Echocardiogram
- Professor Mark Westwood, Consultant Cardiologist
- Rachael Mayfield-Blake, Freelance Health Editor
An echocardiogram is a test that checks the structure of your heart and how well it’s working. It uses sound waves (ultrasound) to create moving images. An echocardiogram test can help diagnose problems with your heart – for example, an injured heart muscle or heart valve disease. It can also monitor how well your heart works over time.
About an echocardiogram
During an echocardiogram procedure, sound waves reflect off the muscles and tissues in your heart to create a moving image on a screen.
There are different types of echocardiogram.
- A transthoracic echocardiogram is the most common type of echocardiogram. It involves moving an ultrasound probe over your chest to get pictures of your heart.
- A stress echocardiogram checks what happens when your heart has to work harder than normal. Stress can be created through exercise or by taking medicines.
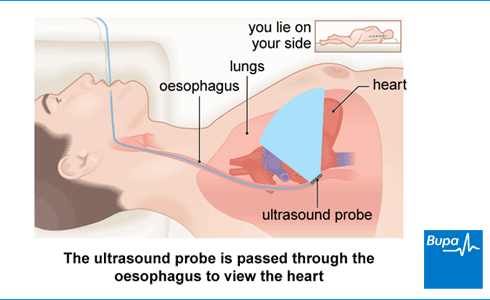
- A transoesophageal echocardiogram. A doctor or sonographer will pass an ultrasound probe into your oesophagus (the pipe that goes from your mouth to your stomach). This enables them to take pictures from behind your heart.
Your echocardiogram will usually be done by a sonographer (who is trained to do ultrasounds) or a cardiologist (a specialist heart doctor). You may have an echocardiogram while you’re lying down or while you’re doing exercise (a stress echocardiogram). Sometimes, you may need to have more than one echocardiogram to monitor changes in your heart over time.
You can have an echocardiogram at any age; even newborns and unborn babies can have an echocardiogram.
Preparation for an echocardiogram
You usually have an echocardiogram as an outpatient at hospital. This means you have the test and go home on the same day. If you are going to have a sedative, arrange for a friend or family to drive you home.
Your doctor or sonographer will explain how to prepare for your echocardiogram. You can ask to have a friend or family member with you during the procedure if you’d like. Or you can ask for a healthcare chaperone, although you may need to let your hospital know in advance if you want to do this. If you’re having a transoesophageal echocardiogram, you’ll need to remove any dentures or dental plates that you have before your procedure.
Medicines
Normally, you can take your usual medicines before an echocardiogram. But if you’re having a stress echocardiogram, you’ll usually need to stop taking beta-blockers or calcium-channel blockers for two days before your test. This is because these medicines change how your heart works. If you don’t stop taking them, you may need to re-arrange your appointment and have your echocardiogram another time.
If you’re having a transoesophageal echocardiogram, let your hospital know if you’re taking any medicines that help to prevent your blood clotting – for example, warfarin. Also let your doctor know if you have any problems with swallowing because you may need an alternative procedure.
Ask your doctor if you need to stop taking your medicines before your echocardiogram.
Eating and drinking
You can usually eat and drink normally before a transthoracic echocardiogram, it won’t affect the test. But if you’re having a stress echocardiogram using medicines, you must stop eating two hours before your test. You may still drink water.
If you’re having a transoesophageal echocardiogram, you won’t be able to eat or drink anything for six hours before the procedure.
Your doctor or hospital will give you more information and some specific instructions for your procedure. Check with them if you’re unsure about anything.
The echocardiogram procedure
Transthoracic echocardiogram
A transthoracic echocardiogram usually takes around 30 to 40 minutes.
You’ll need to undress to your waist and put on a hospital gown that opens at the front. When you’re in the procedure room, you’ll lie on your left-hand side on the bed, with your left arm behind your head. Your doctor or sonographer will put stickers on your chest and connect them to a machine to monitor your heart rate during the test.
Your doctor or sonographer will put a clear gel on your chest. They’ll then press the probe firmly against your chest and move it around. As they move the sensor, it will send out sound waves and pick up the returning echoes reflected from the different parts of your heart. Pictures of your heart will be displayed on a screen. These pictures are constantly updated, so the scan can show your heart beating.
Most people don’t find an echocardiogram painful, but if you are uncomfortable, let your sonographer or doctor know.
You may be able to hear some noise during the echocardiogram. This is the sound of the machine recording the blood flowing through your heart valves. It’s nothing to worry about.
Stress echocardiogram
A stress echocardiogram checks what happens when your heart has to work harder than normal so it’s under stress. Your doctor or sonographer may ask you to do some exercise or give you some medicines for this test. They’ll monitor your blood pressure and heart rate regularly during the test, which usually lasts for 30 to 45 minutes.
- In an exercise stress echocardiogram, your doctor or sonographer may ask you to walk on a treadmill or pedal on a stationary exercise bike. The exercise will be gentle at first but may keep getting harder. They may take pictures of your heart while you exercise and/or immediately afterwards.
