Anterior cruciate ligament (ACL) injury
Your health expert: Dr Arjuna M Imbuldeniya, Consultant Trauma and Orthopaedic Surgeon
Content editor review by Julia Ebbens, March 2023
Next review due March 2026
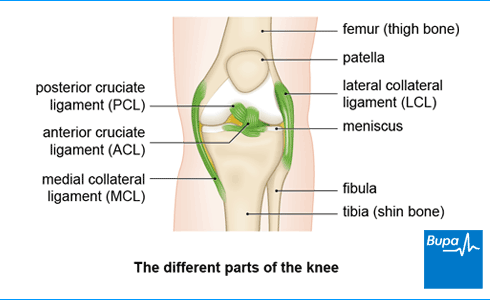
The anterior cruciate ligament (ACL) is one of the ligaments inside your knee – it joins your thigh bone (femur) to the front of your shin bone (tibia). You might injure your ACL by playing sports which involve quick direction changes or sudden stopping, such as football, netball, or skiing.
About anterior cruciate ligament (ACL) injury
The ACL passes in front of another ligament, called the posterior cruciate ligament (PCL). The cruciate ligaments get their name from the fact they form a cross within the knee as they run in different directions from the thigh to the shin bone. Along with the other ligaments in your knee, your ACL keeps your knee stable and prevents your thigh and shin bones moving out of place. This is useful for pivoting movements, as well as walking down hills or stairs. If you have an ACL injury, these activities could be difficult to do.
When your knee ligaments are stretched but not torn, it’s called a sprain. Knee ligament injuries are given different grades depending on how severe they are. Around half of all people with an ACL injury will have injuries to other parts of their knee as well, such as a meniscus tear.
An ACL injury is a partial or complete tear, a stretched ligament, or a detachment of the ligament from the bone.
Causes of anterior cruciate ligament (ACL) injury
Most anterior cruciate ligament (ACL) injuries happen during sports, especially football, netball, and skiing. Women are more likely to injure their ACL than men. An ACL injury may happen if you:
- twist your knee, particularly when your foot is on the ground – for example, you land from a jump and twist in the opposite direction
- quickly change direction when running or walking
- slow down or stop suddenly when running
- overextend your knee joint
If you’re playing contact sports, you can also injure your ACL if you have a direct blow to your knee from a collision with another player.
Symptoms of anterior cruciate ligament (ACL) injury
If you injure your ACL, you may hear a popping sound and feel pain in your knee. Your knee may feel unstable and give way (or feel like it will), and you may not be able to bear weight on it. If you’re playing sport, you’re unlikely to be able to carry on – you won’t be able to walk on it. You’ll quickly develop swelling around your knee joint within an hour or two of injuring it. And you may lose the full range of movement in your knee. With an ACL injury, you will find it hard to continue playing sport or skiing, and you may struggle to stand on the affected leg.
As several knee injuries may cause popping and similar symptoms, you’ll need to see a doctor or physiotherapist to get an accurate diagnosis of your injury.
Self-help for anterior cruciate ligament (ACL) injury
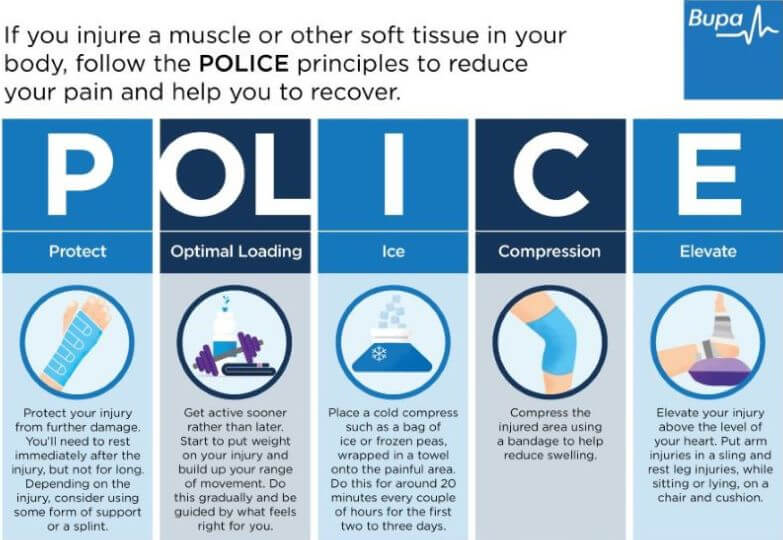
If you think you have a knee injury, you should first follow the POLICE procedure to manage any type of soft tissue injury to your knee. POLICE stands for protect, optimal loading, ice, compression, and elevation.
There are certain things you shouldn’t do in the first three days after your injury, so you don’t damage your knee further. These can be remembered as HARM, which stands for heat, alcohol, running and massage.
If you’re having difficulty bearing weight on your knee, you may need to use crutches or wear a brace to support you for a while. You might be offered a hinge knee brace which takes some of the load off your knee, while allowing it to still bend. Your doctor or physio will explain how long you’ll need to use these for.
Infographic: POLICE principles
Bupa's POLICE infographic (PDF, 0.5 MB) below illustrates the ‘POLICE principles’ to reduce your pain and help you to recover.
Infographic: HARM principle
Bupa's HARM infographic (PDF, 0.6 MB) below illustrates the ‘HARM principle' of things you should avoid doing in the first three days after your injury.

