Angioplasty of the leg arteries
- Professor Alok Tiwari, Consultant Vascular and Endovascular Surgeon
An angioplasty is a keyhole procedure to open up narrowed or blocked blood vessels (arteries). You can have an angioplasty in your leg arteries to treat a condition called peripheral arterial disease and improve blood flow to your legs. It’s called a femoral angioplasty when it’s below your groin (in your legs).
About angioplasty of the leg arteries
Your doctor may offer you an angioplasty procedure in your legs if you have pain in your legs when you walk due to peripheral arterial disease. This is a condition in which the arteries in your legs narrow or become blocked, which reduces the blood supply.
A specialist doctor will carry out the procedure. This may be a radiologist (a doctor who specialises in imaging techniques), a heart specialist or a vascular surgeon.
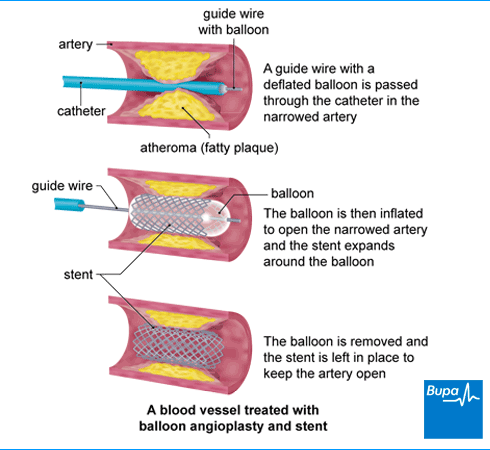
In an angioplasty, your doctor will inflate a balloon inside your narrowed artery to open it up (balloon angioplasty). It’s a minimally invasive procedure (a keyhole procedure), which means it doesn’t involve surgery. Instead, it’s done by placing a very fine tube in your artery, and sometimes, leaving a very small wire mesh (stent) to keep the artery open.
If your doctor thinks you could benefit from an angioplasty, they’ll go through exactly what to expect. This includes what happens before, during and after the procedure and any risks involved. If you’re happy to go ahead, you’ll need to sign a consent form.
Preparing for angioplasty of the leg arteries
Your doctor will explain how to prepare for your angioplasty procedure in your legs. You may need to stop taking certain medicines before your procedure. An angioplasty will involve having a local anaesthetic and an X-ray dye to show up your blocked arteries. Tell your doctor if you have an allergy to anaesthetics or any X-ray dye. Also let them know about any medical conditions you have or if there’s any possibility you might be pregnant.
You may need to have a pre-admission appointment a few weeks before your procedure. This is to check that you’re fit and well enough for it to go ahead. It’s also a good opportunity to ask any final questions you may have.
You can usually go home the same day as having an angioplasty, but there’s a chance you may need to stay in hospital overnight. An angioplasty is usually done under local anaesthesia and sometimes sedation. This means the area where you have the procedure will be numb. If you have a sedative, you may feel sleepy. You might need to stop eating and drinking for about four hours before the procedure. Follow any advice your hospital gives you.
The angioplasty of the leg arteries procedure
Angioplasty usually takes about an hour to perform, but it can be longer depending on how complex your procedure is. Your hospital will give you a gown to change into and ask you to lie flat on your back on an examination table.
Your doctor will clean the area of skin where they’ll perform the procedure (usually your groin) and numb it with local anaesthetic. They’ll place a small needle through your skin to access your artery, before replacing this with a small tube (catheter). Your doctor can inject a dye (contrast medium) into the tube and take X-rays to show up the narrow or blocked blood vessels.
Your doctor will pass a thin guidewire through to the affected section of your artery. They’ll insert a catheter that contains a deflated balloon over this. Once it’s in place, your doctor will inflate the balloon to open up your artery. This might feel a bit uncomfortable but it shouldn’t be painful. They’ll deflate the balloon after a minute or two, before they remove it. Your doctor will take X-rays to check whether your artery has stayed open. If necessary, they may insert a very small wire mesh tube called a stent into your artery to keep it open.
At the end of the procedure, your doctor will remove the catheter. Your doctor or nurse will apply pressure to the area where the catheter was inserted for around 10 minutes, until any bleeding stops. Sometimes, they might use a device to seal the hole in your artery instead.
