Tonsil and adenoid removal
Your health expert: Mr Jonathan Hughes, Ear, Nose and Throat Consultant
Content editor review by Pippa Coulter, Freelance Health Editor, July 2023
Next review due July 2026
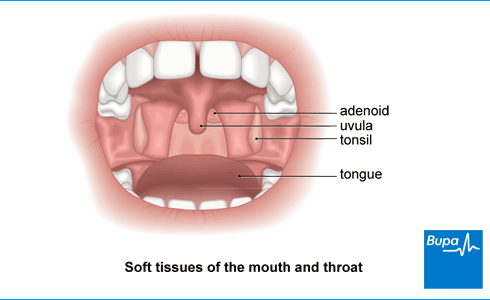
Your tonsils and adenoids are small lumps of tissue at the back of your throat. You may have an operation to remove your tonsils (a tonsillectomy) if you keep getting tonsillitis. You may have your adenoids removed (an adenoidectomy) if you have large adenoids that are causing problems. Adenoids and tonsils are often removed together (an adenotonsillectomy).
How an adenotonsillectomy is carried out
Adenotonsillectomy | Watch in 2:47 minutes
This animation shows how adenotonsillectomy is carried out. It is a procedure to remove your tonsils and adenoids. Having your tonsils and adenoids removed can be an effective treatment for recurrent tonsillitis, ear infections and nasal blockages.
This animation shows where the adenoids and tonsils are located and what happens if they become inflamed, which can happen as a result of an infection.
We then show how the operation called an adenotonsillectomy is performed.
The adenoids are two small lumps of tissue that lie at the back of your nose.
The tonsils are two oval lumps of tissue.
They sit on either side of the back of your mouth behind your tongue.
In children, the adenoids and tonsils can swell up and become inflamed.
This may happen as a result of a viral infection.
Now we show the inflammation.
People who suffer from frequent bouts of infected or inflamed adenoids or tonsils may have them taken out.
The operation to take out both the adenoids and the tonsils is called an adenotonsillectomy.
Your child will be given a general anaesthetic.
This means he or she will be asleep during the operation and feel no pain.
In this section, we show the anaesthetic being given.
Once the anaesthetic is taken effect, your child's mouth will be held open so the surgeon can see into the throat.
Specially adapted instruments are used to remove the adenoids and tonsils.
In this section, we show the tonsils and adenoids being removed.
The surgeon will press a gauze pad on the adenoid and tonsil area.
In this section, we show pressure being applied to stop the bleeding.
Sometimes the surgeon will close the wound and stop the bleeding with dissolvable stitches.
Sometimes a heated instrument is used to remove the tonsils and stop the bleeding.
This method is called diathermy.
There has been some question over the safety of diathermy because there is evidence that it increases the risk of bleeding after the operation.
Ask your surgeon for information on this technique and other possible complications of the operation.
This is the end of the animation.
About tonsil and adenoid removal
Your tonsils and adenoids are part of your immune system, which helps your body to fight infections. They become less important as you get older, and your body can still fight infections without them.
Tonsil removal
Tonsil removal (tonsillectomy) is a very common surgical procedure. It’s more frequently performed in children. But it’s a common operation in adults too.
There are several reasons why you may be offered an operation to remove your tonsils. These include if you’ve had repeated bouts of severe tonsillitis.
- seven times or more in the last year
- five times or more in each of the last two years
- three or more times in each of the last three years
- that are so severe, it stops you doing your usual activities including work or school
Your doctor may also recommend a tonsillectomy if you have an abscess on your tonsil (a peritonsillar abscess or quinsy). This can be a complication of tonsillitis.
If your GP thinks surgery may be an option for you, they will refer you to an ear nose and throat (ENT) surgeon. This is a doctor who specialises in identifying and treating conditions of your ear, nose and throat. The specialist will assess you to see whether surgery would help.
Adenoid removal
You may have your adenoids removed if you have large adenoids that are causing problems. If your adenoids are large, they can cause::
- a blocked nose, meaning you can only breathe through your mouth
- snoring, and sometimes sleep apnoea – where you get temporary pauses in your breathing, interrupting your sleep
- regular ear infections, leading to hearing loss or glue ear
An operation to remove your adenoids will help with these problems. Most operations are done in children because your adenoids usually shrink by the time you’re a teenager and will no longer cause problems.
You can have your adenoids removed on their own. But they are more often removed together with your tonsils, or at the same time as having grommets put in for glue ear. If you have your adenoids and tonsils removed at the same time, it’s called an adenotonsillectomy.
Your child’s GP will refer them to an ENT surgeon to discuss if adenoid removal might be an option.
Deciding on tonsil and adenoid removal
Surgery can stop you from getting tonsillitis and the problems associated with large adenoids. But it’s important to be aware that tonsil or adenoid removal can be a painful procedure and you’ll need some time to recover. Like any surgery, there is also a risk of complications. You’ll need to weigh up all the benefits and risks if you’re thinking about a tonsil or adenoid removal.
