Underactive thyroid (hypothyroidism)
Your health expert: Dr Amilia Alifrangis, Lead Physician at Bupa Health Clinics, and Dr Raja N R Padidela, Consultant in Paediatric and Adolescent Endocrinology
Content editor review by Victoria Goldman, September 2023
Next review due August 2026
If you have an underactive thyroid (hypothyroidism), your thyroid gland isn’t making enough thyroid hormones. This can cause tiredness, weight gain and depression. Treatment with replacement thyroid hormones usually improves your symptoms.
About underactive thyroid
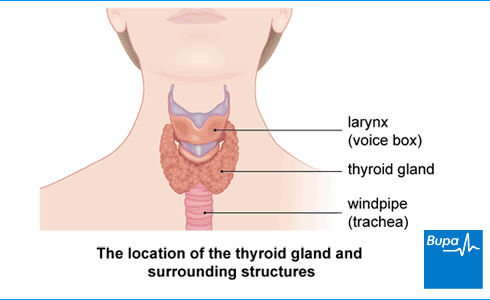
Your thyroid gland is in your neck, in front of your windpipe. It makes two main hormones called thyroxine (T4) and triiodothyronine (T3).
Thyroid hormones affect tissues throughout your body. These help to control your metabolism. Your metabolism is the combination of all the chemical processes happening in your body. It includes processes that change the food you eat into energy. If you don’t have enough thyroid hormones, your body’s metabolism slows down. This can cause a wide range of symptoms – see our Symptoms of underactive thyroid for more information.
Around one or two out of every 100 people develop an underactive thyroid. Women are up to 10 times more likely than men to develop this condition.
How a thyroid gland can become underactive
Video explaining underactive thyroid | Watch in 2:23 mins
Having an underactive thyroid slows down the body's metabolism, leading to symptoms including tiredness and putting on weight. Find out more in the video
Causes of underactive thyroid
In the UK, the most common cause of an underactive thyroid is autoimmune thyroiditis. This is also known as Hashimoto's thyroiditis. It happens when your immune system attacks your thyroid gland. Your thyroid gland gets damaged and stops making enough thyroid hormones.
An underactive thyroid can also be caused by:
- surgery to remove your thyroid gland
- radioactive iodine treatment for an overactive thyroid
- radiotherapy for thyroid cancer
- some medicines, such as lithium and amiodarone
- an infection caused by a virus (thyroiditis)
- pregnancy – some women develop an underactive thyroid in the first year after their baby is born
- having a thyroid gland that didn’t develop properly before you were born
- having a genetic condition from birth that means your body can’t make thyroid hormones properly
Thyroid problems from some of these causes, such as surgery, pregnancy and infections, usually only last for a short time.
Symptoms of underactive thyroid
Underactive thyroid symptoms usually develop slowly and gradually. Signs of an underactive thyroid can be quite vague and can be caused by many other conditions. This can sometimes make an underactive thyroid hard to diagnose. You may not get any symptoms at all.
If you do get underactive thyroid symptoms, these may include:
- feeling the cold
- feeling weak and tired and having no energy
- putting on weight
- constipation
- if you’re a woman, your periods may be heavy, irregular or stop completely
- dry skin
- not feeling so hungry
- muscle or joint pain
- losing your hair, which may be thinner overall (but usually grows back with treatment)
- a hoarse voice
- a slow heartbeat
Having an underactive thyroid can affect your mental health too. You may become forgetful and find it difficult to concentrate. You may find it harder to think clearly, called “brain fog”. And you may feel emotionally up and down, and get depressed.
If you have any of these symptoms, contact your GP.
GP Subscriptions – Access a GP whenever you need one for less than £20 per month
You can’t predict when you might want to see a GP, but you can be ready for when you do. Our GP subscriptions are available to anyone over 18 and give you peace of mind, with 15-minute appointments when it suits you at no extra cost.
Diagnosis of underactive thyroid
Your GP will ask about your symptoms and examine you. They may also ask you about your medical history.
- If your GP thinks you may have an underactive thyroid, they’ll ask you to have one or more blood tests. This is to check the levels of thyroid hormones in your body. There are two main hormones measured in blood tests. TSH (thyroid-stimulating hormone). This is made by your pituitary gland to control your thyroid gland. It tells your thyroid to make more hormones if the levels of thyroid hormone in your blood get too low.
- FT4 – free T4 (thyroxine). This hormone is made by your thyroid gland.
You may hear these blood tests referred to as ‘thyroid function tests’. If you have an underactive thyroid, you will often have a TSH level above normal and a free T4 level below normal.
If the results of the blood tests show that you have underactive thyroid problems, you’ll usually be treated by your GP. But sometimes your GP will refer you to an endocrinologist – a doctor who specialises in treating hormone problems such as thyroid conditions.
