Kidney infection (pyelonephritis)
- Dr Richard Hull, Consultant in Renal Medicine
A kidney infection is also known as pyelonephritis. It can develop if you have a urinary tract infection (UTI) and bacteria travel up to one or both of your kidneys. A kidney infection can make you feel unwell, but is usually easily treated with antibiotics.
About kidney infection
Your kidneys do a number of important jobs. They ‘clean’ your blood by filtering out water and waste products to make pee (urine). They also control your blood pressure and the amount of fluid in your body.
Doctors call kidney infections acute pyelonephritis. ‘Acute’ just means it is a short-term, rather than a long-term, kidney problem. Pyelonephritis means inflammation at the centre of the kidney.
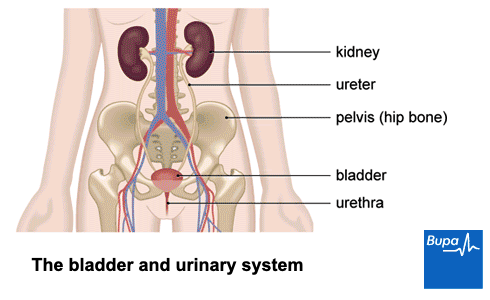
Kidney infections usually develop from an infection in your lower urinary tract. This includes:
- your bladder
- your urethra (the tube that carries urine out of your body)
Urinary tract infections normally start in your urethra. They can then travel to your bladder, causing an infection known as cystitis, and then up to your kidneys causing kidney infection.
You can also develop a kidney infection from bacteria in your bloodstream. This might be more likely if something is blocking your urethra. This may be because you have a kidney stone or in men who have an enlarged prostate.
Symptoms of a kidney infection
Kidney infection symptoms can develop quickly. Signs of kidney infection may include:
- pain in your back or sides (it may be only on one side)
- a fever (a high temperature) and chills
- feeling sick or being sick
- generally feeling unwell with flu-like symptoms
You may have symptoms of a lower urinary tract infection (cystitis) before you get a kidney infection. These may include:
- needing to pee urgently
- burning or stinging when you pee
- blood in your urine
If you have any of these symptoms, contact your GP.
Causes of kidney infection
E coli is the most common type of bacteria in kidney infections (pyelonephritis), causing up to 8 out of 10 cases. Other types of bacteria can also cause them.
The bacteria travel up to your bladder through your urethra (the tube that carries urine out of your body). They can then travel up from your bladder to infect one or both kidneys. In about 1 in 20 cases, bacteria reach the kidneys through your bloodstream, from an infection somewhere else in your body.
Kidney infections are more common in women than in men. You're more likely to develop a kidney infection if:
- you have an underlying condition affecting your kidney or urinary tract
- you have a catheter – a medical tube that takes urine out of your body from your bladder
- your ureter or kidney is blocked – for example, by a kidney stone or an enlarged prostate gland
- you’re pregnant
- you have diabetes
- your immune system is weakened – for example, if you have HIV/AIDS, cancer or are taking steroids
- you have urinary incontinence
- you have sex often or have had a new partner recently
Diagnosis of kidney infection
Your GP will ask you about your symptoms and medical history. They’ll examine you and ask you to give a urine sample. Your GP may test the urine sample in the surgery, to look for signs of infection. This is sometimes called a ‘dipstick’ test. Or, they may send a urine sample to a laboratory to look for infection and find out which type of bacteria is causing it.
To assess your condition further, your GP may arrange other tests. These could include blood tests or a scan, such as a renal ultrasound or a CT scan.
GP Subscriptions – Access a GP whenever you need one for less than £20 per month
You can’t predict when you might want to see a GP, but you can be ready for when you do. Our GP subscriptions are available to anyone over 18 and give you peace of mind, with 15-minute appointments when it suits you at no extra cost.
