Tonsillitis
- Dr Ade Adeniyi, Lead physician, Bupa
- Rachael Mayfield-Blake, Freelance Health Editor
Key points
- Tonsillitis is the inflammation of the tonsils, commonly caused by viral or bacterial infections.
- Tonsillitis is not contagious, but you can catch the infections that cause it.
- Tonsillitis symptoms include sore throat, high temperature, headache, and you may generally feel unwell.
- Tonsillitis usually goes way on its own within a week and can be managed with over-the-counter medicines. Other treatments are available if it doesn’t improve on its own.
What is tonsillitis?
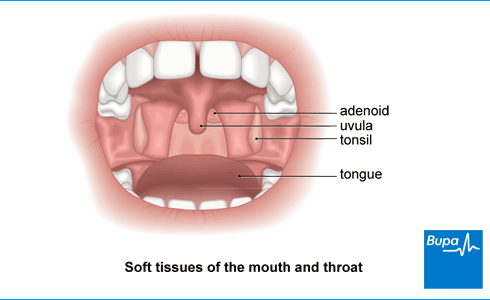
Tonsillitis means you have swollen (inflamed) tonsils. Your tonsils are two small round lumps of tissue at the back of your throat. You may have a sore throat, swollen tonsils, and pain when you swallow.
What causes tonsillitis?
Tonsillitis is a usually caused by a viral infection. Viruses causing tonsillitis include:
- the common cold virus
- the flu virus (influenza)
For around one in every three people, tonsillitis is caused by bacteria. Most bacterial tonsillitis is caused by streptococcus bacteria – specifically group A beta-haemolytic streptococcus bacteria. This is sometimes called ‘strep throat’.
Is tonsillitis contagious?
Tonsillitis itself isn’t contagious. Tonsillitis is often caused by cold and flu viruses that you can catch. You may also get tonsillitis if streptococcal bacteria affect your throat.
Symptoms of tonsillitis
If you have tonsillitis, you’ll probably have a sore throat. But a sore throat isn’t always due to tonsillitis.
Other symptoms of tonsillitis may include:
- pain when swallowing
- finding it hard to swallow
- earache
- high temperature (over 38°C)
- bad breath
- headache
- feeling generally unwell
- feeling sick or vomiting
- tummy pain
You may also notice that you have swollen tonsils and swollen glands in your neck. Your tonsils may be covered with a white coating or white flecks of pus.
Tonsillitis symptoms are similar to glandular fever symptoms. Glandular fever is a viral infection affecting mostly teenagers and young adults. Your GP may ask you to have a blood test if they suspect glandular fever.
Should I see my GP about a sore throat?
You don’t normally need to see a GP about a sore throat. Tonsillitis usually gets better within a week without needing to visit a GP. But if you’re worried about symptoms, or they don’t improve, see a GP.
Diagnosis of tonsillitis
To see if you have tonsillitis, a GP will examine your throat and tonsils. They may:
- use a bright torch to see the inside of your mouth better
- use a tongue depressor to push your tongue down gently
- feel around your neck to see if you have swollen glands
Under 18 GP Appointments
We now offer GP appointments for children under 18 via our remote video service (UK wide) and face to face appointments at selected centres. Please note that these appointments cannot be booked online so please call 0330 822 3072 for more information or to book. Lines are open Monday to Friday 8am to 8pm, Saturday and Sunday 9am to 5pm. We may record and monitor our calls. Available from £49.
To book or to make an enquiry, call us on 0800 665 577∧
Self-help for tonsillitis
Here are some ways to ease your tonsillitis symptoms at home:
- rest and take it easy for a few days
- drink plenty of fluids
- drink warm tea with honey, or cold and iced drinks
- gargle with warm salt water for throat pain
- try throat lozenges throat sprays to ease throat pain
Over-the-counter medicines such as paracetamol or ibuprofen can help ease a sore throat and high temperatures. Ask your pharmacist for advice.
Treatment of tonsillitis
Most people find that tonsillitis symptoms improve with self-help. Antibiotics won’t work if your tonsillitis is caused by a viral infection. A GP may give antibiotics for tonsillitis if:
- your symptoms are very bad, such as severe bacterial infection
- you could be prone to serious complications (see our section on complications)
GPs usually prescribe a 5 to 10-day course of penicillin. Tell your GP if you’re allergic to penicillin so they can give you a different antibiotic.