If you’re diagnosed with an underactive thyroid, you may have some other blood tests too.
Subclinical (borderline) hypothyroidism
Some people have a mildly underactive thyroid, with few or no signs of low thyroid hormones. Doctors call this subclinical hypothyroidism. If you have this, your blood test will show that your TSH is raised but your free T4 is normal. This is fairly common, especially in older people. Some people with this condition can get symptoms of underactive thyroid as the years go by. It’s important to check their thyroid hormone levels every year.
If you have subclinical hypothyroidism, your GP will offer to monitor your thyroid hormones every year. This will check whether your thyroid is getting less active. See our Treatment of underactive thyroid section for more information about treating borderline underactive thyroid.
Treatment of underactive thyroid
The aim of underactive thyroid treatment is to ease your symptoms and prevent any complications. This means getting your thyroid hormone levels back to within the normal range. Once your treatment is working well, you should feel much better.
An underactive thyroid doesn’t usually get worse over time. But the amount of medicine your body needs may vary. Your GP may need to adjust the dose every now and then if:
- your symptoms come back
- your blood tests show your thyroid hormone levels are outside the normal range again
If your symptoms continue to affect your quality of life, talk to your doctor.
If you have just a mildly underactive thyroid (subclinical hypothyroidism), your doctor may recommend you have treatment too. This depends on:
- your age
- your blood test results
- whether you’ve had treatment for thyroid problems in the past
- your symptoms
If you’re not having treatment, your GP will usually check your thyroid hormone levels every year. If you develop symptoms, your GP may suggest that you start having treatment.
Medicines
If you have an underactive thyroid, your doctor may prescribe a hormone replacement medicine called levothyroxine (thyroxine). You take this once a day as a tablet on an empty stomach, preferably first thing in the morning before breakfast. If you’re over 65 or have heart disease, you’ll start by taking a small amount of levothyroxine. This will be increased every four weeks to give your body a chance to adjust gradually.
After you start taking levothyroxine, your GP will take a blood sample every three months to check that your TSH level is returning to normal. They may need to adjust your dose, depending on the results of these tests.
Levothyroxine can interact with some other medicines and iron supplements. Your doctor or pharmacist may also give you instructions about when and how to take it. It’s important to read the patient information leaflet that comes with your medicine. If you have any queries about taking your medicine, you can ask your pharmacist for advice.
It can take a while for your hormone levels to get back to normal. So it may be a few months until you start to feel better. Once your thyroid levels have returned to normal, you’ll usually have a blood test once a year to check your thyroid hormone levels. You’ll probably need to take levothyroxine for the rest of your life.
Most people who take levothyroxine make a full recovery and feel much better. But around one in every 20 people with an underactive thyroid will still have some symptoms, even when their hormone levels are back to normal. If this happens, speak to your GP. Your GP may arrange for you to have some tests to see whether something else is causing your symptoms.
Natural thyroid extract (natural desiccated thyroid, NDT) is not routinely recommended for an underactive thyroid. This is because research doesn’t show that this extract works any better than levothyroxine. Doctors also don’t know whether this extract causes any long-term effects on the body. Liothyronine (T3) is also not prescribed routinely by doctors for the same reasons.
Complications of underactive thyroid
The symptoms of an underactive thyroid can have a serious impact on your day-to-day life. Your physical and mental tiredness and lack of energy may mean you find it hard to do your usual activities. You may find that your quality of life suffers and it affects your work life, relationships and social life.
Other complications of underactive thyroid include:
- fertility problems
- heart problems, such as chest pain (angina), coronary heart disease and heart failure
- myxoedema – this is a rare but serious condition (sometimes life-threatening), usually linked with a severe underactive thyroid that hasn’t been treated
Being overtreated for underactive thyroid can also cause complications. This can be avoided by taking your prescribed medicine regularly and having the regular blood tests that your GP recommends. The complications include osteoporosis and atrial fibrillation (an irregular heart rhythm). For information on things to watch out for when you’re taking levothyroxine, see our After treatment for underactive thyroid section.
Underactive thyroid and pregnancy
If you know you have an underactive thyroid, tell your GP as soon as you think you’re pregnant. You’ll need to have regular checks every four to six weeks during your pregnancy. This will make sure your thyroid hormones are at a healthy level. The dose of your medicine may need to be changed during pregnancy. You may be referred to an endocrinologist and obstetrician to monitor the progress of your pregnancy.
Having an underactive thyroid can lead to miscarriage in the first three months of pregnancy. During pregnancy, it can affect your baby’s development. Later on in pregnancy, an underactive thyroid can increase your chance of getting pre-eclampsia, or your baby may be born too soon. But you’ll be monitored regularly to aim to prevent these effects.
