Achilles tendinopathy
- Annie Henderson, Triage Physiotherapist at Bupa
Key points
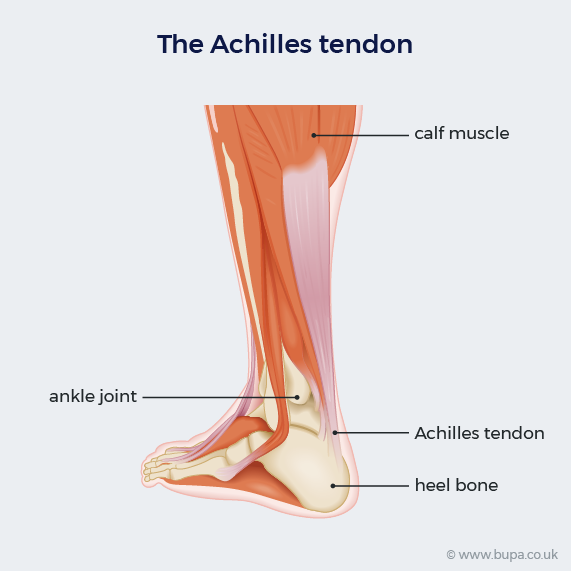
- Achilles tendinopathy is an injury to the Achilles tendon, which connects your calf muscle to your heel bone.
- It’s caused by overuse and repeated stress on the tendon.
- Symptoms of Achilles tendinopathy include pain, stiffness, and swelling around the tendon and your heel.
- Achilles tendinopathy is common, especially if you’re very active.
What is Achilles tendinopathy?
Achilles tendinopathy is an injury to the band of tissue (tendon) that connects the muscles in your lower leg to your heel bone. The Achilles tendon helps you to move your foot – when you walk, run, climb, or jump. It’s a common injury, especially if you’re very active.
Achilles tendinopathy is sometimes called Achilles tendonitis. But doctors don’t usually use this term anymore. Tendonitis means your tendon is inflamed. But because there isn’t always inflammation when your tendon is injured, this term isn’t strictly accurate.
Achilles tendinopathy symptoms
Achilles tendinopathy can cause several symptoms, including:
- pain in your heel – this may be an ache or a sharp pain, which feels worse when you’ve been active or put pressure on it
- stiffness in your tendon – this is often worse first thing in the morning or if you’ve been resting for a while
- swelling at the back of your ankle
- tenderness when you touch your tendon
- a grating noise or creaking feeling (crepitus) when you move your ankle
If you feel a sudden sharp pain in your heel or calf, this could mean you’ve torn your tendon. This is called an Achilles tendon rupture. You may hear a snap and have trouble bearing any weight on your leg. If this happens, seek urgent medical advice.
Self-help for Achilles tendinopathy
You can try lots of things to ease the symptoms of Achilles tendinopathy without needing to see a health professional. These self-help measures include the following.
- Rest your tendon by reducing (or stopping) the activity that triggered your symptoms.
- Apply cold packs or ice wrapped in a towel to ease your pain and reduce any swelling. You can do this for 20 to 30 minutes every two to three hours. But don’t apply ice directly to your skin because ice may damage your skin.
- Take over-the-counter painkillers such as paracetamol to help ease the pain. Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen may also help to ease the pain at first. But you shouldn’t take NSAIDs for very long. Always read the patient information leaflet that comes with your medicines.
Try to carry on putting weight on your leg if you’re able to. It may also help to do some gentle calf stretches if you can. You may be able to do some exercises that don’t put too much stress on your Achilles tendon – for example, swimming.
You can gradually restart your normal activities once the pain starts to ease. But avoid uphill and downhill running until the pain has completely gone, and stick to softer running surfaces. You should also make sure you warm up well and do plenty of calf stretches and massage.
You might find heel lifts helpful. These are insoles that you fit into each of your shoes. They can reduce the stress on your Achilles tendon and ease your symptoms.
For more tips on avoiding further injury, see our section on prevention of Achilles tendinopathy.