It’s important to take antibiotics properly. Complete the full course, even if you start to feel better. This helps to get rid of the bacteria and reduces the risk of antibiotic resistance (when antibiotics no longer work against the bacteria). Read the patient information leaflet carefully and see a pharmacist if you have questions.
Do I need surgery for tonsillitis?
A GP may refer you to an ear, nose, and throat (ENT) surgeon if you need your tonsils removed. This operation is called a tonsillectomy.
Some people get tonsillitis again and again. This is called recurrent tonsillitis and may be a reason to consider tonsil removal by tonsillectomy.
Your doctor may also recommend tonsillectomy if you’ve had abscess on your tonsils. This can be a complication of tonsillitis.
For children, your GP may recommend waiting for tonsillitis to get better on its own before considering surgery. As children get older, they are less likely to have tonsillitis.
Complications of tonsillitis
Tonsillitis usually doesn’t cause long-term problems. Severe infection or complications are more likely if you have a weak immune system. Complications are also more common in young children and older people.
Bacterial tonsillitis can sometimes lead to a build-up of pus on or around your tonsils. This is called a peritonsillar abscess or quinsy. This may cause very bad throat pain, often worse on one side. You may also have other symptoms, which include:
- earache
- high temperature
- difficulty swallowing due to pain
- difficulty opening your mouth
Peritonsillar abscess is more common in teenagers and young adults. But children can get it too. The abscess is usually treated with antibiotics and surgery to drain the pus.
Common childhood viruses [podcast]
Why children pick up so many viruses | Podcast | Listen in 18:31 minutes
In this podcast, Bupa GP, Dr Samantha Wild, to discuss common childhood viruses. Find out why children pick up so many viruses and illnesses during childhood, how to manage them and when to seek medical advice. They also discuss how the pandemic has affected general immunity, and whether the vaccination programme will extend to children.
Speaker 1: Alice Windsor
Hello and welcome to another episode of the Bupa Healthy Me Podcast. Today we're going to be talking about common childhood viruses. I'm Alice Windsor and I'm a specialist health editor at Bupa. I'm also a mother to two young children, Julius who's 3, and Molly, who's 6. I'm joined today by Doctor Samantha Wild, who is a Bupa GP. Hi, Samantha.
Speaker 2: Dr Samantha Wild
Hi, Alice.
Alice Windsor:
Hi. Thank you for joining me today.
Alice Windsor:
I think we'll start off by saying that it's very common for children to pick up viruses throughout childhood, as we know.
As a parent myself, I know just how easily and how often children could pick up things, may that range from a mild cold or to more severe bouts of illness such as tonsillitis or croup.
And some children I think are probably more prone to becoming more ill than others. I know my two children are very different in how often they pick up things.
Or some parents might say that their child has a weakness. They might be, you know, a child that always gets a temperature or always has a cough or a runny nose.
So I think it would be great to start by talking about why children get so many illnesses. Not all of them, but why throughout childhood, it's maybe more common and is this important for children to help them build a strong immune system?
Dr Samantha Wild:
Yes, it is. So, in the first few years of life, catching viruses is the best way for your child to build a strong and healthy immunity which will set them up for life. Babies are born with a very delicate immature immune system, which is why we recommend breastfeeding because we then pass on natural antibodies in our breast milk, and we also administer vaccines at that age too.
But as children are exposed to vaccines and viruses on a day-to-day basis in childcare, and then at school, and these are all spread by coughing, sneezing or breathing, as we know from the precautions, we've had to take now with COVID. But this is the way that they build up their immune systems. And so, the average school-age child can get sort of three to eight colds a year and two to three bouts of viral gastroenteritis.
And that is completely normal. So, although it may seem a lot, that's normal. It's also very common for children to get sick from one virus very quickly after recovering from another.
So, it might seem that they've been sick for weeks on end and as a GP, you often see these children being brought in and parents are worried, but they have actually recovered from one illness and you've not really noticed, and they very quickly caught another one again, but that frequency does drop as they get older and their immune system has then been built up.
Alice Windsor:
Definitely. Actually, I can relate to that. My youngest seemed to, in his first couple of years, really have, you know, one thing after another, so it's interesting that you say that.
Dr Samantha Wild:
Yeah, I remember that with my children too.
