Transurethral resection of bladder tumour (TURBT)
Your health expert: Mr Aziz Gulamhusein, Consultant Urological Surgeon
Content editor review by Rachael Mayfield-Blake, Freelance Health Editor, March 2023
Next review due March 2026
Transurethral resection of a bladder tumour (TURBT) is an operation to diagnose and treat early bladder cancer. You may need TURBT if you have an abnormal growth (tumour) in your bladder.
About TURBT
During a TURBT operation, your surgeon will remove any abnormal growths (tumours) in your bladder. These will be sent to a lab to find out if they’re cancerous and if they have grown into your bladder wall.
TURBT is the first treatment you’re likely to have for what’s known as non-muscle invasive bladder cancer. This is when the tumour is on the lining of your bladder and hasn’t grown into the muscle layer below. It’s also called early bladder cancer. Non-muscle invasive bladder cancer is the most common type.
Straight after the procedure, you’re likely to have a single dose of chemotherapy delivered into your bladder. This will help to reduce the chance of the cancer coming back.
Preparation for TURBT
You’ll meet the surgeon who is going to do your procedure to discuss your care and find out what to expect. It may be different from what we describe here because it will be designed to meet your individual needs.
You may be able to go home on the same day as your procedure but you may need to stay in hospital overnight.
Your surgeon will explain how to prepare for your procedure. If you smoke, they’ll advise you to stop because smoking increases your risk of complications after surgery. Smoking is also one of the main causes of bladder cancer so if you stop now, it may help to stop the cancer from coming back.
You’ll have either a general anaesthetic or a spinal anaesthetic before TURBT. If you have a general anaesthetic, you’ll be asleep throughout the operation. If you have a spinal anaesthetic, you’ll be awake but feel numb from the waist down.
A general anaesthetic can make you sick so it’s important that you don’t eat or drink anything for at least six hours before your procedure. You can usually drink water up to two hours before, but check with your anaesthetist or surgeon and always follow their advice.
You may be asked to wear compression stockings to help maintain your circulation and reduce the risk of forming blood clots in your legs. You may need to have an injection of an anti-clotting medicine as well as or instead of wearing compression stockings.
Your nurse or surgeon will explain what will happen before, during and after your operation, including any pain you might have. If you’re unsure about anything, ask. No question is too small. It’s important that you feel fully informed so you’re in a position to give your consent for the operation to go ahead. You’ll be asked to sign a consent form.
Looking for cancer cover that supports you every step of the way?
If you develop new conditions in the future, you can rest assured that our health insurance comes with full cancer cover as standard.
To get a quote or to make an enquiry, call us on 0800 600 500∧
TURBT Procedure
Depending on how many tumours you have and how big they are, the operation can take between 15 minutes and one and a half hours. Before the operation starts, your surgeon may give you antibiotics through a drip or injected into a vein.
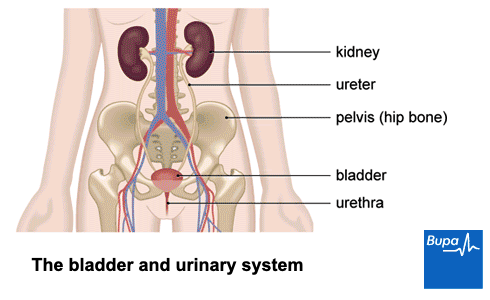
Your surgeon will put a thin, tube-like telescope called a cystoscope into your urethra (the tube where pee comes out of your body) and up into your bladder. A camera lens at the end of the cystoscope will send pictures from the inside of your bladder to a monitor, where your surgeon can see them.
Your surgeon will then pass surgical instruments through the cystoscope to remove the tumour. These instruments use heat from electricity or a laser to remove the tumours. The heat will also stop any bleeding after the tumours are removed.
Your surgeon will also remove some deeper tissue to check if the cancer has spread into the bladder wall. These tissue samples will be sent to the laboratory to be tested.
At the end of the operation, your surgeon will remove the cystoscope and put a thin, flexible tube into your urethra. This is called a catheter and is connected to a bag which will collect your pee.
Your surgeon will put chemotherapy into your bladder through the catheter. This goes in straight after the operation and will stay in your bladder for an hour before it’s drained out. This is to help reduce the risk of the bladder tumours coming back. It doesn’t cause the usual side-effects of chemotherapy.
Aftercare for TURBT
You’ll need to rest until your anaesthetic has worn off. You may need pain relief to help with any discomfort as the anaesthetic wears off. You can eat and drink as soon as you feel ready.
You may need to keep wearing compression stockings until you’re up and about to help maintain circulation. It’s best to get out of bed and move around, even if you don’t feel like it. This will help to prevent chest infections and blood clots in your legs.
Having a general anaesthetic can really take it out of you. You might find that you're not so coordinated or that it's difficult to think clearly. This should pass within 24 hours. In the meantime, don't drive, drink alcohol, operate machinery or sign anything important.
You might see some blood in your pee but this is normal after TURBT. When you’re able to, drink plenty of fluids. Your nurse may use your catheter to flush your bladder out with fluid after your operation. You may also have a bag of fluid attached to the catheter, so that it continuously runs into your bladder and then out to the drainage bag. This is called continuous irrigation and helps to stop blood clots forming.