Your doctor will go through exactly what will happen before, during and after your procedure, and any pain you might have. It’s important to ask any questions you have so that you feel fully informed. You’ll be asked to sign a consent form if you decide to go ahead.
Preparation for tonsil and adenoid removal
Your nurse or surgeon will explain how to prepare for your procedure. You usually have a tonsil or adenoid removal as a day case in hospital. This means that you have the operation and go home the same day. You’ll need someone to arrange for someone to take you home afterwards.
You’ll also need to organise some time off work or school to recover after the operation. This will usually be a week for adenoid removal, and up to two weeks for tonsil removal.
If you get an infection such as a cold or chest infection in the week before your operation, it’s important to let your hospital know. It may be safer to delay your operation until you’ve recovered.
Your healthcare team will want to know if you have any other health conditions or allergies, as this may affect the surgery or recovery. You should also tell them about any medicines you’re taking. You may need to stop medicines that may increase bleeding (‘blood thinners’), such as Warfarin, before your operation.
You’ll have a tonsil or adenoid removal under general anaesthesia, which means you’ll be asleep during the operation. You’ll usually be asked to stop eating around six hours before a procedure under general anaesthesia. You can usually carry on taking clear fluids up to two hours beforehand. Follow your anaesthetist’s advice and if you have any questions, just ask.
Tonsil and adenoid removal procedure
Tonsils and adenoids are removed through your mouth – or sometimes your nose for adenoids. There isn’t any need for cuts or stitches to your skin.
Your surgeon will usually remove your tonsils or adenoids using one of the following methods.
- Dissection. This is the traditional method. Your surgeon will carefully cut out your tonsils and/or adenoids using surgical instruments. They’ll apply pressure to stop the bleeding and use dissolvable stitches or heat to seal the wound.
- Diathermy. Your surgeon will use heat from an electric current to remove or destroy your adenoids and/or tonsils. The surgeon may use suction with this method to remove adenoids.
- Coblation. This involves passing an electric current through a saline solution to remove your adenoid or tonsil tissue.
You’ll be taken to a recovery area or ward after your operation to be monitored while you wake up from the anaesthetic.
Aftercare for tonsil and adenoid removal
You’ll need to rest until the effects of the anaesthetic have worn off. The nurse will monitor you in the recovery room, before you return to the ward. You’ll need pain relief to ease any discomfort as the anaesthetic wears off. You’ll need to be able to eat and drink before you leave hospital. You’ll usually be able to go home after a few hours if you feel ready. Sometimes your surgeon may recommend you stay overnight.
Someone will need to drive you home, and also stay with you overnight.
Having a general anaesthetic affects everyone differently. You may find that you’re not so co-ordinated or that it’s difficult to think clearly. This should pass within 24 hours. In the meantime, don’t drive, drink alcohol, cook or use any machinery.
Tonsil and adenoid removal recovery
It will usually take around two weeks to recover from tonsil removal and a week to recover from having adenoids removed. But this can vary, so ask your surgeon what to expect. During this time, get plenty of rest at home. Keep away from crowded, smoky places and from people with coughs and colds.
Your throat will feel painful after a procedure to remove adenoids or tonsils. With an adenoid removal, it may be sore for a few days. With tonsil removal, it tends to get worse during the first five to seven days, before gradually getting better. Many people also find they get pain in their ears. Take regular painkillers to help manage your pain. Always ask your doctor or pharmacist for advice and read the patient information leaflet that comes with your medicine.
You should aim to eat normally after tonsil or adenoid removal. This will help to clean the back of your throat, reducing the chance of bleeding and infection. If it's uncomfortable to eat, you may find it helps to take a painkiller half an hour before a meal. Chewing gum may also help to ease the pain.
Your throat may look white as your throat lining heals and you might see some small threads in your throat. These will fall out by themselves. You’re likely to have bad breath after the surgery, while your throat is healing. This isn’t a problem on its own. But if you notice any bleeding from your throat, have a fever or are finding it difficult to control your pain, contact your hospital immediately.
Side-effects of having tonsils and adenoids removed
Side-effects are unwanted but mostly temporary effects you may get after having your tonsils or adenoids removed.
Common side-effects of tonsil and adenoid removal include:
- feeling sick – the hospital may give you anti-sickness medicine to help with this
- pain – this may go on for a week or two, but can be managed with painkillers
- earache
- a blocked nose after adenoids are removed – this usually clears within a week or so
- swelling at the back of your throat, and difficulty swallowing
- bad breath – drinking water and chewing gum may help
- a change in your voice – it may sound as if you’re talking through your nose after adenoid surgery – this should settle down in a few weeks
- a change in your taste – this usually gets better with time
Complications of having tonsils and adenoids removed
Complications are more serious, unexpected problems that may happen during or after the procedure. For tonsil or adenoid removal, complications may include the following.
- Bleeding after the operation. It’s normal to have a small amount of blood in your saliva on the first day after the operation. But if there’s a lot of blood, contact your hospital or go to your nearest A&E. You may need a second operation to stop the bleeding.
- Infection in your throat. Contact the hospital, your GP or go to A&E if you develop a fever after an adenoid or tonsil removal. You may need to take antibiotics.
