.
I don't know.
Isn't it mad to think as well that at the time if you did talk about it, there were probably so many people that actually were going through a similar thing.
Exactly.
Yeah.
Yeah, you know.
Well, almost, almost definitely.
As you discovered, Michelle.
Yeah.
You've had a friend- Suffer with it.
Who was going through the same in silence.
Yeah.
So how do we change that?
What's the solution?
Keep talking about it.
Yeah.
As you said, yeah.
Start educating schools.
We do a lot of of work now with businesses as well.
So we are talking to managers, employees about, you know, raising their awareness of it and what can be done to support women within the workplace too.
So I think, you know, we've just gotta speak about it as much as we can and just normalise that conversation.
Talking about periods is still very much of a taboo, isn't it?
So it's not just endometriosis, it's periods as a whole.
Yeah.
I think the sound of it as well, it sounds complicated, doesn't it?
Yeah.
And I remember when I was growing up being labelled with endometriosis as a condition.
Yeah.
You know, if you were to say, "I have endometriosis to somebody," my thoughts and feelings where they'd be like, whoa, Yeah.
don't wanna talk about that because it sounds complicated.
Yeah.
You know?
Yeah, and I know they've got a lot of the sort of support networks out there.
They call it endo for short, don't they?
Endo warriors and endo, which is perhaps a bit still, it's a bit of a weird word still, but you know, it's a bit more manageable, isn't it?
Yeah.
Yeah.
I think you're right.
I think a word like endometriosis, you just think, I can't really get my head around that, too complicated.
I'm shutting off.
But I mean, we know we do still live in a man's world to some extent.
We know, you know, the past couple of years it feels like there is finally some movement from government recognising that women have had a bit of a raw deal and still have a raw deal when it comes to our health.
And I think there's probably no denying that if this was a condition that affected men as well as women or just men, then maybe 64, if it affected men, I'm sure more than 64% of women would've heard of it, for sure.
Sam, what else, any other comments from the chat?
Again, I think, yeah, just when you were talking about Michelle at work.
So one in six women with endometriosis give up work.
Do they?
so again, scary stats, 55% they've had to have time off work due to- That's not surprising having heard Michelle's experience, because, you know, as I mentioned, I think it's incredible that you've managed and you as well.
Sam, you know, being a junior doctor is hard work.
Yeah.
But then it's the impact, you know, in other areas of your life.
Like, you know, you were saying mentally, I dunno whether you felt similar.
It's like you're carrying an ongoing but actually it is destroying another part of you whilst you're doing that.
That's it.
I think, you know, it's not just the pain, is it?
It's that fatigue, it's that just the mental exhaustion as well.
I used to go to work and come home, you know, six, seven o'clock after I'd finished surgery and just go straight home to bed.
And I did that for years.
I had no social life.
It would keep me awake at night as well, you know, not just when I was on my period, but it ended up being throughout the month, and yeah.
And you just learn to live with it.
That's the thing.
You sort of adapt and you just, again, I didn't really kick up at first, I just got on with it.
Yeah.
I can't help but just sort of know that there's so many things that we're discussing that overlap with the conversations that we had recently about menopause, about how women have this determination to just grit their teeth and get on with it.
How they feel that there's this stigma, and it's difficult to raise it and, you know, especially raise it at work that women leave their jobs that, you know, there's a lot of similarities but that, you know, this is affecting women from teenage years.
Yeah.
Yeah.
And women are also finding that they're missing out promotions.
Because of it, they're suffering financially because of it as well.
So, you know, it's really creating an inequality in the workplace too.
I think that's a really good point as well 'cause if I think back to when I, you know, started in tele, I knew that I needed to be in the building, right?
I knew that I just needed to keep going 'cause you've got this one opportunity.
If you don't take it then no one might be interested anymore.
So it was again, that focus of trying to ignore what was going on to grasp this new opportunity 'cause I was scared that, oh maybe I'm not gonna be, you know, if I tell anybody, maybe they're not gonna take me as seriously, maybe I'm not gonna be able to continue within this job.