Self-help for kidney infection
If you have a kidney infection (pyelonephritis), it’s important to make sure you keep hydrated. So you need to drink enough fluids to prevent dehydration. It’s often said that we need 8 to 10 glasses or mugs a day. But how much you need varies depending on your body size – so if you’re large you may need more – aim for about 20 to 30mls per kilogram of body weight. Drinking water is a good way to stay hydrated. But all fluids count, including tea, coffee and even soup, so drink what you feel like having. One way to tell if you’re hydrated is to check the colour of your urine – it should be very pale yellow (straw-coloured).
It’s also important to get plenty of rest. Don’t try to do too much while you’re feeling unwell and recovering. If you need to, you can take over-the-counter painkillers.
Treatment of a kidney infection
Medicines
If urine tests show you have a kidney infection (pyelonephritis), your GP will prescribe antibiotics. You’ll need to take these for one to two weeks. Your doctor and pharmacist will tell you exactly how long.
Most people with kidney infection respond well to antibiotics and make a good recovery. The time it takes for your infection to go depends on how severe it was to begin with – it can be days or weeks. It’s important to complete the full course of antibiotics, even if your symptoms clear up before you finish them. This helps to stop the infection from coming back.
Some people may need further treatment in hospital. Your GP will tell you if you need to go to hospital. You should contact your GP if your kidney infection symptoms get worse, particularly if you feel sick or start vomiting. Or if your symptoms don’t start to get better within 48 hours (two days) of starting the antibiotic.
Hospital treatment
Your GP may refer you to hospital for treatment if they think you’re at high risk of developing complications. This might be for any of the following reasons.
- You have signs of a more serious condition such as sepsis. Signs include becoming increasingly unwell, a very high fever, sweating, shivering, becoming pale, shortness of breath and dizziness.
- You’re pregnant.
- You are very dehydrated, can’t drink or can’t take medicines.
- There are other underlying health problems, such as diabetes or kidney disease.
- You keep getting urinary tract infections (UTIs).
In hospital, you may have a drip put into a vein in your hand or arm to give you fluids and antibiotics. If all goes well, after a couple of days you can usually switch to antibiotics by mouth. For more about who may need hospital treatment, see our section on complications.
Complications of kidney infection
In most people, kidney infection (pyelonephritis) clears up easily with treatment. But sometimes an infection can become serious and even life-threatening. Complications include the following.
- Resistance to antibiotics. Your doctor may need to try a different antibiotic, and you may develop further infections.
- An abscess (a collection of pus) in your kidney. You may need a procedure to drain it.
- Damage to your kidney. This can be permanent and lead to kidney failure.
- Sepsis (blood poisoning) – this can happen if bacteria get into your blood. If this happens, you’ll need to be admitted to hospital for treatment.
You're more likely to develop complications if you:
- have a severe infection
- have type 1 or type 2 diabetes
- are over 65
- have a long-term infection that’s not responding to treatment
- have an underlying condition affecting your kidney or urinary tract
- have a catheter (medical tube that takes urine out of your body from your bladder)
- have a weakened immune system – for example, if you have HIV/AIDS or cancer
- have kidney stones
- are pregnant
If you're pregnant and you develop a kidney infection, it can lead to complications for you and your baby. These include your baby being born early and being born small. If you have any of the symptoms of a kidney infection and you’re pregnant, contact your GP or midwife as soon as possible. This is really important even if your infection is mild.
Prevention of kidney infection
Some people keep getting kidney infections or urinary tract infections (UTIs). If you do, your doctor may prescribe antibiotics to help prevent them. How long you need to take them for will depend on your personal circumstances.
Kidney infections usually develop following a urinary tract infection. To help stop UTIs from developing you can try these self-help tips.
- Drink enough fluids to stay hydrated.
- Don’t delay passing urine (peeing) – always go as soon as you feel the urge.
- Go to the toilet to pee after having sex.
- Wipe from front to back after using the toilet, to avoid spreading bacteria from your anus.
- Don’t ‘douche’ (flush out the vagina with water or any other fluids).
- If you have an enlarged prostate, try to make sure you’ve completely emptied your bladder. If necessary, try peeing again a few minutes after you’ve been to the toilet.
