Patellofemoral pain syndrome
Your health expert: Mr Damian McClelland, Trauma and Orthopaedic Consultant, and Clinical Director for Musculoskeletal Services at Bupa
Content editor review by Rachael Mayfield-Blake, June 2023
Next review due June 2026
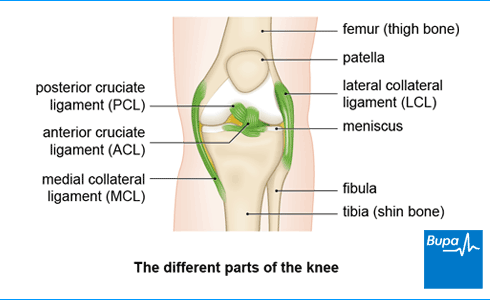
Patellofemoral pain syndrome (PFPS) is the name for a knee condition where you get pain at the front of your knee. It may be behind or around your kneecap (patella). It’s thought to happen because of stress on the joint between your kneecap and your thigh bone (femur).
About patellofemoral pain syndrome
Patellofemoral pain syndrome is one of the most common causes of knee pain. Although anyone can get it, it’s more common in women, and in people in their twenties and thirties. Patellofemoral pain syndrome is sometimes called ‘runner’s knee’ because it’s particularly common in people who run. But you can get it doing other sports too.
Causes of patellofemoral pain syndrome
The exact reasons why you can develop patellofemoral pain syndrome aren’t known. But it’s probably caused by a combination of things. It often develops as a result of overuse – for instance, if you have repeated stress on your knee during sports. It can also be triggered by a sudden change in how often you exercise or how long you exercise for.
You’re more likely to get patellofemoral pain syndrome if there’s a structural problem that affects the joint between your kneecap and thigh bone. This can include minor problems in the alignment of your knee joint and weakness in the muscles around your hip or thigh. These problems can affect the way your knee joint moves, and can cause pain.
Looking for physiotherapy?
You can access a range of treatments on a pay as you go basis, including physiotherapy.
To book or to make an enquiry, call us on 0370 218 6528∧
Symptoms of patellofemoral pain syndrome
Patellofemoral pain syndrome can affect one or both of your knees. The main patellofemoral pain syndrome symptom is a dull, aching pain, which you feel around and in front of your knee or at the back of your kneecap. The pain can also feel sharp. The pain will usually start gradually and get worse if you do a lot of activity.
The pain may be especially bad when doing activities where you need to bend your knee. Such activities include going up and down stairs or doing squats. You may get pain when you sit with your knees bent for a long time.
You may also get crackling or crunching sounds in your knee when you bend or straighten it.
Self-help for patellofemoral pain syndrome
Patellofemoral pain syndrome self-care is important. You’ll need to reduce the amount of activity you do that causes you pain. For example, if you’re a runner, you might reduce the amount of running you do. Alternatively, you could change the type of activity. You could maintain your fitness with exercises such as swimming and cycling that put less stress on your knee.
If you have any swelling, put an ice compress on your knee. Leave it on your knee for 10 to 15 minutes at a time, two to three times a day. This may be especially helpful after you’ve been active. But don’t put ice directly on your skin because it can burn your skin – place a cloth between the ice and your skin.
Treatments for patellofemoral pain syndrome
The initial patellofemoral pain syndrome treatment is to tackle your pain. You can do this by reducing any activities that cause pain and using ice to reduce pain and inflammation (see our section on self-help). Medicines will also help to reduce pain and inflammation. Further treatment includes stretching and strengthening exercises with physiotherapy to gradually get you back to your usual activities.
The patellofemoral pain syndrome recovery time for most people is about four to six weeks.
You may find it helpful to see a sports medicine professional such as a physiotherapist or a sports doctor. An orthopaedic doctor is a doctor who specialises in bone conditions. Your GP may be able to refer you to a physiotherapist or an orthopaedic doctor, or you can book an appointment with a physiotherapist yourself.