Treatment of anterior cruciate ligament (ACL) injury
You’ll usually need to go to A&E with this kind of injury, where they’ll examine you. They may then refer you to an acute knee clinic, which will organise any investigations and treatment you need.
The treatment you’re offered for your ACL injury will depend on how severe the damage is and how active you normally are. The initial treatment will be to control your pain and swelling using the POLICE and HARM self-help measures (see above). Further treatments may include physiotherapy, medicines and occasionally, surgery.
You may see an orthopaedic surgeon (a doctor who specialises in bone surgery) or a sports medicine professional, such as a sports doctor or physiotherapist. If your symptoms do not settle within one to two weeks you may be offered a magnetic resonance imaging (MRI) scan. This helps the doctor to see your knee ligaments. A doctor or physiotherapist might recommend different treatments depending on the extent of your injury.
Medicines for anterior cruciate ligament (ACL) injury
You can take over-the-counter painkillers, such as paracetamol or ibuprofen, if you’re in pain. Your doctor may be able to prescribe you stronger painkillers if your knee is really painful. As well as easing your pain, non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen may help to reduce inflammation and swelling. Always read the patient information that comes with your medicine, and if you have questions ask your pharmacist or GP for advice. Taking NSAIDs with food can help to reduce the risk of stomach discomfort.
Physiotherapy for anterior cruciate ligament (ACL) injury
Your physiotherapist will assess your knee and then plan a programme of rehabilitation exercises to suit your individual needs. These will include strengthening movements, as well as stretches. The physiotherapy programme will be designed to give you the best chance of returning to your usual activity. Make sure you do the exercises as this is an important part of your recovery. The aim of physiotherapy is to help your knee recover its full range of movement, its strength and stability, and return to working normally.
Surgery for anterior cruciate ligament (ACL) injury
Your surgeon will advise you if you need surgery; for example, if your knee is unstable and gives way when you play sport or sometimes when walking. Surgery may be the best option to repair your injury if you exercise a lot or are in a physically demanding job. For instance, if you:
- play sports that include a lot of twisting and turning – such as football or basketball, to a high level – and you want to get back to it
- have a very physical or manual job, for example you're in the military, a firefighter, police officer or work in construction
You may prefer to give rehabilitation with physiotherapy a try first before you have an operation. Either way, your doctor probably won’t recommend that you have surgery right away after your injury. It’s usually best to wait at least a week or two, to allow the swelling in your knee to go down first.
It usually takes between 6 and 12 months to return to full activity after surgery. And you’ll need to be prepared to undergo an intense and lengthy period of physiotherapy after your operation. Ask your doctor about the pros and cons of surgery, and how it might help you.
Looking for physiotherapy?
You can access a range of treatments on a pay as you go basis, including physiotherapy.
To book or to make an enquiry, call us on 0370 218 6528∧
If you tear your ACL, it will probably be painful, and you may not be able to bear weight on your knee. Your knee may feel unstable and give way (or feel like it will).
Your treatment plan depends on how severe your ACL tear or sprain is. Minor tears or sprains may heal with non-surgical treatment such as physiotherapy. More severe or complete tears will most likely need surgery to repair. Your doctor or orthopaedic surgeon will be able to advise the best treatment for you.
After an injury, a doctor will examine your knee. They will ask if you heard or felt a pop when twisting the knee, and if your knee swelled immediately afterwards. There are some movement tests they can do to see which part of your knee is injured. Your doctor may perform a test called the Lachman's test to see if your ACL is intact.
You may also have an MRI scan.
Posterior cruciate ligament (PCL) injury
With a PCL injury, it’s common to injure other ligaments, or other parts of your knee, at the same time.
Lateral collateral ligament (LCL) injury
An LCL injury is often associated with injuries to the ligaments and tendons in this area, as well as to other parts of the knee.
Medial collateral ligament (MCL) injury
The MCL is the most commonly injured knee ligament. It often gets injured during sports such as rugby.
Meniscal tear
Tears of the menisci are a common injury. When people talk about a ‘torn cartilage’ in their knee they usually mean a meniscus injury.
Patellar tendinopathy (jumper's knee)
Patellar tendinopathy is also called ‘jumper’s knee’ because the injury commonly occurs during sports that involve jumping, such as basketball.
Patellofemoral pain syndrome
Patellofemoral pain syndrome is sometimes called ‘runner’s knee’ because it’s particularly common in people who run or do other sports.
Did our Anterior cruciate ligament (ACL) injury information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Acute knee injuries. Brukner & Khan’s Clinical Sports Medicine: Injuries, Volume 1, 5th ed. (online). McGraw-Hill Medical. csm.mhmedical.com, accessed 7 March 2023
- Knee ligament injuries. PatientPro. patient.info/doctor, last edited 16 August 2022
- Anterior cruciate ligament injury. BMJ Best Practice. bestpractice.bmj.com, last reviewed 1 March 2023
- Anterior cruciate ligament injury. Medscape. emedicine.medscape.com, updated 26 February 2021
- Knee assessment. PatientPro. patient.info/doctor, last edited 16 February 2022
- Meniscus tears. American Academy of Orthopaedic Surgeons. orthoinfo.aaos.org, last reviewed March 2021
- Sprains and strains. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised September 2020
- Knee pain. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised August 2022Treatment of sports injuries. Brukner & Khan’s Clinical Sports Medicine: Injuries, Volume 1, 5th ed. (online). McGraw-Hill Medical. csm.mhmedical.com, accessed 7 March 2023Treatment for knee pain. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 26 March 2020