And again, there lies that separation because you want to support people and raise awareness, but at the same time you're hiding things 'cause you think you're gonna get judged and no one's gonna want to work with you.
I would like us to get onto a more positive note if we can.
So I think, I think what would be really great from both of you would be, there'll probably be people listening to this thinking I have this condition, or I care about somebody, I know somebody and I think they have this condition.
What should they do?
How can they take positive action towards one, I guess getting that diagnosis, and two, finding some form of management plan, treatment plan that's gonna help alleviate their symptoms.
What would you say, Michelle?
Well, you know, even just talking about this today for me has been so lovely- Yeah.
And I think it is coming back to that, you know, as women you wanna support other women and that is so key.
And just think the more we can speak out about how we're feeling, that just goes, you know, hand in hand with raising more awareness and learning, learning from each other about, you know, the condition 'cause my specific symptoms, my experience of the condition could be very different to somebody else's.
It varies for different people, doesn't it?
So for me it would be just, I mean, it's given me the confidence to speak out about it even more, and I want to understand other people's journeys and how they are.
And I guess that goes back to being kind and being ready to be an ear and sometimes, asking those questions, you know, if you feel like you're in that safe, comfortable space to do that, asking those questions and seeing how people are, I think it's important.
Yeah.
Definitely.
Sam?
So yeah, education.
But I think for an individual to think of what symptoms you're experiencing, keep a period diary if you can so that you can go on to the GP with these are the symptoms that I'm experiencing and when, you know, say to the GP, "Could this be endometriosis?
" So, you know, we always talk about GPs.
If we know what someone's thinking, it really helps us with our management to know where they're coming from.
So, you know, say, could it be this, you know, "I'd like to be investigated.
What do you think about that?
" And hopefully, you know, if they don't think it's that, they can explain exactly why.
But if they do think it's that, then you'll on the next steps then to be able to get referred for investigations and then get some management sorted.
And, Sam, before we end, I would love for you to talk us through kind of what that looks like, what that journey looks like in terms of what investigations are likely to happen in what order, and also what kind of are the potential treatments, even if we just list them.
But one of the things I wanted to reflect on, I wanted to just share really that I think making this podcast and hearing both of your stories, it always gets me thinking about my own medical practise.
And I think I used to think that because the tests to diagnose endometriosis is so invasive, it is a general anaesthetic and an operation.
I think I used to almost make the assumption that my patients perhaps wouldn't always want to go down that path.
And even though they have the symptoms of endometriosis, might wanna skip that and go straight to treatment options.
And I think, you know, just having this conversation has made me reflect and think, gosh, but when you've been through so much, like for many patients from the age of 13 or for 14, for years and years of this incredibly crippling pain physically, but also pain in every other aspect, actually laparoscopy is quite a small procedure in comparison to what they've already been through.
And I think it's kind of rewritten that for me slightly.
And one other thing I just wanted to mention is, I know we've been talking about women throughout this conversation, but we do also recognise that there are people who don't identify as women who are affected.
And we want them to feel the part, the part of the conversation.
So sort of more the scientific bit then, Sam.
Okay.
If somebody thinks they have endometriosis or might and they go to their GP, and they share that with them, what can, and what should they expect to happen?
Okay, so the GP will start by obviously asking them loads of questions about their symptoms.
They will probably ask to examine them as well, and that will involve an internal examination too, quite often, because if there has been a lot of scarring left by the endometriosis, they may be able to fill that.
They may also be trying to exclude other conditions as well.
They will sometimes refer for an ultrasound scan.
Again, we don't always see endometriosis on an ultrasound.
We can see sometimes if there's a cyst, but we wouldn't necessarily see it on its own.
But again, to exclude other conditions and getting an ultrasound is usually a lot quicker than having a laparoscopy.
The next step is then to be referred to a gynaecologist to have a laparoscopy.
