Cervical screening (smear test)
Please note, this topic page has gone past its three year review date. We review our content every three years to ensure we meet the highest standards in health information. The review of this page will be live shortly.
- Ms Shanti Raju-Kankipati, Gynaecologist
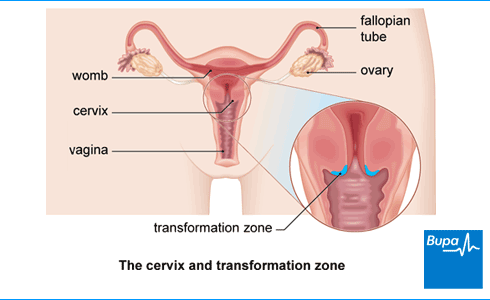
Cervical screening (a smear test) is a test to see if your cervix, which is the neck of your womb, is healthy. The test involves collecting a sample of cells, which are tested for the human papilloma virus (HPV). If you have HPV, the sample will be tested for any changes in your cells that can be caused by the virus. These changes could develop into cervical cancer.
About cervical screening
Cervical screening is commonly known as a smear test. You might have heard the term ‘Pap smear’, which is what people call it in the USA and in many European countries.
Screening means testing for early signs of an illness before you have symptoms. Cervical screening works really well to prevent cervical cancer – it saves thousands of lives every year. So it’s important to attend regular screening when you’re invited.
In cervical screening, a nurse or doctor will take a sample of your cells and test for high-risk types of the human papillomavirus (HPV). HPV infection is the main cause of cervical cancer. HPV infections are really common and most people get HPV at some point in their lives. Usually, your body will get rid of the infection and you won't know that you had the virus.
If you don’t have HPV, you’re very unlikely to have abnormal cells or to develop cervical cancer. This means the cells in the sample won’t be examined further.
If an HPV test finds that you have HPV, your cell sample will be checked for any abnormal changes that could potentially develop into cancer in the future.
Any abnormal cells can be either monitored or treated to stop cervical cancer developing.
NHS cervical screening programme
The NHS runs a national cervical screening programme in the UK for all women aged 25 to 64.
If you’re in this category, your GP surgery will invite you for cervical screening. If you’re a trans man (with a cervix), you can also have screening. But if you’re registered as a man with your GP, you won’t be invited automatically. You can ask your GP or a local sexual health or family planning clinic to add you to the cervical screening list.
If you’re aged between 25 and 64 and registered with a GP, you’ll be invited for screening every three or five years. This will depend on your age and where you live.
You don’t have to have the test at a GP surgery. You can also have one at a family planning or sexual health clinic or at a private clinic.
At the moment, doctors don’t screen women under 25. Cervical screening doesn’t work as well in women under this age. It’s common to have changes in the cells of your cervix when you’re younger but cervical cancer at this age is extremely rare. Treating these changes unnecessarily could lead to issues later on.
If you’re 65 or over, you’re very unlikely to develop cervical cancer if your last screening results were normal. But if you’ve never had cervical screening, or haven’t had a test since you were 60, you’re entitled to one.
Cancer awareness: cervical cancer
Cervical cancer awareness| Screening | Watch in 1:20 minutes
This animation explains the importance of attending cervical cancer screening so that if you have cervical cancer it can be detected early.
Who needs to have cervical screening?
Women who’ve had any type of sexual contact with men or women (including touching or using sex toys), should have cervical screening. Even if you haven’t had sex for years, you should still attend screening. This is because you may have come into contact with the human papilloma virus (HPV) from a previous partner, months or even years ago. The virus can be inactive and cause abnormal cells later on.
If you’ve had the HPV vaccine, it’s still best to go for your screening appointments. The HPV vaccine protects against the two types of HPV that cause most cases of cervical cancer. But it doesn't protect against other types of HPV that are also linked with cervical cancer.
If you’ve never had any sexual contact, your risk of HPV is small but you may decide to still have regular screening. And if you have any unusual bleeding or discharge, see your GP.
If you’ve had a hysterectomy, you won’t need screening unless your cervix wasn’t removed. Ask your GP for more information.
At any age, if you get symptoms such as bleeding after sex or have an unusual discharge, see a GP. You should also see your GP if you get bleeding after menopause.
Cervical screening and pregnancy
If you're pregnant and have previously had normal screening tests, you can delay routine screening until three months after your baby is born. But check with your doctor or midwife.
If you’ve had an abnormal test before you became pregnant, you may need to have a colposcopy. A colposcopy is a test that uses a magnifying instrument called a colposcope to examine your cervix. Ask your doctor or midwife what’s best for you.
Preparing for a cervical screening test
It’s best to have your cervical screening test when you’re not on your period. If you’re bleeding, the sample probably won’t be clear and you may need to have the test again.
For two days before your test, don’t use any spermicide (including condoms coated with spermicide), lubricating jelly or vaginal creams. This is because chemicals in these products can affect the test.
What happens during a cervical screening test?
When you go for your cervical screening test, your appointment will usually last about 10 minutes. But the actual test only takes a minute or two. Usually, a female nurse or doctor will do your test, but if you want to make sure, ask when you make your appointment.
Your nurse or doctor will ask you to take off your clothes (just your bottom half) but if you’re wearing a skirt you can just take your underwear off. They’ll then ask you to lie on your back on an examination couch with your knees bent and apart. If you can’t manage this easily, tell your nurse – you may be able to lie on your side instead.
Your nurse or doctor will use an instrument called a speculum (pronounced speck-you-lum) to gently open your vagina, so they can see your cervix (neck of your womb). They’ll then use a small, soft brush to take a sample of cells from your cervix. They’ll send this sample to a lab to be tested.
