Colposcopy
- Dr Karin Hellner, Consultant in Gynaecology and Lead Colposcopist
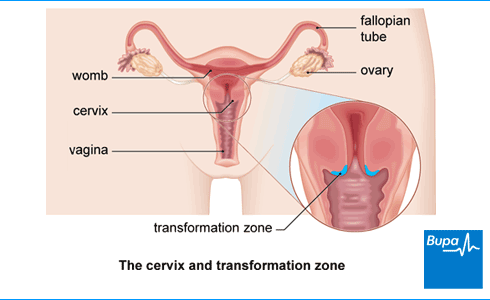
A colposcopy is a simple examination to have a detailed look at your cervix (the neck of your womb) and vagina. It can help to find abnormal cells that may be likely to turn into cancer. These cells may then be removed or treated.
Why would I need to have a colposcopy?
You’ll be offered a colposcopy if your cervical screening test (smear test) has shown that you may be at an increased risk of cervical cancer.
Cervical screening is offered to anyone with a cervix and aged between 25 and 64 in the UK. It involves taking a sample of cells from your cervix in the area where most abnormal cell changes are seen (the transformation zone). The cells are tested for HPV (human papillomavirus). This virus can cause abnormal changes in the cells in your cervix. If the test is positive for HPV, the sample will also be checked for abnormal cell changes.
You may be offered a colposcopy for one of the following reasons.
- You’ve tested positive for HPV infection and your sample also shows some abnormal cell changes.
- You’ve tested positive for HPV infection, and it hasn’t gone away after two years – even if you haven’t had abnormal cell changes.
- You’ve had two cervical screening tests in a row that didn’t give a result. These test results are called ‘inadequate’. Inadequate means the cells aren’t clear enough to look at, or there’s been a problem with the way the sample was taken.
- The nurse or doctor who carried out your cervical screening test didn’t think your cervix looked as healthy as it should do.
- You’ve had symptoms of cervical cancer and have been referred for a colposcopy by your doctor.
A colposcopy allows a doctor or nurse to have a closer look at abnormal cells in your cervix. It can help to identify cells that may be more likely to develop into cancer. Your doctor or nurse may also be able to remove or treat abnormal cells during the colposcopy.
Preparing for colposcopy
If you’re invited for a colposcopy, you’ll be given information to explain:
- what will happen during your appointment
- if you’re likely to need any treatment during your colposcopy
A colposcopy is usually done in a colposcopy clinic as an out-patient procedure. This means you have the examination and go home on the same day. If you would prefer a female nurse or doctor to carry out your colposcopy, you should contact your clinic to request this.
If you think you may have your period on the day of your colposcopy, contact your clinic. You may still be able to have the colposcopy during your period. But some clinics may prefer to rearrange your procedure for another time.
If you’re pregnant or think you could be, let the clinic know before your appointment. It’s usually still fine to have a colposcopy during pregnancy, but it’s important that the clinic knows. If you need treatment as part of your colposcopy, they may advise you to delay it until after you’ve had your baby.
You can eat and drink as usual before a colposcopy. Follow any advice you’ve been given by your clinic. You may be advised not to:
- have sex for at least 24 hours before your appointment
- use creams or lubricants in your vagina in the 24 hours beforehand
You may want to bring a panty liner or sanitary pad to use afterwards. This is because you’re likely to have some discharge or light bleeding.
A colposcopy can be a bit uncomfortable, especially if you need to have a biopsy as well. Some people find it a little painful. Your colposcopist may recommend that you take paracetamol or ibuprofen an hour before your appointment. You may be able to have a local anaesthetic – discuss this with your colposcopist before your procedure.
What happens during a colposcopy?
When you get to the clinic, you’ll meet the doctor or nurse carrying out your colposcopy (the colposcopist). They’ll talk to you about why you’ve been invited for a colposcopy and what to expect. Tell your colposcopist if you’re feeling nervous or worried. They’ll be able to reassure and support you.
Once you’re ready, your colposcopist will give you a private area where you can undress from the waist down. They may give you a paper sheet to cover yourself with. You’ll need to lie on your back on the bed with your feet drawn up and your knees bent and apart. There may be supports for your legs or feet.