And what they would probably do is start you with some treatment in the meantime, depending on, you know, how long that weight's likely to be.
And that goes from things like painkillers to the hormone type treatments that we've talked about already.
And that could be things like the combined pill, and the Mirena coil.
And so then, when you see the gynaecologist, they're likely again to just go through that same sort of routine of the history and examination, but then get you in for the surgery.
And at laparoscopy as well as diagnosis, they can also do some treatment then.
So that's another reason really why women should be offered it.
Because what they tend to do is they either remove or they burn away some of the patches of endometriosis if they can see them there.
And actually, that, for some women can increase their fertility immediately straight after they've had that done.
There's no guarantee, but it does work for some and, you know, some people will have a bit of relief for a while until sometimes it grows back again.
Okay, great.
I could see you nodding away there.
Yeah, no, 'cause I, yeah, I went through that experience.
I had the laparoscopy and then had laser treatment at the same time, so yeah- When you just say it's just bringing back those memories of, you know, the different stages and, you know, the everything that you go through at different times with the condition.
Yeah.
And I know you're not here, Sam, to give specific advice to Michelle, but I just wondered what your thoughts were when she's sort of thinking now, looking forward, you know, at the moment her symptoms are pretty well managed but she's considering, you know, she's thinking every day about the fertility aspect, potentially having children.
If she could takes out the Mirena, could her symptoms come back?
But equally she wants to find out where she's at and just, you know, I know you're not here to do a consultation, but I know you've got the wisdom to probably say something really helpful that, you know, not just for Michelle but for other people who might be experiencing the same.
So not everyone with endometriosis is going to suffer with infertility.
So I think that's really reassuring to start with.
And it's often a misconception that everybody would, so they say about 30 to 50% will suffer, but also the degree of endometriosis that you have, again, doesn't correlate with infertility.
So we don't really know why the association is there.
Sometimes it can be obvious because there's maybe some scarring and some distortion of the tubes and things, but sometimes, someone can have very mild endometriosis or it looks like it's mild, but it does affect the fertility.
So you can't really draw any conclusions about how things are gonna be until you start trying.
And I know it's very difficult when you come off the treatment, but your symptoms don't normally recur straight away.
And so, we would recommend that somebody started trying straight away.
And again, there's always that option of having another laparoscopy.
So if there is quite a lot of active endometriosis there, they can start to treat that and, you know, then get you trying to conceive straight after again.
That's good advice.
Thank you.
I know, I appreciate that.
So yeah, it's, you know, it's really difficult and you are always gonna have that worry, and that sort of uncertainty there, but you've just gotta try when the time's right.
No, and thank you for that 'cause it's been a big thing for me even just vocalising those kind of fears.
Yeah, and I think a lot of women with endometriosis, that's one of the things we worry about, you know?
And for me, that was my main thing.
I knew I wanted to have children, but it did really give me that extra pressure to get on and do that.
Whereas maybe, in hindsight, I would've felt more comfortable leaving it a bit later now.
I don't know, but how I felt then.
Yeah.
Very different to know.
Yeah, yeah.
It's like, does that help like improve It really does.
The hope a little bit?
It does, yeah.
And it is just kind of, sometimes you have all these thoughts in your head, and it just almost becomes like a spider web of thoughts and feelings.
So even just talking about it and, one, knowing that other people are going through it, but two, you know, just kind of compartmentalising it and dealing with each stage separately and seeing how you get on feels far more manageable than just a whole mishmash of thoughts and fears, you know, that you're not sharing.
Yeah.
And I think even getting in that next appointment with your GP and not necessarily taking action, doing anything, but you know, almost just even that conversation with Sam, then just kind of figuring out exactly what the next steps would be and then figuring out, you know, what your next steps are from there and help you figure out where the next plan forwards, which I don't know, I just feel really excited about.
(team laughing) You got a feeling.
It's not very scientific of that, is it?
But anyway, I just wanna say a huge thank you to both of you.