Diagnosis of Achilles tendinopathy
Your GP or physiotherapist will ask you about your symptoms and examine your leg, heel and ankle. They may ask you to do a series of movements or exercises so they can see how well you can move your leg. They may squeeze your calf muscle to check the movement of your foot.
They may also:
- ask you about your medical history to check for other related causes or conditions
- check if any medicines you’re taking may have increased your risk of Achilles tendinopathy
For more information, see our section on causes of Achilles tendinopathy.
Achilles tendinopathy can usually be diagnosed from your symptoms. So you won’t usually need any further tests or scans. But sometimes your GP or physiotherapist may suggest a referral for an MRI or ultrasound if:
- your symptoms are severe
- they suspect a rupture
- you’re not responding to treatment
Physiotherapy services
Our evidence-based physiotherapy services are designed to address a wide range of musculoskeletal conditions, promote recovery, and enhance overall quality of life. Our physiotherapists are specialised in treating orthopaedic, rheumatological, musculoskeletal conditions and sports-related injury by using tools including education and advice, pain management strategies, exercise therapy and manual therapy techniques.
To book or to make an enquiry, call us on 0345 850 8399
Achilles tendinopathy treatment
If self-help measures aren’t helping your Achilles tendinopathy, your GP or physiotherapist may suggest some treatments. This will usually involve a physiotherapy exercise programme to start with, before moving onto other treatments if this doesn’t work. Most people find their symptoms improve within around 12 weeks.
Physiotherapy exercises for Achilles tendinopathy
Physiotherapy can help to build up the strength and function in your Achilles tendon.
Your physiotherapist will suggest some exercises for you to do. The specific exercises will depend on your symptoms. But they usually involve stretching and lengthening your Achilles tendon and surrounding muscles over time. You’ll probably need to do Achilles tendinopathy exercises two to three times a day, on most days, for at least three months to get the best results.
Other treatments for Achilles tendinopathy
If your Achilles tendinopathy doesn’t improve with self-help measures or physiotherapy exercises, there may be other treatments you can try. These include the following.
- Extracorporeal shockwave therapy. This is where a machine passes shockwaves through your skin to the damaged part of your tendon. This may help to ease your pain. You may need several sessions.
- Blood or platelet-rich plasma (PRP) injections. These use part of your own blood that’s rich in growth factors. The injections may help your Achilles tendon to heal faster. Your doctor injects the plasma or blood into or around your damaged tendon. They may use ultrasound to make sure they’re injecting into the right place.
- Dry needling. This involves passing a thin needle into your tendon. This aims to trigger the healing process and strengthen your tendon.
Your physiotherapist may be able to give you some of these therapies. But for others, you may need to be referred to a specialist sports or musculoskeletal doctor. Some of these treatments may only be available in specialist centres or as part of a research trial.
Achilles tendinopathy surgery
Most people don’t need surgery for Achilles tendinopathy. But if you’ve been trying other treatments for several months and they haven’t helped, surgery may be an option. You’ll need a referral to a specialist foot and ankle surgeon. They can assess if surgery may be helpful for you. Your surgeon may ask you to have some scans to check the condition of your tendon.
Surgery involves removing damaged areas of your tendon and repairing what’s left of it. Your surgeon may need to use tissue from higher up your Achilles tendon or from a different tendon for these repairs. It will take time to recover from Achilles tendon surgery, and the surgery will leave scars. Surgery doesn’t work for everyone with Achilles tendinopathy.
Causes of Achilles tendinopathy
Achilles tendinopathy is usually caused by overuse – which is repeated stress on your Achilles tendon over time. This can cause changes to the structure of your tendon. Tiny tears in your tendon may make your tendon painful and irritated.