Alice Windsor:
Thinking about some of the most common childhood viruses that are out there in the community. You know, what are the most common viruses that children can bring home and are they things we should be worried about?
Dr Samantha Wild:
So, I think top of the list has got to be sort of common colds and coughs, which obviously we all know about. So, the common cold it’s usually a mild self-limiting viral upper respiratory tract infection. We know it's more frequent in the winter months.
Dr Samantha Wild:
But the main take home message is that antibiotics are ineffective. It is a virus, and so antibiotics do not work for that. So, on the whole, you know, children can be managed quite safely at home, keeping them well hydrated, giving them paracetamol if they need it.
And it's not unusual for them to sort of lose their appetite a little bit or maybe be a bit more sleepy.
Dr Samantha Wild:
But you know, we would always say use your parental instinct. So, mother, father, if you feel that the child is just not right, if they've got a very high fever, if they've got a rash, if they're very sleepy, if they're having difficulty breathing, that is when you need to see a GP.
But a normal cough or cold then obviously, you know, I think most parents would be happy to manage that at home.
Dr Samantha Wild:
It's using your common sense really. And using that sort of that gut instinct that we must never sort of-
Alice Windsor:
Take for granted.
Dr Samantha Wild:
Ignore, yeah, exactly. And I think this is where, you know, people have come unstuck in the past. You know, it's such an important instinct that parents have.
Alice Windsor:
Yeah. And I think from my point of view as well that one of the most worrying things I find when I've got a child at home who's is sick is what is the temperature. And I've actually, you know, what my youngest did have a febrile seizure at one point from his temperature just being too high.
Alice Windsor:
And I'd done everything right and sort of given them, you know, ibuprofen and paracetamol at the right time period. And it still happened. What advice could you give parents around temperatures at home because, you know, for me, I'm aware of how to manage them, but it's still a worry. And I am that parent that's got their thermometer in their ear quite often.
Dr Samantha Wild:
Yeah, yeah.
Oh, that's good. That's good. So just to sort of put it into perspective. So a normal temperature in a child is 36.4°.
And in general, we tend to say a high temperature is over 38°, although for a child sort of over 37.5° is quite high and high temperatures are really common and they often clear up themselves without needing any treatment.
And the reason your temperature does go up is because that's the way that the body fights off infection.
So you know it has an important function. But if a child is becoming distressed with that, that is when we say that you should give paracetamol or ibuprofen.
You don't need to use them together at the same time. Usually sort of use one or the other, but if the child isn't responding to the one, that's when you can use the other one. And so yeah, it's not just treating the temperature on its own, it's treating the fact that they may be distressed with it too.
As you said, very good to use a digital thermometer to actually ascertain what the temperature is. And then really important to give the child plenty of fluids. Make sure that they're not becoming dehydrated.
Give them a little bit of food if they want to, and then just keep an eye on things. If your child's younger, so three months or below, then a GP would want to see them. If their temperature was over 38°, a child at between three and six months, a temperature over 39°.
But for any other child, just if that temperature is lasting and it's just not settling, if they are becoming dehydrated or again just using those parental instincts - if there's any other sort of signs that just don't seem right.
So, we talk about floppy children. So, if children just seem like they've got no energy, if they're not responding to you, if they are breathing very quickly, obviously if there's a rash that you know, just doesn't look like a normal rash, all those sorts of reasons that you should get some medical advice.
Alice Windsor:
Yeah, brilliant. In terms of that, these sort of you know these things to look for that we really should be seeking medical help about, what would your best advice be? Would it be the first port of call to contact your GP surgery, or would you say always go for the 111 number for advice, and then what are those moments where it is always a 999 call?
Dr Samantha Wild:
I mean it completely depends what time of day it is. So, you know if you're within sort of normal working hours for a GP, try your GP surgery.
Obviously, things have been very different at the moment with COVID, so it will depend how your GP surgery is working at the moment and sometimes things are being directed still, through 111 to start with, if it's out of hours, I would definitely go 111 first.
Again, it's just using those instincts so you know if a child is really struggling to breathe, if they can't complete a sentence without stopping for breath, you're going to want to get them seen very quickly.
And so, you know, if if it's taking time, then it's going to be 999. You know other things to consider, or whether you've got transport to get to A&E.
Alice Windsor:
Yeah.