- In a pharmacological stress echocardiogram, your doctor will give you some medicines that mimic the effects of stress. These medicines make your heart beat faster and harder. You’ll usually have these medicines through a drip into a vein in your arm. Your doctor may also inject a contrast medium into your vein (see below) so they can see your heart more clearly. Once your heart has been made to work hard enough, your doctor will stop giving you the medicine. Your sonographer will keep taking pictures of your heart until the effects of the stress medicine have worn off.
Contrast echocardiogram
A contrast echocardiogram is when a doctor injects a dye into a vein in your arm. The dye helps to show your heart more clearly. You might have this if you had an echocardiogram and the images weren’t very clear.
Bubble echocardiogram
In a bubble echocardiogram (sometimes called a bubble study), your doctor will inject a saline contrast agent into your vein during your echocardiogram. This is salt water that contains tiny bubbles, which help to show blood flowing through your heart more clearly. A bubble echocardiogram helps to show if there is a hole in your heart.
Transoesophageal echocardiogram
A transoesophageal echocardiogram usually takes about 20 minutes. Your doctor may give you a sedative, which will make you feel sleepy but you’ll be awake.
Your doctor or sonographer will spray a local anaesthetic into the back of your throat to numb it. They’ll then ask you to lie on your left side.4 They’ll put the ultrasound probe into your mouth and ask you to swallow so they can pass it into your oesophagus. The test isn't painful but it may feel uncomfortable when the probe passes down the back of your throat. You’ll still be able to breathe normally throughout.
The probe will send out sound waves and pick up the returning echoes. These are converted into pictures of the inside of your heart.
Uses of an echocardiogram
Your doctor may recommend you have an echocardiogram test to check your heart valves, heart chambers and large blood vessels. The test will build a detailed picture of your heart. This could be to check for any injuries to your heart muscle or to check for changes that may happen as you get older.
An echocardiogram can check for lots of heart problems, including:
- an injury to your heart muscle because of a heart attack
- a blood clot in your heart
- damaged heart valves
- congenital heart disease (an abnormality you were born with)
- endocarditis (an infection in your heart)
- pericardial effusion (fluid around your heart)
- heart failure (when your heart isn’t pumping blood properly)
- enlarged heart chambers
- problems with your aorta (the main artery that carries blood away from your heart)
If you have any questions about why you need an echocardiogram, ask your doctor.
Aftercare for echocardiogram
If you have an echocardiogram as an out-patient procedure, you’ll be able to go home straight after your test. If you didn’t have a sedative, you should be able to drive home and carry on with your usual day-to-day activities.
If you had a transoesophageal echocardiogram and were given a sedative, you’ll need to rest for two to three hours. Once you’re fully recovered, you’ll be able to go home. Ask friends or family to drive you home because it can take up to 24 hours for the effects of a sedative to wear off. You might feel a bit unsteady after having a sedative and may find it hard to think clearly. This should pass within 24 hours. In the meantime, don’t drive, drink alcohol, operate machinery or make any important decisions.
If you were given medicines to increase your heart rate in a pharmacological stress echocardiogram, you may need to rest for about 20 minutes after the test. This will make sure the effects of the medicines have completely worn off before you leave the hospital. It’s best not to drive that day – ask someone to drive you home.
Getting your echocardiogram results
Your sonographer or doctor may talk you through your echocardiogram results straight after your procedure. But they’ll usually send the results to the doctor who sent you for the test. Your doctor will discuss your results with you at your next appointment. Sometimes, you may have an appointment with your doctor straight after your echocardiogram.
Don’t worry if your doctor or sonographer can’t give you the results straight away. Your results may need to be analysed first. Your doctor may also need to consider your medical history and the results of any other tests you’ve had.
Your doctor will let you know if you need any treatment based on the results of your echocardiogram and any other tests you had. Your echocardiogram may rule out a problem with your heart or it may show you need further tests or treatment. Your doctor will talk you through the next steps.
Worried about your heart health?
Get a picture of your current health and potential future health risks with one of our health assessments.
To book or to make an enquiry, call us on 0800 665 577
Side-effects of an echocardiogram
Echocardiograms don’t usually cause any side-effects. But if you had a transoesophageal echocardiogram, you may have a sore throat for a day or two. Your throat may also feel bruised or bleed a little.
Having an exercise stress echocardiogram is the same as doing some vigorous exercise at home. You may feel some mild discomfort in your chest or feel breathless or dizzy.
During a pharmacological stress echocardiogram, you are given some medicines and you may feel your heart beating harder and faster. You may feel some discomfort in your chest and be a bit breathless. These medicines can also make you feel a bit sick or dizzy. These feelings should go away once your doctor stops giving you the stress medicines.
But if you’re still feeling sick or dizzy after your test, let your doctor or sonographer know.
Complications of an echocardiogram
A standard transthoracic echocardiogram is a safe procedure and doesn’t cause any complications.
A stress echocardiogram can sometimes cause heart rhythm problems and chest pains. Your sonographer or doctor or will monitor you carefully throughout.
If your sonographer or doctor has used contrast agent or medicines during the echocardiogram, there’s a very small chance you may have an allergic reaction.
If you had a transoesophageal echocardiogram, complications can include a very small risk of damage or a tear to your oesophagus.