Your nurse will take your catheter out before you go home. At first, you might find it uncomfortable to pee, it may burn and you may need to go urgently or more often. This will usually get better in a few days but if not, see your doctor.
Before you leave hospital, your nurse will give you a follow-up appointment to talk about the results from your surgery. You’ll need to arrange for someone to drive you home. Try to have a friend or relative stay with you for the first 24 hours or so after your procedure.
Recovery for TURBT
You may feel tired and sleepy for a few days after your operation. If you need pain relief, you can take over-the-counter painkillers such as paracetamol. Always read the patient information leaflet that comes with your medicine and if you have any questions, ask a pharmacist for advice.
How fast you recover varies from person to person, but generally you’ll get better and return to your normal activities in about a week or two. Ask your surgeon when you can go back to work.
You may have some bleeding for up to three weeks after your operation. But if you have large blood clots and these stop you peeing, contact your surgeon straightaway, or go to your local accident and emergency department.
Up to one in 10 people develop a urine infection after TURBT, so it’s important to be aware of the symptoms. See a GP if you:
- feel that you need to pee urgently and often or when you’ve just been
- have pain or discomfort when you pee
- have smelly or cloudy and thick pee
- have a temperature above 37.5 °C
- feel generally unwell (ache all over, feel sick, tired and shiver or have cold sweats)
To make sure you fully recover and heal well at home:
- drink plenty of fluids – around 2 litres a day for the first two or three days
- take any antibiotics you were given after your operation
- try to get moving and get back to your normal activities as soon as you feel able to
- don’t drive until you feel comfortable doing so
Follow up after TURBT
Any further treatment you have after TURBT will depend on the risk of the cancer coming back and if it has spread into your bladder wall. Your surgeon and healthcare team will discuss this and meet with you to explain your options. They’ll talk you through the risks and benefits of further procedures and treatments.
Further treatments may include:
- regular cystoscopies to check that the cancer hasn’t come back (recurred) – a cystoscopy uses a tube with a telescope that goes up into your urethra to look inside your bladder
- another TURBT (within six weeks of the first one)
- a course of at least six more treatments of chemotherapy into your bladder
- an immunotherapy treatment called BCG (Bacille Calmette-Guerin) that will be put into your bladder
- surgery to remove your bladder
- radiotherapy or chemotherapy
Side-effects of TURBT
Side-effects are the unwanted but mostly temporary issues you may have after treatment. Possible side-effects of TURBT include:
- feeling tired and worn out
- pain and discomfort when you pee
- blood in your pee
You may also develop a urine infection.
There’s more information about infection, bleeding and what to look out for in our section on recovery from TURBT.
Complications of TURBT
Complications are problems that can occur during or after treatment. The possible complications or risks of any operation include an unexpected reaction to the anaesthetic or developing a blood clot in your leg (deep vein thrombosis).
Possible complications of TURBT include the following.
- Bleeding that doesn’t stop and blood clots – you may need an operation to stop the bleeding and remove blood clots. Large clots can stop you peeing. If you can’t pee, speak to your surgeon straightaway or go to accident and emergency.
- Small holes made in your bladder wall during the operation. This is called perforation. If this happens, your catheter might need to stay in for longer than usual. If the hole is large, you may need an operation to fix it.
All of the cancer might not be removed or the cancer might come back (recur) after TURBT. You’ll have regular check-ups after TURBT and if there’s any sign of cancer, you’ll be offered more treatment.
Alternatives to TURBT
TURBT is the main treatment for non-muscle invasive bladder cancer. Before and after TURBT, you may have more tests such as a CT scan or MRI scan, to see if the cancer has spread.
If the cancer has grown into the muscle of your bladder wall or has spread outside your bladder, your doctor will usually suggest other treatments. These could include an operation to remove all or part of your bladder, radiotherapy and chemotherapy. Ask your doctor for more information.
Chemotherapy
Radiotherapy
Did our Transurethral resection of bladder tumour (TURBT) information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Bladder cancer. BMJ Best Practice. bestpractice.bmj.com, last reviewed 6 December 2022
- Bladder cancer. Kaseb H, Aeddula NR. Statpearls publishing. www.ncbi.nlm.nih.gov, last updated 24 October 2022
- Transurethral telescopic resection of a bladder tumour. British Association of Urological Surgeons. www.baus.org.uk, published May 2022
- Types of bladder cancer. Cancer Research UK. www.cancerresearchuk.org, last reviewed 22 September 2022
- Transurethral resection of a bladder tumour (TURBT). Cancer Research UK. www.cancerresearchuk.org, last reviewed 14 October 2022
- Chemotherapy into the bladder. Cancer Research UK. www.cancerresearchuk.org, last reviewed 14 October 2022
- Venous thromboembolism in over 16s: Reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 13 August 2019
- Lucas A, Ward CW. Manual and continuous bladder irrigation. Best practices. Nursing 2022; 52(7):31–6. doi: 10.1097/01.NURSE.0000832324.25954.7b
- Bladder cancer surgery. American Cancer Society. www.cancer.org, last revised 30 January 2019