Dr Samantha Wild:
But at the moment, you know we are being encouraged not to just turn up at GP surgeries at hospitals as well because of COVID. So the advice is very different at the moment than it would normally be. So I think at the moment, yeah, you need to speak to someone and 111 is going to be the best, sort of quickest route to get some advice.
Alice Windsor:
Brilliant. I think as well, you know, it's just really important, like you say, to look at your child as a whole. And I think as a parent, you know your child better than anyone. So I think that is the best advice.
Dr Samantha Wild:
Definitely.
Alice Windsor:
OK. I've got a few questions that I've gathered from parents here that I thought we could just pick up on. I've got one here about viral rashes and when they come up and post-viral rashes, could you tell me a little bit more about those?
Because I think as a parent again, you know, my children have often had rashes alongside different illnesses and, you know, what we should be looking for in rashes and what is common, and when should we be seeking some medical advice?
Dr Samantha Wild:
So viral rashes, again, as you said, are really common in young children and they are usually called sort of reddish or pink spots over large parts of the body. So often on the chest and the back area.
And they're usually not sort of itchy or although some can be. Usually, like I say, it sort of covers that big area, but it's also symmetrical as opposed to just one side of the body, and you can usually tell that it's come, you know very quickly after or with a viral infection.
So, they might have a fever or runny nose or cough. Something else that you can tell you know is going on to sort of explain that.
So, you know, if a child is fairly well with it, if they've obviously just got a cough or a cold and the rash and we don't need to see them. When you do need to see a doctor is 1: if you did want a definite diagnosis of what it was, but also if the rash was causing them any pain at all.
A meningitis rash is obviously something that you know, we all worry about when we see a rash.
Alice Windsor:
Yeah. And is the glass test still something that we should do?
Dr Samantha Wild:
It definitely is. But just to say that a meningitis rash appears very late, usually with meningitis. So, you can usually tell that your child is very unwell before that rash appears, so we want to see a child before a rash appears there so, but yes, we use the tumbler test.
So, for people that don't know, that's if you use the bottom of a clear tumbler to gently apply pressure onto a rash, and it doesn't then go white or lighten up as you press on it and it sort of remains quite dark. And so what the rash that you get in meningitis is, it's bleeding under the skin.
So, it's very different to something that, you know, as you press it, it disappears. So that is, you know, definitely a medical emergency and you should then be calling 999.
Another reason you would call a GP if they had a rash, again, is if your child's very lethargic, if they are getting dehydrated so they're not feeding. If they have a fever, again, that isn't settling, as I said already, or if the rash just isn't settling after a few days as well.
Alice Windsor:
Brilliant. It's great advice. And the next question here is about a cough. As we all know with COVID going on, it's all about coughs at the minute, but someone has asked: my child has had a cough for a while a while after suffering a cold and at what point should you take them to the doctor? So, you know, how long do we keep them at home with this cough before we seek some advice.
Dr Samantha Wild:
OK. So again, you know, coughs are really common with colds and what happens is the mucus trickles down the back of the throat. Children are not very good at blowing their noses as adults are.
So, you know, that that's what stimulates the cough. If they're feeding, drinking, eating, breathing normally, you know, the cough is nothing to worry about.
So, although it can be sort of quite upsetting to hear them cough, you know that's the body's way of clearing the phlegm away from the chest or the back of the throat. And so that's completely normal. If it's been going on for longer than three weeks.
So that's when a GP would normally want to see them or, again, if they had a very high temperature, if they're, you know, if they feel hot and shivery, if they've got any difficulty with their breathing with it, again, if they can't talk in sentences, we would want to see them to make sure that it's not a chest infection.
And also, we'd want to see them if it carried on for, as I say, longer than the three weeks, if it's worse at night, if it's brought on by sort of running around, exertion, that could be a sign of asthma. So again, we would want to see them then.
So, it's if it's lingering and if it seems to be associated with any other symptoms, we would want to review them.
Alice Windsor:
And I think from my personal experience and it's not quite a question, but it's more of a topic of conversation. My youngest has had recurring croup since he was very little. We've had a few trips to A&E.
And it's amazing how many people, especially maybe of an older generation like my parents, you know, would say, get the steam going in the shower and and if he's got, you know, he's tight in the chest and it's sort of that croup cough, to use steam when actually the guidance has changed that.