A colposcopy usually takes around 5 to 10 minutes. If you’re having treatment as well, the whole procedure may take around 10 to 20 minutes.
During the procedure, your colposcopist will:
- use a special tool called a speculum to hold open your vagina
- usually put special solutions on the surface of your cervix to show up any abnormal cells more clearly
- use a colposcope (a special type of microscope) to have a detailed look at your cervix
The colposcope will stay outside your body the whole time. Your colposcopist will look through the colposcope and get a close-up view of the cells in your cervix.
During the examination, your colposcopist may take a biopsy (small piece of tissue) from your cervix to be tested. The biopsy will be sent to a laboratory for testing and the results sent to your doctor.
Let your colposcopist know if you have any discomfort, and they’ll try to make it more comfortable for you.
Colposcopy treatments
If your colposcopy finds abnormal cells, you may be offered treatment to remove them. Whether or not you’re offered treatment depends on the ‘grade’ of the cells. This relates to how likely the cells are to develop into cancer.
If your colposcopist can tell that you need treatment during your colposcopy, they may be able to remove the cells straightaway. This is called a ‘see-and-treat’ appointment. Your clinic should tell you before your appointment if this is likely, and explain what your treatment will involve. You’ll need to give your consent beforehand, so talk to your colposcopist if there’s anything you’re unsure about. If you have abnormal cells but don’t have treatment at your first colposcopy appointment, you’ll be invited back for a second appointment at another time.
The treatment you’re offered will depend on several things. These include:
- how severe the changes in your cells are
- how far into your cervix they go
The main types of treatment include the following.
LLETZ
LLETZ stands for ‘large loop excision of the transformation zone’. It is the most common treatment. It uses a small wire loop with an electric current passing through it, to remove the abnormal cells from your cervix. You’ll usually have this treatment under local anaesthesia. This means you’ll be awake but the area being treated will be numb.
NETZ or SWETZ
NETZ (needlepoint excision of the transformation zone) and SWETZ (straight wire excision of the transformation zone) are similar to LLETZ. But instead of a small wire loop, a needle or straight wire is used to cut away the tissue. You may have one of these procedures if the abnormal cells are deeper into your cervical canal.
Cone biopsy
A cone biopsy is a minor operation to remove a cone-shaped piece of tissue from your cervix. It’s done under general rather than local anaesthesia. This means you’ll be asleep during the procedure, and you may need to stay in hospital overnight.
Other treatments
Sometimes other treatments are used to get rid of abnormal cells. These aren’t used as often, but they include the following.
- Cryotherapy. This involves freezing the affected area of your cervix to destroy the abnormal cells.
- Laser treatment (or laser ablation). This treatment uses a laser to burn away abnormal cells.
- Cold coagulation. Despite the name of this procedure, it involves using a heated probe to destroy any abnormal cells.
What to expect after a colposcopy
How you’ll feel after your colposcopy will depend on whether you’ve had:
- only a colposcopy examination
- a colposcopy biopsy procedure
- colposcopy treatment
After a colposcopy, you’ll usually be able to go home as soon as you feel ready. You may feel well enough to go about your normal day-to-day activities – including driving and light exercise – straight away. But take some time to rest if you need to. If you’ve had treatment, you may have some pain for a couple of days afterwards. This may feel a bit like period pain. You can take over-the-counter painkillers for this.
You may have some spotting and light discharge for around one to two days after your colposcopy, especially if you had a biopsy. If you had treatment, you may have heavier bleeding for up to four weeks. You may also notice discharge from your vagina that looks a bit like coffee granules. This is normal as you start to heal. But if your bleeding is very heavy or your vaginal discharge has an unusual smell, you should speak to your GP. For more details, see our section on complications of colposcopy.
Until any bleeding or discharge has stopped, you shouldn’t:
- have sex
- use tampons
- swim
- use any medications, creams, or lubricants in your vagina
Colposcopy biopsy results
Your colposcopist may be able to tell you straight away if they found anything during their examination. But if you had a biopsy, this will need to be sent to a laboratory for testing. You’ll usually receive your biopsy results within about four weeks, but it can sometimes take a bit longer. These may be sent to you in the post, or you may be contacted by the clinic. Your doctor will also tell you if they recommend any further treatment.