Looking for prompt access to quality care?
With our health insurance, if you develop new conditions in the future, you could get the help you need as quickly as possible, from treatment through to aftercare.
To get a quote or to make an enquiry, call us on 0800 600 500∧
Aftercare following angioplasty of the leg arteries
After your angioplasty procedure, you'll need to lie flat down flat for a while – sometimes for several hours. This is to stop the artery from bleeding.
It’s likely to feel a bit sore around the area where the tube was inserted, and you may have some bruising. You can take painkillers to manage this.
Your doctor will usually discuss the results of the treatment with you before you go home. They may prescribe you some medicines to help prevent blood clots and avoid future problems.
When you’re ready to go home, you’ll need someone to take you. If you’ve had a sedative, you might find that you’re not so coordinated or that it’s difficult to think clearly for the first 24 hours. In the meantime, don’t drive, drink alcohol, operate machinery or make any important decisions. It’s a good idea to have someone to stay with you overnight while you recover.
Recovering following angioplasty of the leg arteries
Take it easy while you recover from an angioplasty procedure. In terms of the angioplasty recovery time, you’ll usually be able to walk around after the first day. It might take about a week to get back to your usual activities, including returning to work. You’ll need to be able to perform an emergency stop before you’re safe to drive. Check with your doctor about your own individual circumstances.
Contact the hospital if you have any concerns about your leg when you get home. For instance, if it becomes red and swollen, it might be a sign of an infection.
There are some signs that the blood supply to your leg has become blocked. These include your leg becoming:
- cold
- pale
- painful
- numb
- immobile (you can’t move your leg)
Contact the hospital urgently or call an ambulance if this happens. See the Complications section for more information.
Leg angioplasty is often successful but it’s possible that your artery may become narrow or blocked again over time. This is known as restenosis or re-occlusion. See your doctor if you develop more leg pain after an angioplasty. You may need to have another angioplasty, or a bypass procedure instead.
If you make some lifestyle changes after your operation, it can reduce the risk of your arteries getting narrow or blocked again and you needing more treatment. These include the following.
- Stop smoking if you smoke.
- Eat a healthy, balanced diet, low in saturated fat.
- Keep active. Choose something you enjoy and build activity into your day-to-day life.
- Keep to a healthy weight.
- Taking any medicines you’ve been prescribed to reduce your cholesterol, treat high blood pressure, and to prevent blood clots.
Complications of angioplasty of the leg arteries
Complications are problems that may occur during or after your angioplasty. Complications of angioplasty of the leg arteries include the following.
- You may bleed at the site where your artery was pierced with the catheter. This may cause a blood clot, called a haematoma. Occasionally, you may need an operation to remove the haematoma and repair the artery.
- Your artery can be damaged or torn during the procedure. This is very rare, but if it happens, you may need to have an operation to repair it.
- It’s possible for your artery to become completely blocked during or soon after the procedure. If this happens, you will need another procedure to re-open the artery.
- You might have an allergic reaction to the dye used during the procedure. For most people, this is just a minor reaction, but very rarely it could be a more severe reaction that will require urgent treatment.
- The site where the catheter was inserted may become infected. Signs of an infection include your leg becoming red and swollen, and possibly a foul-smelling discharge or bleeding from the puncture site. Seek urgent medical advice if this happens.
- It’s possible for the wires and tubes used in the procedure to dislodge fragments of the blockage as they’re being passed through. These may go on to cause blockages elsewhere and you may need another procedure to remove these fragments.
- The stent (if you had one put in) may break and need to be replaced.
Sepsis (adults)
Sepsis is a life-threatening complication that can develop if you get an infection. Sepsis is a medical emergency. Call 999 or go to A&E immediately if you have any of the following symptoms.
- Slurred speech, confusion, difficulty making sense.
- Extreme shivering or muscle pain.
- Passing no pee (urine) during a day.
- Severe difficulty breathing, feeling breathless, or breathing very fast.
- It feels like you’re going to die.
- Skin changes, such as your skin looking blue, pale or blotchy, or a rash that doesn’t fade when you roll a glass over it.
