Ilio-tibial band (ITB) syndrome
Your health expert: Mr Damian McClelland, Trauma and Orthopaedic Consultant, and Clinical Director for Musculoskeletal Services at Bupa
Content editor review by Rachael Mayfield-Blake, Freelance Health Editor, June 2023
Next review due June 2026
Iliotibial band (ITB) syndrome – also known as ITB friction syndrome – is an injury that causes knee pain. ITB syndrome is the most common cause of pain on the outside of the knee in runners , cyclists and other sports people.
About Ilio-tibial band syndrome
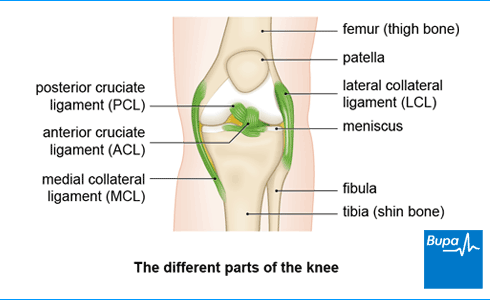
Your iliotibial band (ITB) is a thickened band of tissue that runs all the way down the length of the outside of your thigh. Your ITB works with your knee ligaments to help stabilise your knee joint.
One theory of how ITB syndrome happens is that your ITB rubs repeatedly against the lower end of your thigh bone as it joins your knee. This friction causes inflammation and pain. But there are other theories of how it happens, and it may be caused by a combination of these.
Causes of iliotibial band syndrome
You usually get iliotibial band (ITB) syndrome if you run or cycle, but you can also get it from other sports such as hockey or football. ITB syndrome is an overuse injury – it tends to get worse with repeated movement. You’re more likely to get it the more exercise you do during a week.
There are certain things to do with how you run or exercise that can increase your risk of developing ITB syndrome. These include if you:
- run for long distances or for a long time
- are new to running or you suddenly increase how far or how often you run
- wear worn-out running shoes
- run on slippery or uneven ground
- overpronate (your foot rolls inwards when you run)
There are some things in your body that can make you more susceptible to developing ITB syndrome too. These include:
- weak muscles in your hips or knees
- tightness in your ITB
- slight differences in the length of your legs
Symptoms of iliotibial band syndrome
The main iliotibial band (ITB) symptom is a sharp pain or ache on the outside of your knee. The pain may spread up or down your leg. The outside of your knee may be tender to the touch and you may have some swelling. The pain may be worse when you run downhill or if you run or cycle for longer than normal. You may find that the pain starts at a similar point in your run, and goes when you stop.
Usually, you’ll only feel pain when you do activities such as running or cycling. But if the problem gets worse, it can start to affect you even when you go for a walk or sit with your knee bent.
Self-help for iliotibial band syndrome
It’s important that you stop doing the activity that brings on your pain. If you’re only getting mild pain, doing less of your activity may help. For instance, stop running before the time or distance when you normally get the pain. If your pain is more severe, you should stop altogether. You can keep active by doing exercise that doesn’t bring on pain – for example, swimming (just using your arms – use a float between your legs).
When you first develop ITB syndrome, it can help to put ice or a cold compress on the painful area. Apply it for 15–20 minutes at a time, every two to three hours. Don’t put ice straight on your skin – wrap the ice in a cloth or towel.
Treatment for iliotibial band syndrome
The initial treatment for iliotibial band (ITB) syndrome will aim to reduce your pain and inflammation. You can do this with rest and ice (see our section on self-help for iliotibial band syndrome), and medicines. Further iliotibial band treatment includes physiotherapy to gradually get you back to your usual activities.
Most people recover and can go back to sports or running within six to eight weeks.
A sports medicine professional such as a physiotherapist or a sports doctor can diagnose and treat ITB syndrome. Your GP may refer you or you can book an appointment with a physiotherapist directly.
Medicines for ITB syndrome
You can take over-the-counter painkillers such as non-steroidal anti-inflammatory drugs (NSAIDs), which include ibuprofen, to help ease your pain and reduce inflammation and swelling. Your doctor may prescribe stronger NSAIDs if your pain is really bad. Always read the patient information that comes with your medicine, and if you have questions ask your pharmacist or GP for advice.
Your GP may recommend that you have a steroid injection into the inflamed area if you have severe pain or swelling.
Physiotherapy for ITB syndrome
Your physiotherapist will carefully assess your knee and plan an individual programme of iliotibial band syndrome exercises to help strengthen your knee and leg muscles gradually.
Treatment usually involves manual techniques (such as massage) and stretching exercises at first. Your physiotherapist may suggest you try using a foam roller as part of a home exercise programme to help reduce your pain. You’ll then usually need to follow some specific strengthening exercises to help you recover. Finally, your physiotherapist will advise you on how you can gradually get back to your normal activities. Make sure you do the exercises because this is an important part of your recovery.
Your physiotherapist may give you some advice on how to try to prevent the problem coming back. For example, you may need to change your running shoes to correct problems with your foot movement or look at the way you run (your gait) on a treadmill.
Surgery for ITB syndrome
Surgery isn’t usually used to treat ITB syndrome. Your doctor will only suggest you have an operation if other treatments haven’t worked. Ask your doctor for more information on the best treatment for you.
Looking for physiotherapy?
You can access a range of treatments on a pay as you go basis, including physiotherapy.
To book or to make an enquiry, call us on 0370 218 6528∧
You can fix iliotibial band (ITB) syndrome with a combination of things. Medicines can ease pain and inflammation, and physiotherapy can help you recover. Your physiotherapist will use manual techniques, such as massage, and stretching exercises. They’ll also give you some strengthening exercises to do at home. They’ll help you gradually get back to your normal activities.
For more information see our section on treatment for of iliotibial band syndrome.
For most people, it takes about four to eight weeks to heal from iliotibial band (ITB) syndrome. It’s important to stick to the exercise programme your physiotherapist gives you to recover well.
For more information see our section on treatment for of iliotibial band syndrome.
An iliotibial band (ITB) injury feels like a sharp pain or ache on the outside of your knee. This may spread up or down your leg. The outside of your knee may feel tender to the touch. The pain may be worse when you run downhill or if you run or cycle for longer than normal.
For more information see our section on symptoms of iliotibial band syndrome.
Posterior cruciate ligament (PCL) injury
With a PCL injury, it’s common to injure other ligaments, or other parts of your knee, at the same time.
Anterior cruciate ligament (ACL) injury
An ACL injury can be a partial or a complete tear, an overstretch, or a detachment of the ligament.
Medial collateral ligament (MCL) injury
The MCL is the most commonly injured knee ligament. It often gets injured during sports such as rugby.
Common running injuries
Patellar tendinopathy (jumper's knee)
Patellar tendinopathy is also called ‘jumper’s knee’ because the injury commonly occurs during sports that involve jumping, such as basketball.
Patellofemoral pain syndrome
Patellofemoral pain syndrome is sometimes called ‘runner’s knee’ because it’s particularly common in people who run or do other sports.
Did our Ilio-tibial band (ITB) syndrome information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Iliotibial band syndrome. BMJ Best Practice. bestpractice.bmj.com, last reviewed 24 April 2023
- Hadeed A, Tapscott DC. Iliotibial band friction syndrome. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 30 May 2022
- Hutchinson LA, Lichtwark GA, Willy RW, et al. The iliotibial band: a complex structure with versatile functions. Sports Med 2022; 52(5):995–1008. doi: 10.1007/s40279-021-01634-3
- Sprains and strains. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised September 2020
- Find a physio. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 24 January 2023
- Treatment for knee pain. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed 26 March 2020