Researchers have looked into preventing UTIs with cranberry products (cranberry juice or cranberry supplements). Doctors also sometimes recommend a fruit sugar called d-mannose. There is now some evidence that both d-mannose and cranberries can help to prevent UTIs. So if you’re prone to bladder infections, they may help. But if you already have symptoms of an infection, it’s important to see your doctor and get some antibiotics.
Kidney infection symptoms can include:
- back or side pain
- feeling or being sick
- a high temperature with shivering
- muscle aches and pains
You may also need to pass urine (pee) more often, urgently, and feel pain when you pee. For more information, see our section on symptoms of kidney infection.
Most kidney infections are caused by bacteria travelling up the tube that carries urine out of your body (the urethra). You can also get an infection if bacteria enter your kidneys via your bloodstream from an infection elsewhere in your body. See our section on causes of kidney infection for more information.
To see if you may have a kidney infection, your GP will ask you for a urine (pee) sample to be sent off and tested for bacteria. Sometimes, you may need blood tests or a scan. For more information on this, see our section on diagnosis of kidney infection.
If you have signs of a kidney infection, it’s very important to see your doctor. An untreated infection could become serious and damage your kidneys. You are likely to need antibiotics. See our section on treatment of kidney infections for more information.
Most kidney infections are easily treated with antibiotics and don’t become severe. But any infection can become more serious if not treated. Some people are more prone to a severe infection, for example pregnant women and people with lowered immunity. See our section on complications of kidney infections for more information.
There are several possible causes of kidney infections. They are more common in women, especially during pregnancy. They’re also more common if you have diabetes. A blockage of the urinary tract can also increase risk, such as an enlarged prostate or kidney stones. For other factors that can increase risk, see our section on causes of kidney infections.
Antibiotics
Kidney stones
Kidney stones (or calculi) are hard stones that can form in one or both of your kidneys
Keeping hydrated
We explain why you need to drink enough and offer some tips to help you stay hydrated
Other helpful websites
Discover other helpful health information websites.
Did our Kidney infection (pyelonephritis) information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Acute pyelonephritis. BMJ Best Practice. bestpractice.bmj.com, last reviewed May 2023
- Pyelonephritis – acute. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised May 2023
- Human excretion. Encyclopaedia Britannica. britannica.com, accessed June 2023
- Kidney infection. BMJ Best Practice. bestpractice.bmj.com, published September 2021
- Chronic pyelonephritis. BMJ Best Practice. bestpractice.bmj.com/topics/en-gb/552, last reviewed May 2023
- Pyelonephritis. Patient. patient.info, last updated January 2022
- Kidney Infection. MSD Manuals. msdmanuals.com, last reviewed December 2022
- The importance of hydration. British Dietetic Association. bda.uk.com, published August 2019
- Personal communication, Dr Richard Hull, Consultant Nephrologist, June 2023
- What should older people drink? British Dietetic Association. bda.uk.com, published April 2021
- Urinary tract infections in pregnancy. Medscape. emedicine.medscape.com, last updated 8 October 2019
- Urinary Tract Infections in Pregnancy. Medscape. emedicine.medscape.com, last updated August 2021
- Oxford Handbook of General Practice (5 ed). Oxford Medicine Online. academic.oup.com, published June 2020
- Urinary tract infection (lower) – women. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised March 2023
- Prostate Symptoms. British Association of Urological Surgeons. baus.org.uk, accessed June 2023
- Williams G, Hahn D, Stephens JH, et al. Cranberries for preventing urinary tract infections. Cochrane Database of Systematic Reviews 2023, Issue 4. Art. No.: CD001321. DOI: 10.1002/14651858.CD001321.pub6, published April 2023
- De Nunzio C, Bartoletti R, Tubaro A, et al. Role of D-Mannose in the prevention of recurrent uncomplicated cystitis: State of the art and future perspectives. Antibiotics (Basel) 2021; 10(4):373. doi: 10.3390/antibiotics10040373, published April 2021
- Liz Woolf, Freelance Health Editor