Any sports or activities that put stress on your Achilles tendon can lead to Achilles tendinopathy. This includes:
- running, including in football
- jumping, as in dancing, gymnastics and tennis
- cycling, if your saddle is too low
You may also be more likely to damage your Achilles tendon if you:
- use badly designed equipment or wear the wrong footwear
- have a poor technique or haven’t trained properly for the activity you’re doing
- suddenly increase how much exercise you do or increase the intensity of your exercise
- train on hard or sloping surfaces
For advice on how to reduce your risk, see our section on prevention of Achilles tendinopathy.
Other things that can make you more likely to develop Achilles tendinopathy include:
- getting older – your Achilles tendon becomes less flexible and less able to cope with stress
- having a family history of the condition
- if you’ve injured your tendon or the muscles around it in the past
- having certain long-term health conditions such as rheumatoid arthritis, diabetes, high cholesterol or thyroid problems
- being very overweight or obese
- doing too much or too little exercise
- taking certain medicines such as corticosteroids, statins or antibiotics belonging to the quinolone group
Prevention of Achilles tendinopathy
- There are several things you can do to help prevent Achilles tendinopathy. Make sure you wear appropriate and well-fitting shoes for running and other activities you do.
- Whether you’re active through work or sports, make sure you use the right equipment and techniques.
- Gradually build up new activities slowly. You should increase the intensity and duration of your activities slowly over time.
- Warm up well before you start exercising and stretch your calf muscle afterwards.
- If you have underlying health problems that put you more at risk, make sure they’re being treated properly.
Aim to maintain a healthy weight because being overweight can increase your risk of Achilles tendinopathy.
Wearing orthotics (special inserts) in each shoe may help if there’s a problem with the shape of your foot or how you walk.
Looking for fast access to quality care?
If you’re suffering from a muscle, bone or joint injury, as long as your symptoms are covered under your policy you can call us for advice and we can often authorise a consultation without the need for a GP referral.
To get a quote or to make an enquiry, call us on 0808 273 6216∧
Achilles tendon rupture
An Achilles tendon rupture is when you tear the tissue that connects your calf muscle to your heel bone.
Physiotherapy
Over-the-counter painkillers
Other helpful websites
Discover other helpful health information websites.
Did our Achilles tendinopathy information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Achilles tendinopathy and rupture. Patient. patient.info, last updated March 2022
- Tendinopathy. BMJ Best Practice. bestpractice.bmj.com, last reviewed May 2024
- Tarantino D, Mottola R, Resta G, et al. Achilles tendinopathy pathogenesis and management: A narrative review. Int J Environ Res Public Health 2023; 20(17):6681. doi: 10.3390/ijerph20176681
- Achilles tendon injuries. Medscape. emedicine.medscape.com, updated September 2022
- Achilles tendon. Britannica. www.britannica.com, accessed June 2024
- Achilles tendinopathy. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised June 2020
- Malliaras P. Physiotherapy management of Achilles tendinopathy. J Physiother 2022; 68(4):221–37. doi: 10.1016/j.jphys.2022.09.010
- Achilles tendinitis. MSD Manuals. msdmanuals.com, reviewed/revised November 2023
- Achilles tendon pain. British Orthopaedic Foot and Ankle Society (BOFAS). www.bofas.org.uk, accessed June 2024
- Achilles tendinopathy. Versus Arthritis. www.versusarthritis.org, accessed June 2024
- Heel pain. Royal College of Podiatry. rcpod.org.uk, accessed June 2024
- Find a chartered physiotherapist. Chartered Society of Physiotherapy. www.csp.org.uk, last reviewed January 2023
- Extracorporeal shockwave therapy for Achilles tendinopathy. The procedure. Interventional Procedures Guidance IPG571. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published December 2016
- Autologous blood injection for tendinopathy. The procedure. Interventional Procedures Guidance IPG438. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, published January 2013
- Stoychev V, Finestone AS, Kalichman L. Dry needling as a treatment modality for tendinopathy: a narrative review. Curr Rev Musculoskelet Med 2020; 13(1):133–40. doi:10.1007/s12178-020-09608-0
- Personal communication from Annie Henderson, Bupa Triage Physiotherapist, July 2024
- Victoria Goldman, Freelance Health Editor