- Damage to your teeth, lips or gums. This can be caused by the instruments used to keep your mouth open during surgery. It’s more likely to happen if one of your teeth is loose, capped or crowned.
- Adenoid regrowth. Although uncommon, it’s possible that your adenoids could grow back again after surgery.
- Nasal regurgitation. Although very rare, fluid may leak through your nose when you drink after adenoid surgery. This usually only happens if you have a weakness in the back of your throat. Your doctor will check this before you have surgery. Even if this does happen, it usually gets better by itself.
Alternatives to tonsil and adenoid removal
It’s your choice whether to have surgery to remove your adenoids or tonsils. If you decide against tonsil removal, you may continue getting frequent tonsillitis. You can take over-the-counter painkillers, such as ibuprofen or paracetamol to ease symptoms of tonsillitis. Your GP won’t usually prescribe antibiotics to treat tonsillitis, unless it’s very severe, or isn’t getting better on its own.
If you’re not sure whether surgery is the best option, your surgeon may suggest waiting for six months. Children’s tonsils usually shrink as they get older, so they may grow out of infections over time.
Adenoids also get smaller as children get older. So if you decide against having adenoid surgery for children, you’re likely to find any problems get better in time.
You should try to eat normally after having your tonsils out. Your throat is likely to hurt, but if you eat and drink, normally it will help your throat to heal more quickly. If you’re finding this difficult, take a painkiller half an hour before you’re due to eat. See our tonsil and adenoid removal recovery section for more information.
If your child’s tonsils and adenoids are removed, it may help their snoring. But surgery is usually only recommended if they also have obstructive sleep apnoea or tonsillitis that keeps coming back. Children’s tonsils and adenoids shrink as they get older, so their snoring may improve on its own. See our about tonsil and adenoid removal section to find out more.
Tonsil or adenoid removal can be a painful procedure. You should expect some pain for at least a few days after adenoid surgery, and for a week or so after tonsil removal. Taking painkillers regularly while you’re recovering will help to keep the pain under control. See the tonsil and adenoid removal recovery section for more information.
Some side-effects are to be expected after surgery to remove your tonsils or adenoids. These include some pain, swelling, difficulty swallowing and bad breath. These will pass with time. The most common serious complication is bleeding after the operation. A second operation may be needed to stop this. Read our side-effects of having tonsils and adenoids removed section and complications of having tonsils and adenoids removed section to find out more.
Acute middle ear infection in children
If you’re a parent you’ll probably know that middle ear infections are common in children, and unfortunately they’re often painful.
Tonsillitis
Tonsillitis is inflammation of your tonsils, usually as a result of an infection. The infection may be viral or, less commonly, bacterial.
Over-the-counter painkillers
Glue ear
Sleep apnoea
Did our Tonsil and adenoid removal information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Tonsil and adenoid anatomy. Medscape. emedicine.medscape.com, updated 20 July 2015
- Sore throat – acute. NICE Clinical Knowledge Summaries. cks.nice.org.uk, revised January 2023
- Commissioning guide: tonsillectomy. ENT UK. www.entuk.org, published January 2021
- ENT. Oxford handbook of operative surgery. Oxford Academic. academic.oup.com, published online May 2017
- Adenoid surgery. ENT UK. www.entuk.org, published July 2022
- Tonsillectomy (taking out your tonsils) because of repeated infections. ENT UK. www.entuk.org, published July 2022
- Tonsillitis. Patient. patient.info, last updated 1 February 2023
- Keltie K, Donne A, Daniel M, et al. Paediatric tonsillectomy in England: A cohort study of clinical practice and outcomes using Hospital Episode Statistics data (2008–2019). Clin Otolaryngol 2021; 46(3):552–61. doi: 10.1111/coa.13707
- Wilson JA, O'Hara J, Fouweather T, et al. Conservative management versus tonsillectomy in adults with recurrent acute tonsillitis in the UK (NATTINA): a multicentre, open-label, randomised controlled trial. Lancet. 2023; 401(10393): 2051–59. doi: 10.1016/S0140-6736(23)00519-6
- Otitis media with effusion. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised June 2021
- Obstructive sleep apnoea syndrome – Management. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised November 2021
- Good surgical practice. The Royal College of Surgeons, www.rcseng.ac.uk, published September 2014
- Caring for someone recovering from a general anaesthetic or sedation. Royal College of Anaesthetists, www.rcoa.ac.uk, published November 2021
- General surgery. Oxford handbook of operative surgery. Oxford Academic. academic.oup.com, published online May 2017
- Surgery. Oxford handbook of adult nursing. Oxford Academic. academic.oup.com, published June 2018
- Suction diathermy adenoidectomy. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 16 December 2009
- Anaesthesia explained. Royal College of Anaesthetists, www.rcoa.ac.uk, published January 2021
- After your child's tonsil surgery: tips for parents. ENT UK. www.entuk.org, published 22 September 2022
- Adult tonsil surgery. ENT UK. www.entuk.org, accessed 19 January 2022