You can take levothyroxine if you’re pregnant. It’s important to have the right amount of thyroid hormones in your bloodstream during pregnancy. While you’re pregnant, your body usually needs more thyroid hormones than usual. Because of this, your doctor may need to increase the amount of levothyroxine you take. After your baby is born, the amount of levothyroxine you need to take should go down again.
Diet and underactive thyroid
You don’t need to follow any special diet if you have an underactive thyroid – just aim to eat a healthy diet. If you’re taking levothyroxine, some foods may affect how well this medicine is absorbed into your body – ask your doctor or pharmacist for advice.
No specific food supplements can help to treat an underactive thyroid. In fact, some food supplements (such as iron or calcium) may affect how well your thyroid gland is working and the result of any thyroid blood tests. So if you have an underactive thyroid, speak to your doctor or a pharmacist before you take any food supplements.
Most people with an underactive thyroid gland put weight on. But this can get better with treatment. Speak to your doctor if you’re worried this may happen to you. Weight can be affected by lots of things, such as your family history, diet, medicines and other medical conditions. So you may not always be able to lose the extra weight. To help you keep your weight within a healthy range, it’s important to eat a healthy diet and be active.
After treatment for underactive thyroid
Treatment for underactive thyroid raises the levels of thyroid hormone in your body. It’s important to make sure that these don’t get too high. If they do, you could develop symptoms such as:
- chest pain
- a racing heartbeat (palpitations)
- anxiety
- shaking (tremors)
- changes to your bowel movements – you may go more often
It’s important to have your thyroid hormone levels checked with blood tests every six weeks when you first start your treatment. After this, your GP will tell you when you need to have more blood tests.
If you get any of these symptoms, contact your GP.
Most people will feel much better once their hormone levels get back to normal. But it can take a few months for your symptoms to ease after starting treatment. Some people have persistent mild symptoms, such as tiredness.
For more information, see our treatment of underactive thyroid section.
If an underactive thyroid isn’t treated, it can lead to complications such as heart problems and fertility problems. But an underactive thyroid is usually easily treated with medicines to keep your thyroid hormone levels within the normal range. For more information, see our treatment of underactive thyroid gland section.
An underactive thyroid and hypothyroidism are the same. They both mean that your thyroid gland isn’t making enough thyroid hormones to keep you healthy. For more information, see our about underactive thyroid section.
Hypothyroidism (underactive thyroid) won’t go away on its own. But it can be easily treated with medicines that get your thyroid hormone levels back to normal. You will need to take these medicines for life. For more information, see our treatment of underactive thyroid section.
Hypothyroidism (underactive thyroid) can make you feel very weak and tired and affect your mood. You may feel the cold more easily and have aching muscles and joints. For more information on other signs and symptoms of an underactive thyroid, see our symptoms of underactive thyroid section.
Heavy periods (menorrhagia)
Overactive thyroid (hyperthyroidism)
If you have an overactive thyroid (hyperthyroidism), it means your thyroid gland is making too much thyroid hormone.
Tips for a healthy and well-balanced diet
A healthy, well-balanced diet involves eating foods from a variety of food groups to get the nutrients that your body needs to function.
Did our Underactive thyroid (hypothyroidism) information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Primary hypothyroidism. BMJ Best practice. bestpractice.bmj.com, last reviewed February 2023
- Thyroid. Oxford Handbook of Endocrinology and Diabetes. 4th ed. Oxford Academic (online). academic.oup.com, published November 2021
- Metabolism. Encyclopaedia Britannica. www.britannica.com, last updated March 2023
- Hypothyroidism. Medscape. emedicine.medscape.com, updated May 2022
- Hypothyroidism. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised May 2021
- Hypothyroidism. Patient. patient.info, last reviewed February 2020
- Levothyroxine sodium. NICE British National Formulary. bnf.nice.org.uk, last updated March 2023
- Hypothyroidism. NICE British National Formulary. bnf.nice.org.uk, last updated March 2023
- Chiovato L, Magri F, Carlé A. Hypothyroidism in Context: Where We've Been and Where We're Going. Adv Ther 2019; 36(Suppl 2):47–58. doi: 10.1007/s12325-019-01080-8. Epub 2019 Sep 4. PMID: 31485975; PMCID: PMC6822815
- Levothyroxine interactions. NICE British National Formulary. bnf.nice.org.uk, last updated March 2023
- Thyroid and diet factsheet. British Thyroid Foundation. www.btf-thyroid.org, accessed March 2023
- Personal communication, Dr Amilia Alifrangis, Lead Physician at Bupa Health Clinics, August 2023
- Personal communication, Dr Raja N R Padidela, Consultant in Paediatric and Adolescent Endocrinology, August 2023