Alternatives to angioplasty of the leg arteries
Your doctor will usually suggest you try other measures for peripheral arterial disease before you consider angioplasty. These include:
- stopping smoking
- managing your diet and weight
- taking any medicines you have to control cholesterol, blood pressure and diabetes, and to stop blood clotting
- an exercise programme
If these measures don’t improve your symptoms, your doctor may refer you to a specialist, to assess whether an angioplasty may help. Sometimes, your doctor may be able to prescribe some medicines instead of referring you for angioplasty.
If an angioplasty isn’t a suitable option for you, another option is bypass surgery. This is a procedure that creates another way for blood to get around a blocked artery in your leg.
It’ll take some time to recover from a leg angioplasty. Most people feel able to get back to work or their usual activities after about a week. However, this can be different for everyone. It may take longer, especially if you develop any complications. Ask your doctor when it’s a good time for you to go back. See our recovery following angioplasty of the leg arteries section for more information.
A leg angioplasty is successful in up to 8 in 10 people who have the operation. Some of these people go on to develop further blockages in their legs. If this happens, you may need another angioplasty, or an alternative procedure.
There are various treatments for blocked arteries in the legs. These may include stopping smoking, managing your diet and weight and completing an exercise programme. If these don’t help, you may be offered an angioplasty operation to open up your artery. If an angioplasty isn’t a suitable option for you, another option is bypass surgery. This is a procedure that creates another way for blood to get around a blocked artery in your leg. See our alternatives to angioplasty of the leg arteries section for more information.
Yes, you’ll be awake during a leg angioplasty procedure. It’s usually done under local anaesthesia and sometimes sedation. This means the area where you have the procedure will be numb. If you have sedation, you may feel sleepy but you’ll still be awake. See our preparation for angioplasty of the leg arteries section for more information.
There are some risks of putting a stent into an artery in the leg. These include the stent getting blocked, or it may break. The site where the catheter was inserted may become infected. And it’s possible for the wires and tubes used in the procedure to dislodge fragments of the blockage as they’re being passed through. See our complications of angioplasty of the leg arteries section for more information.
Tips for a healthy and well-balanced diet
A healthy, well-balanced diet involves eating foods from a variety of food groups to get the nutrients that your body needs to function.
Effects of smoking
Other helpful websites
Discover other helpful health information websites.
Did our Angioplasty of the leg arteries information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Angioplasty and stent insertion. British Society of Interventional Radiology. bsir.org, published 2020
- Peripheral arterial disease. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised July 2022
- Majeed H, Chowdhury YS. Percutaneous transluminal angioplasty and balloon catheters. StatPearls Publishing. ncbi.nlm.nih.gov/books, last updated 14 September 2022
- Zemaitis MR, Boll JM, Dreyer MA. Peripheral arterial disease. StatPearls Publishing. ncbi.nlm.nih.gov/books, last updated 23 May 2023
- Sedation explained. Royal College of Anaesthetists. rcoa.ac.uk, reviewed June 2021
- About anaesthesia and perioperative care. Royal College of Anaesthetists. rcoa.ac.uk, accessed 18 March 2024
- Peripheral vascular stent insertion technique. Medscape. emedicine.medscape.com, updated 14 February 2022
- Angiography. MSD Manual Professional Version. msdmanuals.com, reviewed/revised November 2023
- Sepsis. Patient. patient.info, last updated 21 February 2024
- Suspected sepsis: Recognition, diagnosis and early management. National Institute for Health and Care Excellence (NICE), 31 January 2024. nice.org.uk
- About sepsis. The UK Sepsis Trust. sepsistrust.org, accessed 18 March 2024
- Peripheral arterial disease: diagnosis and management. National Institute for Health and Care Excellence (NICE), 11 December 2020. nice.org.uk
- Peripheral arterial bypass graft. Vascular Society. vascularsociety.org.uk, accessed 27 March 2024
- Rockley M, Jetty P, Wells G. Physiologic perfusion monitoring methods during endovascular revascularization for atherosclerotic peripheral arterial disease: Protocol for a systematic review. Syst Rev 2020; 9(1):107. doi: 10.1186/s13643-020-01357-y
- Rachael Mayfield-Blake, Freelance Health Editor