That was such a real, you know, I learned a lot from that conversation, as I'm sure did many people out there.
And I think a message to anybody listening, if you've heard something today that's resonated, that's hit a note, and you think actually this is something that you are suffering with, or you just haven't felt able to go and speak to your GP or speak to those around you, I think, first and foremost, what we're all saying is just talk about it.
Just share what you're going through.
There's no shame, you're not alone.
In fact, you know, this is very common and there is help available.
So thank you both so much.
Oh, thank you.
Thank you.
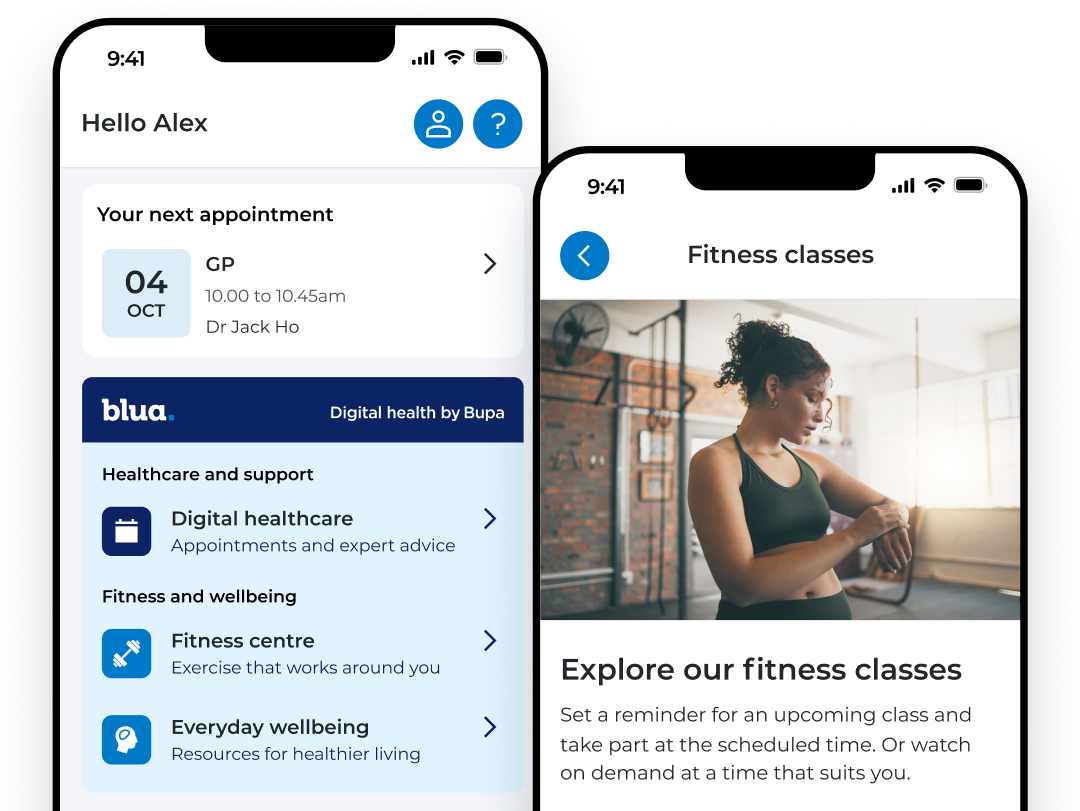
My Bupa, everything your people need in one place.
A digital account provides a convenient way for your people to get the support they need. Personalised to your employees level of cover, they can access a range of resources and services available to them.
To sign into the My Bupa app, your employees can use their existing Bupa account, or by creating a new digital account.
Scan the QR code with your phone camera to download the app.
Further resources

Women's health hub
Get guidance on key health topics including periods, menopause and endometriosis. Along with everyday wellbeing advice for at home and in the workplace.

Healthy Me. Blog
Designed to help you live a healthy lifestyle, find help and advice from our experts on a range of topics.





