Trigger finger
Your health expert: Professor Adam Watts, Trauma and Orthopaedic Surgeon
Content editor review by: Rachael Mayfield-Blake, Freelance Health Editor, September 2023
Next review due September 2026
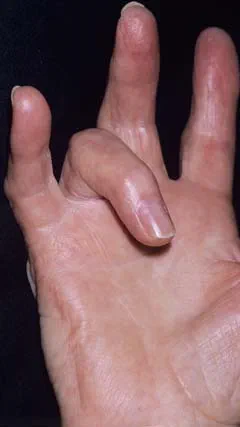
Trigger finger (stenosing tendinopathy) is a condition where your finger or thumb ‘catches’ or locks in place when you bend it. Sometimes trigger finger can recover by itself after a few weeks. If not, there are treatments that can help, which include painkillers, splinting, steroid injections and surgery.
We’ll use the term ‘trigger finger’ here, but our information also covers trigger thumb.
About trigger finger
Trigger finger happens because of a problem with a tendon in your finger. The tendons are long cords that attach your finger bones to muscles in your forearms. They run through tunnels called tendon sheaths. These allow your tendon to move smoothly as you bend and straighten your fingers. The tendon sheath has bands of tissue to hold your tendon close to your finger bones, which are called pulleys.
If you have trigger finger, the tendon sheath thickens, which narrows the space for the tendon and it can’t run through the tunnel smoothly. This can make the fibres of the tendon swell and form a small lump (nodule). This nodule then catches on a pulley in the tendon sheath as you move your finger. If the problem gets worse, your finger can sometimes get stuck (locked) in a bent position.
The ring finger and thumb (trigger thumb) are most often affected in your dominant hand. But trigger finger can happen in any of your fingers on both hands. It’s not unusual to get it in more than one finger.
Causes of trigger finger
We don’t know what the trigger finger cause is but some things make you more likely to get it. It’s more common in women than men, for example. And while you can get trigger finger at any age, it’s most common in people in their 50s and 60s. Children are less likely to get it than adults but if they do, it usually affects their thumb. For more information, see our FAQ: Can children have trigger finger?
You may get trigger finger after you injure your hand. Or it might happen if your work or hobbies involve repeated, powerful hand movements. These include movements that put pressure on your palm or where you use a powerful grip, such as using heavy shears.
Trigger finger is more common in people with certain health conditions, including:
- diabetes
- rheumatoid arthritis
- an underactive thyroid gland (hypothyroidism)
- amyloidosis
You may get trigger finger at the same time as other problems with your hand and wrist – for example, carpal tunnel syndrome.
There isn’t much you can do to prevent trigger finger. But if you start having symptoms, take note of anything that seems to cause them. Then try and avoid those activities for a while.
Symptoms of trigger finger
Symptoms of trigger finger can include:
- pain in your hand – it often begins as an ache in your palm when you move the affected finger
- a painful catching or popping sensation when you bend and straighten your finger
- your finger getting stuck (locked) in a bent position – you may be able to pull it straight with your other hand
- a sore lump in your palm at the base of the affected finger
- stiffness in your finger, which may be worse first thing in the morning or if you haven’t moved your hand in a while
The symptoms tend to develop over weeks and months but can progress more quickly. You may also notice early signs of trigger finger in your other fingers on the same or on the other hand. Contact your GP if you get these symptoms.
Diagnosis of trigger finger
Your GP will ask about your symptoms and your medical history. They’ll ask if there’s anything that could have set off your symptoms, such as an injury or repeated stress on your finger.
Your GP will examine your hand and the affected finger. They’ll feel your hand to see if there’s a tender nodule in your palm at the base of the finger. They may ask you to bend and straighten your fingers, while they feel the palm of your hand. This may let them feel any catching of your tendon. Tell your GP if your hand is painful so they know to be gentle when they examine it.
You won’t usually need to have any tests. But if your GP isn’t sure what’s causing your symptoms, they may recommend you have an ultrasound scan.
Treatment of trigger finger
Self-help
Sometimes, trigger finger gets better without any treatment. Your doctor may advise you to rest your hand and try not to do any activities that make it worse for a while. If you have mild symptoms, these may go away on their own within a few weeks.
If your trigger finger doesn’t go away, you may need one of the trigger finger treatments below.
Splinting and pain relief
Your GP may suggest a combination of a trigger finger splint and pain relief for four to six weeks to see if this helps. They may recommend you see a physiotherapist.
You wear the splint on your finger or thumb at night to keep it straight and stop it moving. This will help smooth the thickened part of your tendon by preventing it from rubbing on the tendon sheath.