Medicines for patellofemoral pain syndrome
You can buy non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or other painkillers over the counter. These may provide short-term pain relief of patellofemoral pain. If your pain is really bad, your GP may be able to prescribe stronger NSAIDs if you need them. Always read the patient information that comes with your medicine, and if you have questions ask your pharmacist or GP for advice.
Physiotherapy for patellofemoral pain syndrome
Your physiotherapist will carefully assess your knee, and then plan an individual programme of patellofemoral pain syndrome exercises. These will help strengthen your knee and leg muscles. The exercises may include stretching and specific strengthening exercises as well as exercises to improve the range of motion of your knee. Make sure you do these exercises because they’re an important part of your recovery.
Other treatments your physio may suggest include the following.
- Manual therapies, such as massage or manipulation of your knee joint may help improve your symptoms.
- Wearing inserts in your shoes (orthoses) may help to reduce pain and improve function. You can buy these from a pharmacy or online. Your physiotherapist can advise you on what to buy or may refer you to see a podiatrist to have them fitted.
- Taping your knee before you do your exercises or wearing a support brace may help with pain. It’s unclear how effective these supports are – but they seem to be helpful for some people.
Surgery for patellofemoral pain syndrome
People with patellofemoral pain syndrome rarely need surgery. But it may be an option if you have severe, persistent pain, and other treatments haven’t worked.
You can fix patellofemoral pain syndrome with a combination of things. First, treat your pain by reducing any activities that cause pain, and use ice. You can also take medicines to provide short-term pain relief. Physiotherapy is an important part of your recovery. A physio will give you a programme of patellofemoral pain syndrome exercises to help strengthen your knee and leg muscles.
For more information, see our section on treatment for patellofemoral pain syndrome.
For most people, it takes about four to six weeks to heal from patellofemoral pain syndrome. It’s important to stick to the exercise programme your physio gives you to recover well.
For more information, see our section on treatment for patellofemoral pain syndrome.
Patellofemoral pain syndrome will often go away with the right treatment. Your physio will carefully assess your knee, and then plan an individual programme of patellofemoral pain syndrome exercises for you to do at home. These will help strengthen your knee and leg muscles and may help with any imbalances in your knee that may have caused the condition.
For more information, see our section on treatment for patellofemoral pain syndrome.
Patellofemoral pain syndrome feels like a dull, aching pain, either around and in front of your knee or at the back of your kneecap. The pain can also feel sharp. The pain may feel worse when you bend your knee going up and down stairs or doing squats. It can also be painful when sitting with your knees bent for a long time.
For more information, see our section on symptoms of patellofemoral pain syndrome.
Posterior cruciate ligament (PCL) injury
With a PCL injury, it’s common to injure other ligaments, or other parts of your knee, at the same time.
Anterior cruciate ligament (ACL) injury
An ACL injury can be a partial or a complete tear, an overstretch, or a detachment of the ligament.
Medial collateral ligament (MCL) injury
The MCL is the most commonly injured knee ligament. It often gets injured during sports such as rugby.
Lateral collateral ligament (LCL) injury
An LCL injury is often associated with injuries to the ligaments and tendons in this area, as well as to other parts of the knee.
Meniscal tear
Tears of the menisci are a common injury. When people talk about a ‘torn cartilage’ in their knee they usually mean a meniscus injury.
Patellar tendinopathy (jumper's knee)
Patellar tendinopathy is also called ‘jumper’s knee’ because the injury commonly occurs during sports that involve jumping, such as basketball.
Did our Patellofemoral pain syndrome information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Bump JM, Lewis L. Patellofemoral syndrome. StatPearls Publishing. www.ncbi.nlm.nih.gov, last updated 13 February 2023
- Patellofemoral syndrome. Medscape. emedicine.medscape.com, updated 9 January 2023
- Patellofemoral pain syndrome. BMJ Best Practice. bestpractice.bmj.com, last reviewed 24 April 2023
- Sprains and strains. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised September 2020
- Find a physio. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 24 January 2023
- Treatment for knee pain. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 26 March 2020
- Patellofemoral pain syndrome. American Academy of Orthopaedic Surgeons. orthoinfo.aaos.org, last reviewed October 2020