It’s natural to worry about your colposcopy test results. Most people who have a colposcopy don’t have cervical cancer. A colposcopy may show that you have some abnormal cells in your cervix. These cells may be more likely than normal cells to develop into cancer. If you have abnormal cells, these may go away on their own, or they can be treated or removed.
Complications of colposcopy
Complications are problems that may occur during or after your colposcopy. The most common complications of colposcopy include the following.
- Pain in your tummy (lower abdomen) or pelvis. You’re likely to get some pain for a couple of days. But if it continues or is severe, speak to the clinic or your GP.
- Heavy bleeding. Some bleeding is normal after a colposcopy, especially if you have treatment. But if it gets particularly heavy or doesn’t go away, you should contact your GP.
- Infection. This can be a risk if you’ve had a treatment such as LLETZ. Signs of an infection include:
- vaginal discharge that looks different from normal or has a strong smell
- a fever (high temperature).
Some of the different treatments have particular risks too. Your colposcopist will discuss these with you before you agree to any treatment.
Worried about your gynaecological health?
Get a picture of your current health and potential future health risks with one of our health assessments.
To book or to make an enquiry, call us on 0370 218 8122
A colposcopy is a procedure to have a close look at your cervix. It can check for abnormal cells and if these are likely to turn into cancer. Abnormal cells can then be treated or removed to reduce your risk of cancer. For more information, see our section: Why would I need to have a colposcopy ?
A colposcopy tests for abnormal cells in your cervix. It can check if these cells are likely to turn into cervical cancer. For more information, see our section: Why would I need to have a colposcopy ?
A colposcopy can rule out cancer. It will show if you have abnormal cells in your cervix. These cells may be more likely to develop into cancer. For more information, see our section: Why would I need to have a colposcopy ?
You may be offered a colposcopy if you’ve had an abnormal cervical smear test result. This could mean you’re at higher risk of cervical cancer. You may also be referred for a colposcopy if you’ve had symptoms of cervical cancer. For more information, see our section: Why would I need to have a colposcopy ?
It’s natural to feel a little worried if you’ve been invited for a colposcopy. But it’s rare for a colposcopy to find cervical cancer. The abnormal cells may go away on their own. Or they may be treated or removed. For more information, see our section on what to expect after a colposcopy .
Some people feel a little discomfort during a colposcopy. But it’s more likely to feel uncomfortable than painful. If you do feel any pain, let your colposcopist know. For more information, see our section on what to expect after a colposcopy .
Cervical cancer
Cervical screening
Other helpful websites
Discover other helpful health information websites.
Did our Colposcopy information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Colposcopy and cervical treatments. Patient. patient.info, last updated January 2023
- Cervical screening: having a colposcopy. NHS England. www.gov.uk, updated August 2022
- Cervical screening: programme overview. Public Health England. www.gov.uk, updated March 2021
- What is cervical screening? Public Health Wales. phw.nhs.wales, accessed August 2023
- Cervical screening: programme and colposcopy management. Management and referral guidelines for colposcopy. HrHPV tests and results. NHS England. www.gov.uk, updated January 2023
- About colposcopy. Jo’s Cervical Cancer Trust. www.jostrust.org.uk, last updated May 2020
- Your colposcopy appointment. Jo’s Cervical Cancer Trust. www.jostrust.org.uk, last updated July 2020
- Treatment at colposcopy. British Society for Colposcopy and Cervical Pathology (BSCCP). www.bsccp.org.uk, accessed August 2023
- Treatment if you have abnormal cervical cells. Cancer Research UK. www.cancerresearchuk.org, last reviewed March 2020
- Anaesthesia explained. Types of anaesthesia. Royal College of Anaesthetists. www.rcoa.ac.uk, published March 2021
- General anaesthesia. Patient. patient.info, last updated August 2023
- After your treatment for abnormal cervical cells. Cancer Research UK. www.cancerresearchuk.org, last reviewed March 2020
- What you should expect after treatment. British Society for Colposcopy and Cervical Pathology (BSCCP). www.bsccp.org.uk, accessed August 2023
- Personal communication by Dr Karin Hellner, Consultant Gynaecologist, September 2023
- Victoria Goldman, Freelance Health Editor