Alternatives to an echocardiogram
Alternatives to a transthoracic echocardiogram include the following.
- Cardiac magnetic resonance imaging (MRI) scan. MRI uses powerful magnets, radio waves and computers to create detailed images of your heart.
- Cardiac computer tomography (CT) scan. This uses X-rays to create a three-dimensional image of your heart and is useful for checking for narrowed coronary arteries.
- Radionuclide test. In this test, your doctor will inject a harmless, radioactive substance into your body and then take pictures of your heart. The radioactive substance shows up as it travels through your heart so your doctor can see your blood flowing and how well your heart’s working.
Ask your doctor to talk through the options with you and discuss which test is best for you.
A doctor would order an echocardiogram to check the structure of your heart. They’ll check your heart valves, heart chambers and large blood vessels to see if they’re still working well. The test can help your doctor to diagnose heart problems, such as any muscle injury after a heart attack or an infection in your heart.
For more information, see our section on uses of an echocardiogram.
If your routine ultrasound scans show a potential problem with your baby’s heart, you’ll be offered a fetal echocardiogram. Your midwife may also offer you this test if you have a family history of congenital heart disease (congenital means you’re born with a problem). A fetal echocardiogram can show the structure of your baby’s heart and how well the blood is flowing through it.8 This will help to show if your baby needs any treatment.
An echocardiogram can diagnose a number of heart problems. These include:
- a blood clot in your heart
- severe heart failure (when your heart isn’t pumping blood properly)
- pericardial effusion (when you have fluid around your heart)
- leaky or narrowed heart valves
For more information, see our section on uses of an echocardiogram section.
There isn’t usually anything you shouldn’t do before a transthoracic echocardiogram. But if you’re having a stress echocardiogram (using exercise or medicines), stop taking beta-blockers or calcium-channel blockers for two days before your test. And if you’re having a stress echocardiogram induced by medicines, don’t eat for two hours before your test. If you’re having a transoesophageal echocardiogram, stop eating and drinking 6 hours before your procedure.
For more information, see our section on preparing for an echocardiogram.
Yes, an echocardiogram can show heart failure (when your heart isn’t pumping blood properly). An echocardiogram will measure the amount of blood that your heart pumps out each time your heart beats. If this is less than normal, your doctor will use this and other test results to diagnose heart failure
In a transthoracic echocardiogram, your doctor or sonographer will move an ultrasound probe over your chest to take the scan. In a transoesophageal echocardiogram, they’ll pass the probe down your oesophagus, which is close to the back of your heart. This can produce clearer pictures than a transthoracic echocardiogram so it’s more helpful for your doctor to diagnose certain problems.
Electrocardiogram (ECG)
An electrocardiogram (ECG) is a test that can record the rhythm and electrical activity of your heart to find out if it’s healthy.
Heart attack
Heart valve disease
Heart valve disease is when one or more of your heart valves become diseased or damaged, affecting the way that blood flows through your heart.
Transoesophageal echocardiogram
Did our Echocardiogram information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Omerovic S, Jain A. Echocardiogram. StatPearls Publishing. www.ncbi.nlm.nih.gov, last updated 24 July 2023
- Heart tests. National Heart Lung and Blood Institute. www.nhlbi.nih.gov, last updated 24 March 2022
- Echocardiography. MSD Manuals. msdmanuals.com, reviewed/revised December 2023
- Exercise stress echocardiography. British Society of Echocardiography. www.bsecho.org, accessed 21 February 2024
- Pharmacological stress echocardiography. British Society of Echocardiography. www.bsecho.org, accessed 21 February 2024
- Transoesophageal echocardiography. British Society of Echocardiography. www.bsecho.org, accessed 21 February 2024
- Transthoracic echocardiography. British Society of Echocardiography. www.bsecho.org, accessed 21 February 2024
- Echocardiogram. British Heart Foundation. www.bhf.org.uk, last reviewed September 2023
- Echocardiography. Medscape. emedicine.medscape.com, updated 7 January 2020
- Contrast echocardiography. British Society of Echocardiography. www.bsecho.org, accessed 21 February 2024
- Sedation explained. Royal College of Anaesthetists. www.rcoa.ac.uk, reviewed June 2021
- McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2021; 42(36):3599–726. doi: 10.1093/eurheartj/ehab670
- Cardiac imaging tests. MSD Manuals. msdmanuals.com, reviewed/revised December 2023
- Radionuclide imaging of the heart. MSD Manuals. msdmanuals.com, reviewed/revised December 2023
- Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, et al. 2018 ESC guidelines for the management of cardiovascular diseases during pregnancy: The Task Force for the management of cardiovascular diseases during pregnancy of the European Society of Cardiology (ESC) Eur Heart J 2018; 39(34):3165–241. doi: 10.1093/eurheartj/ehy340
- Fetal echocardiogram test. American Heart Association. www.heart.org, last reviewed 18 September 2023
- Intrapartum care: Existing medical conditions and obstetric complications. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published 28 February 2020
- Pericardial effusion. Patient. patient.info, last updated 23 November 2022
- Heart failure. British Heart Foundation. www.bhf.org.uk, last updated August 2022