Dr Samantha Wild:
Yeah, we don't recommend that. No, no. And yeah. So, you will still find that some doctors will sort of recommend that as well because they might not be sort of up to date. They used to think that the steam would loosen the mucus and make it easier to breathe. But there is very little evidence that it does do any good.
Alice Windsor:
Yes.
Dr Samantha Wild:
And I think some children were actually being scalded by the steam. So actually, you know, we've stopped recommending that now. The key with croup is to just keep children as calm as possible.
So not to panic, to keep them sat upright on your lap, as I'm sure you've probably found out, then, if you've been through this a few times, and you know a GP or hospital doctor, if they've ended up in hospital, we usually give a single dose of steroid medication if they need it and then that's what really works.
Alice Windsor:
It's very effective isn’t it.
OK. I've got a question here. It's sort of related to the pandemic. Should we be worried about the fact that children haven't been picking up the usual childhood infections this winter?
So, my son had chickenpox, hand, foot and mouth, and a host of other infections in his first year of school. But given COVID precautions, my daughter hasn't had any of these since starting reception. Should I be worried?
Dr Samantha Wild:
I think that's a really interesting question and I think time will probably tell with that. I think at the moment, as it's only been a year, and we don't necessarily get all those illnesses and build up all the immunity in that year, then you know it's unlikely to be an issue. And as children start to mix again in schools, then they're going to sort of – we’ll see that things start to spread again.
Also, as I said before, as children get older, their immune system is becoming more mature anyway, so it might be that they can fight off some of these illnesses themselves.
Yeah, it'll be interesting to see, but I think, you know, within the school environment and especially younger age children, obviously it's very difficult for teachers to ensure that there is any social distancing, you know, masks aren't necessarily worn in children of that age. So, I think, yeah, it'll start to spread as it always has done.
Alice Windsor:
Absolutely.
Great. And I think as well it'd be actually really good to talk about the flu vaccine. I’ve got a question here and it says, what is the effect of the flu vaccination on my child's long-term immunity?
Dr Samantha Wild:
OK. So obviously we have the flu vaccine every year and, you know, we're waiting to see really what's going to be happening with the COVID vaccine, because it looks like that's going to need to be, you know, fairly frequent as well.
So, the reason that we have the flu vaccine every year is because our immune protection that we're given from the vaccination declines with time, and also because the flu virus is constantly changing and, again, we've talked about this with COVID and the different variants that appear.
So, what they have to do is, you know, from the research, try and predict what might, what virus might be coming up next that needs to be protected. So that is why we are given the vaccination on a yearly basis.
As you know, the flu vaccine has been around for years. It's very safe. It's very effective. And so, you know, we would carry on having that yearly in conjunction with COVID vaccination as whatever they decide the time interval needs to be.
Alice Windsor:
Right. And I think it's why we, you know, we probably no one knows the answer to this at the moment. But do you think that the coronavirus vaccine is going to you know come down to children at some point this year or next year? Obviously, it's still a question mark.
Dr Samantha Wild:
Yes, I think it, yeah, I think it definitely will. I was speaking to a professor from London who was saying that he thought probably children over the age of 12, maybe to start with.
But yes, I think, you know, there's been a lot of talk about herd immunity and obviously if we can get that amongst children and we know that children don't really tend to suffer with it, but unfortunately, they do spread it, then it would seem to make sense I think, but I'm definitely not an expert in this area. So, I will leave that to the experts to decide.
Alice Windsor:
That's great, Sam. Thank you so much. We've covered some really brilliant questions today. It's such a vast topic area and children can get so many illnesses and viruses when they're young, but I think, you know, we've just touched on the surface today about how parents can deal with it and, you know, really when to go and see a doctor and when to ask for help.
I think that's a really important thing, when to seek that medical advice, and you know, we've got so much information on our Bupa website about, you know, different childhood illnesses, which is a great place for people to go if they need to, but we'll leave that for today and say thank you for joining.
Dr Samantha Wild:
Thank you.
Looking for prompt access to quality care?
With our health insurance, if you develop new conditions in the future, you could get the help you need as quickly as possible, from treatment through to aftercare.
To get a quote or to make an enquiry, call us on 0800 600 500∧
Adenoid and tonsil removal
Adenoid and tonsil removal is a procedure that involves taking away small lumps of tissue at the back of your nose and throat.
Antibiotics
Over-the-counter painkillers
Did our Tonsillitis information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg



