Physiotherapy for lower back pain
Your health expert: Elaine Dechow, Chartered Physiotherapist
Content editor review by Rachael Mayfield-Blake, Freelance Health Editor, April 2023
Next review due April 2026
Physiotherapy is a treatment that helps to improve the movement and function of joints and muscles. It can help to reduce lower back pain, get you moving normally again, and reduce the risk of back pain returning. Physiotherapists use different techniques to help with lower back pain, and offer advice on how to look after your back.
About physiotherapy for lower back pain
Physiotherapists focus on restoring movement and function to your whole body after you’ve been affected by an illness or injury. They look at how the nerves, muscles and bones in your body are affected, and how treatment with exercise therapy and manual therapies can help. They’ll encourage you to take an active part in your rehabilitation, rather than relying on just being treated by them.
Find a physiotherapist
Your GP may refer you to a chartered physiotherapist through the NHS, or you may be able to book an NHS physiotherapist yourself. This is known as self-referral. Ask at your GP surgery to see if this is available in your area.
You can also have private physiotherapy. You can search online directories to find a private physiotherapist in your area. If you have private health insurance, check what your insurer covers before you book an appointment.
When you book your own physiotherapist, make sure they’re registered with the Health & Care Professions Council (HCPC ). This means they’ve completed approved standards of training and follow the HCPC rules of professional conduct.
Physiotherapy procedure
When you first see a physiotherapist, they’ll ask you about your medical history. They’ll ask about any medical conditions you have, your lifestyle, your work environment, and any medicines you take. They’ll also want to know what symptoms you’ve had, and what tends to trigger them.
Next, they’ll examine you to see how you move and how your back is working. They may also check how well your nerves are working. You may need to remove some clothes when you go for physiotherapy, so that your physiotherapist can see and feel your back. You can ask to take someone along with you if you prefer.
Your physiotherapist will explain the treatment they recommend, and how this may help your lower back pain. They’ll also warn you about any potential risks of treatment. If you’re unsure about anything, don’t be afraid to ask. It’s important that you fully understand what your physiotherapist recommends because they’ll ask you to give your consent to go ahead with treatment.
Your GP or physiotherapist may recommend physiotherapy as part of a treatment package that includes hands-on manual therapy, an exercise programme, painkillers, and psychological support. Having a combination of treatments like this may give you the best chance of easing your lower back pain. Your physiotherapist will also help you to understand what’s causing your lower back pain so you can take steps to manage it.
At the end of your first session, your physiotherapist will usually tell you how many sessions you’ll need and how often. This will depend on how lower back pain is affecting you and how you’re managing your symptoms. You may just need a one-off consultation, or your therapist may recommend a course of physiotherapy appointments over a few months.
Exercise and staying active
Generally, keeping active is the best thing for lower back pain. It can get you back to work faster, and you’re less likely to have long-term problems, or get lower back pain again. Even if you’ve had lower back pain for some time, an exercise programme with a physiotherapist can provide relief and get you moving again.
Exercises can help to improve flexibility, mobility, and strength in your lower back. Some people find it easier to exercise with others, so your GP or physiotherapist may suggest you join a group exercise programme.
A physiotherapist can advise you on exactly what exercises are right for you, and how to do them. Below is an overview of the different types of exercise you may come across.
Aerobic exercise
This is any exercise that gets you moving and increases your heart rate. Aerobic exercise can help with any stiffness you may have and will keep you mobile. It will also help to manage your weight and can give your wellbeing a boost. Your physiotherapist may recommend low-impact aerobic exercises to start with, such as walking, swimming, and using exercise bikes and step machines. They’ll encourage you to do more as you feel able. They’ll probably advise you to exercise for around 30 minutes, at least 5 times a week but their recommendations will be specific to you.
Stretching exercises
Stretching improves flexibility in your spine and reduces tension in the muscles that support your spine. You usually do these exercises every day. A typical stretching exercise is to lie on your back with your knees bent and your feet on the bed. Then let your legs gently roll to the left-hand side and then over to the right-hand side. Ask your physiotherapist about more you can do.
Strengthening exercises
Physiotherapy exercises for lower back pain to strengthen core muscles can sometimes be included as part of an exercise programme. Your core muscles are the tummy (abdominal) muscles around your stomach, the muscles in your back, the buttock (gluteal) muscles, and those around your pelvis.
Manual therapies
Your physiotherapist may suggest manual (hands-on) techniques to treat your lower back pain. This will always be alongside an exercise programme.
- Mobilisation. Your physiotherapist will use slow, gentle, rhythmical movements to stretch your spine and help your back return to its normal range of motion.
- Manipulation. Your physiotherapist will do controlled thrusting movements with their hands at a particular point of your spine. You might hear a ‘pop’ sound when they do this but don’t worry; this is normal. Not all physiotherapists use this technique and they won’t do it unless they’ve explained the reasons for doing so. You’ll need to give your consent for this procedure to be done.
- Massage. Your physiotherapist may use massage to treat lower back pain.
Physiotherapists used to offer other treatments, such as transcutaneous electrical nerve stimulation (TENS) and acupuncture. But these treatments aren’t recommended in guidelines for lower back pain because there’s not enough evidence that they help. Ask your physiotherapist for more information.
Uses of physiotherapy
If you have lower back pain that’s causing you significant problems or doesn’t get better after a few weeks, it could be worth seeing a physiotherapist. Physiotherapy can be useful for different types of back pain, and may help the following.
- Non-specific lower back pain – where no cause (such as a health condition or injury) has been found.
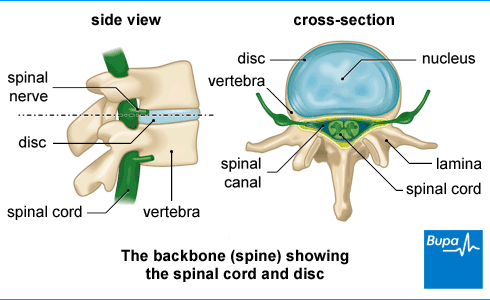
- Sciatic pain. This spreads from your back down your legs and may be caused by a prolapsed disc (when a disc in your spine bulges out of its normal shape and presses on a nerve).
- Back pain caused by ageing of the discs in your spine (degenerative disc disease).
- Spinal stenosis. This is when the space around your spinal cord narrows, putting pressure on your spinal cord and causes pain.
Aftercare for physiotherapy
Your physiotherapist will give you some advice about what you can do at home to help your lower back pain. This may include how to improve your posture, and how to make sure your car seat or office chair is set up properly. If you sit at a desk all day, it can play a big part in back problems. Your physiotherapist may give you some recommendations about your chair and screen height and advise you on how often to take a break and move around during the day.
They’ll also usually give you a home exercise programme. This is a series of exercises to do during the week. Your physiotherapist will adjust the programme at each appointment, as you make progress.
Physiotherapy will be only one part of your treatment for lower back pain. You may also need to make some changes to your lifestyle and keep as active as possible. Your physiotherapist may advise you to do some regular exercise to keep your back mobile and strong for everyday activities. You may be advised to lose any excess weight too. If you have a high body mass index (BMI) or are overweight, it can put an unnecessary load on your spine and add to your pain and discomfort.
Side-effects of physiotherapy
You may find that certain exercises and movements make your lower back pain worse. Your physiotherapist should monitor this and show you which exercises to avoid, and which ones will help relieve your pain.
Manual therapies, such as manipulation, can have side-effects. These usually aren’t serious and only last for a short time. For instance, you may feel some stiffness or discomfort in the area that was treated.
If your home exercises include movements that your muscles are not used to, it can cause your muscles to ache the following day. It’s perfectly normal and will get better as your muscles adapt and get stronger.
It’s possible that manipulation could cause a more serious injury, but this is rare. Your physiotherapist should talk to you about the risks of manual therapies before they do any treatment.
Your physiotherapist should also check how you’re feeling as they do any ‘hands-on’ therapy and stop if you have any pain or discomfort.
Alternatives to physiotherapy
There are different types of manual therapy that can treat lower back pain, which all take a slightly different approach. In addition to physiotherapy, manual therapies are used by the following.
- Osteopaths look at the health of your body as a whole and aim to make sure all your bones, muscles and joints are working smoothly together. They focus on manual therapies to get your body back to a state of balance.
- Chiropractors, like osteopaths, look at your body as a whole. They’re interested in how problems with your bones, muscles and joints affect your nervous system and general health. Their focus is on manipulation of the spine – but they may use other techniques too.
Manual therapy can be done in many different ways, and can vary according to different types of training and also between individual practitioners.
It’s your choice which type of practitioner you see. But if you would like NHS treatment, you’ll most likely be offered physiotherapy because the other services are often not funded.
Physiotherapy services
Our evidence-based physiotherapy services are designed to address a wide range of musculoskeletal conditions, promote recovery, and enhance overall quality of life. Our physiotherapists are specialised in treating orthopaedic, rheumatological, musculoskeletal conditions and sports-related injury by using tools including education and advice, pain management strategies, exercise therapy and manual therapy techniques.
To book or to make an enquiry, call us on 0345 850 8399
Chiropractic for lower back pain
Chiropractic is a treatment where a practitioner called a chiropractor uses their hands to help relieve problems with the bones, muscles and joints, such as lower back pain.
Osteopathy
Osteopathy can help you to manage back pain, neck tension, aches and pains.
Epidural injections for lower back, leg pain
Sometimes spinal injections (epidural or nerve root injections) are used to treat chronic back and leg pain.
Did our Physiotherapy for lower back pain information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- What is physiotherapy? World Physiotherapy. world.physio, accessed 31 March 2023
- Physical therapy (PT). MSD Manual Professional Version. www.msdmanuals.com/en-gb/professional/special-subjects/rehabilitation/physical-therapy-pt, accessed modified September 2022
- Personal communication, Elaine Dechow, Chartered Physiotherapist, 12 April 2023
- What is physiotherapy? Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 7 March 2023
- Find a chartered physiotherapist. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 24 January 2023
- Physiotherapists. Health and Care Professions Council. www.hcpc-uk.org, updated 17 September 2018
- Getting help for back pain. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 29 January 2019
- GP mythbuster 15: Chaperones. Care Quality Commission. www.cqc.org.uk, last updated 23 December 2022
- Consent and physiotherapy practice. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 4 April 2022
- Low back pain and sciatica in over 16s: Assessment and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 11 December 2020
- Low back pain and sciatic. Patient. patient.info, last edited 16 October 2020
- Musculoskeletal lower back pain. BMJ Best Practice. bestpractice.bmj.com, last reviewed 30 December 2022
- Back pain – low (without radiculopathy). NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised November 2022
- UK chief medical officers' physical activity guidelines GOV.UK. www.gov.uk, published 9 January 2020
- Keeping active. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 13 March 2018
- How to get more active. Chartered Society of Physiotherapy. www.csp.org.uk, accessed 2 April 2023
- Stretching for back pain relief. Spine-Health. www.spine-health.com, updated 21 October 2022
- Spinal manipulation: What you need to know. National Center for Complementary and Integrative Health. www.nccih.nih.gov, last updated September 2022
- Moorman AC, Newell D. Impact of audible pops associated with spinal manipulation on perceived pain: A systematic review. Chiropr Man Therap 2022; 30(1):42. doi: 10.1186/s12998-022-00454-0
- Rehabilitative measures for treatment of pain and inflammation. MSD Manual Professional Version. www.msdmanuals.com, modified September 2022
- Assessment of back pain. BMJ Best Practice. bestpractice.bmj.com, last reviewed 28 February 2023
- Sciatica (lumbar radiculopathy). NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised February 2022
- Spinal stenosis. BMJ Best Practice. bestpractice.bmj.com, last reviewed 28 February 2023
- How physiotherapy can help you at work. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 21 May 2019
- About osteopathy. General Osteopathic Council. www.osteopathy.org.uk, accessed 31 March 2023
- GCC patient guidance. Visiting a chiropractor. General Chiropractic Council. www.gcc-uk.org, published February 2022
- Complementary and alternative medicine. Patient. patient.info, last edited 1 March 2022
- NHS and private treatment. General Osteopathic Council. www.osteopathy.org.uk, accessed 31 March 2023
- Video exercises for back pain. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 27 May 2020