You can take over-the-counter medicines, such as ibuprofen or paracetamol, to reduce pain and swelling in your finger. Always read the patient information leaflet that comes with your medicine. If you have any questions, ask a pharmacist.
Steroid injection
Your GP or specialist doctor may offer you a steroid injection instead of splinting and painkillers or if splinting and painkillers don’t help. Or, you may have a steroid injection as well as these. If you don’t want to have a steroid injection, your doctor may refer you to a hand therapist for further splinting.
If you have the injection, your doctor will inject a steroid medicine into the inflamed area of your tendon sheath. The steroid is mixed with a local anaesthetic medicine to lessen pain. Your symptoms may improve within a few days but it may take months. If the first injection doesn't help or only partially works, your doctor may offer you another one.
Steroid injections don’t work for everyone with trigger finger. If your symptoms don’t go away after steroid injections, your doctor may offer you an operation.
Surgery
If other treatments don’t work, your doctor may offer you trigger finger surgery. The operation is called ‘trigger release’ surgery. Trigger finger surgery may be the best treatment for you if your finger is locked in a bent position. Ask your doctor to explain the risks and benefits of trigger finger surgery for you.
In trigger release surgery, your surgeon will cut the part of the tendon sheath that’s blocking movement. This lets your finger move normally again, and eases any pain. There are two main ways of doing this.
- Open trigger release surgery. Your surgeon will make a small cut in the palm of your hand to reach the tendon sheath. You’ll have a small scar afterwards.
- Percutaneous trigger release surgery. Your surgeon will put a needle through the skin of your palm to reach and cut the tendon sheath. This procedure isn’t suitable for everyone.
Your doctor will give you more details about these procedures and what’s involved. Both procedures are usually done as day-cases, which means you won’t need to stay in hospital overnight. You’ll have a local anaesthetic so you won’t feel any pain, but you’ll be awake.
Your doctor will encourage you to move your finger right away after the surgery. You might get some swelling or soreness for a while. And your finger or thumb might feel a bit stiff at first. It can take several months for all the swelling and stiffness to go away.
There’s a low risk of ongoing trigger finger symptoms, or them coming back after surgery.
Physiotherapy services
Our evidence-based physiotherapy services are designed to address a wide range of musculoskeletal conditions, promote recovery, and enhance overall quality of life. Our physiotherapists are specialised in treating orthopaedic, rheumatological, musculoskeletal conditions and sports-related injury by using tools including education and advice, pain management strategies, exercise therapy and manual therapy techniques.
To book or to make an enquiry, call us on 0345 850 8399
Trigger finger can heal on its own but it depends on how severe your symptoms are. If you have mild symptoms, they may go away on their own, particularly if you stop doing activities that might have caused it. But sometimes trigger finger symptoms can get worse and start to interfere with life. The pain may become severe, and your finger may become stuck in a bent position. You’ll then need treatment.
See our treatment of trigger finger section for more information.
The best way to fix trigger finger will depend on how severe it is and what’s likely to have led you to develop it. Mild trigger finger sometimes gets better without any treatment. If your trigger finger doesn’t go away, you may need a trigger finger treatment, which can include a trigger finger splint, a steroid injection, or surgery.
See our treatment of trigger finger section for more information.
The exact cause of trigger finger isn’t known but some things make you more likely to get it. You may get trigger finger after you injure your hand, for example. Or it might happen through repeated, powerful hand movements. Trigger finger is also more common in people with certain health conditions, including diabetes and rheumatoid arthritis .
See our causes of trigger finger section for more information.
No, trigger finger isn’t a form of arthritis. But if you have a form of arthritis, such as rheumatoid arthritis , it may increase your risk of getting it. Children with trigger thumb are sometimes found to have juvenile rheumatoid arthritis
See our causes of trigger finger section for more information.
Carpal tunnel syndrome
Carpal tunnel syndrome is a condition where a nerve in your wrist is under pressure (compressed).
Rheumatoid arthritis
Rheumatoid arthritis is a condition which causes pain, swelling and stiffness in your joints.
Type 1 diabetes
Type 2 diabetes
Other helpful websites
Discover other helpful health information websites.
Did our Trigger finger information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Trigger finger. Medscape. emedicine.medscape.com, updated 17 January 2023
- Jeanmonod R, Harberger S, Waseem M. Trigger finger. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 7 August 2022
- Trigger finger/thumb. British Society for Surgery of the Hand. www.bssh.ac.uk, accessed 31 July 2023
- Tenosynovitis of the hand and wrist. BMJ Best Practice. bestpractice.bmj.com, last reviewed 30 June 2023
- Trigger finger. American Academy of Orthopaedic Surgeons. orthoinfo.aaos.org, last reviewed October 2022