Some women find the test uncomfortable but it doesn’t usually hurt. If it does hurt, let your nurse know so they can try and make you more comfortable. Try to relax – the more relaxed you are, the less discomfort you’ll feel. You might find it helps to take some deep breaths, listen to music or watch something on your phone.
What to expect afterwards
You can usually carry on as normal straight away after your screening test. You might bleed a bit afterwards so you may want to use a sanitary pad. Your cervix is a sensitive area so even though a soft brush is used to take the sample, it can bleed even if it’s touched lightly. If you have heavy bleeding or pain, see your GP.
How healthy are you?
With our health assessments you get an action plan that’s tailor-made for you.
To book or to make an enquiry, call us on 0345 600 3458
Cervical screening results
Your nurse or doctor will let you know when you can expect your cervical screening results. They’re usually sent to the surgery or clinic where you had the screening test, as well as to your home address. Your results should be ready within two to six weeks. If you get an abnormal result, it doesn’t mean you have cancer.
Your human papilloma virus (HPV) test result will fall into one of the following categories.
You don’t have HPV
If you don’t have HPV, you’re extremely unlikely to have abnormal cells or to develop cervical cancer. This means the cells from your sample won’t be examined further. You’ll be invited back for screening in three or five years’ time, depending on your age and where you live.
You have HPV but no abnormal cells
If your screening test shows you have HPV but normal cervical cells, you’ll be asked to have another test (usually a year later but your results letter will say when). This is to see if the infection has gone. Your immune system will usually clear HPV. If cervical screening shows that you have HPV but no abnormal cells three times in a row, your doctor will refer you to have a colposcopy for more tests.
You have HPV and borderline or mild changes
If your test result says that you have cells with ‘borderline’ or ‘mild’ changes, you’ll have more tests. Although these mild changes rarely develop into cancer and may well return to normal by themselves, they need to be checked. You’ll be offered a further test called a colposcopy to look at your cervix more closely. This is usually within six weeks.
You have HPV and moderate or severe changes
If your test result says that you have cells with ‘moderate’ or ‘severe’ changes, it still means you don’t have cancer. But cells with these changes are less likely to return to normal on their own so you may need treatment. You’ll be offered a colposcopy to examine your cervix, usually within two weeks, to see if you do need treatment.
An inadequate result
Sometimes the result may be 'inadequate' or 'unsatisfactory' because there weren’t enough cells in the sample or the cells couldn’t be seen clearly. If this happens, you’ll be asked to have another test after three months.
It may worry you if you have high-risk HPV and/or abnormal cells. If you’re concerned about your results or don’t understand the wording in your results letter, arrange to speak to your GP who can explain them.
Treatment of abnormal cervical cells
IIf your screening test shows abnormal cells, you’ll be asked to have a more detailed test called a colposcopy. If your colposcopy shows an area of your cervix that looks abnormal, the doctor will take a biopsy. This is a small sample of the abnormal tissue that is sent to a lab to be examined.
Depending on the result, you may need to have treatment to either remove or destroy the abnormal cells. The usual way to do this is with a large-loop excision, also known as loop excision or loop diathermy. In this procedure, your doctor uses a wire loop with an electric current to remove the abnormal cells from your cervix.
You’ll usually have this treatment under local anaesthesia so you’ll be awake but won’t feel any pain. General anaesthesia (where you are asleep) may also be an option under some circumstances – ask your nurse or doctor for advice.
Other treatments that can destroy abnormal cells include:
- laser therapy
- cryotherapy (freezing)
- cold coagulation (which actually uses heat to destroy the cells)
Ask your nurse or doctor for more information about these.
Cervical screening (a smear test) tests a sample of cells from your cervix for an infection with a virus called the human papilloma virus (HPV). If you have a certain high-risk type of HPV, you’ll then be tested for any changes in the cells. These changes could later develop into cervical cancer.
For more information, see our section about cervical screening.
A Pap smear is what people in the USA call cervical screening. As in the UK, a health professional will take a sample of cells from your cervix. In the USA, the sample will be tested first for any changes to the cells, then tested for HPV.
A smear test is another name for cervical screening – they are the same thing. A sample of cells is collected from your cervix and tested for an HPV infection. If you have HPV, the sample will be tested for any changes in your cells.
For more information, see our section about cervical screening.
Cervical screening isn’t usually painful but you may find it uncomfortable. If it is painful, let your nurse know. And try to relax because the more relaxed you are, the less discomfort you’ll feel. You might find it helps to take some deep breaths or distract yourself by listening to some music on your phone.
If you’re registered with a GP, you’ll be invited and start cervical screening from the age of 25. Doctors don’t think it’s helpful to screen women under this age. It’s common to have changes in the cells of your cervix when you’re younger but cervical cancer at this younger age is extremely rare. Treating these changes unnecessarily could lead to issues later on.
For more information, see our section on the NHS cervical screening programme.
If you’re aged between 25 and 64 and registered with a GP, you’ll be invited for screening every three or five years. It depends on your age and where you live in the UK because the different UK nations have slightly different screening programmes. Check what’s available to you. You might get invited earlier if your previous smear showed HPV or abnormal cells.
For more information, see our section on the NHS cervical screening programme.
Cervical cancer
Colposcopy
Did our Cervical screening (smear test) information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Cervical screening: helping you decide. NHS England. www.gov.uk, updated 30 September 2024
- Cervical screening. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised September 2022
- Mansour T, Limaiem F. Cervical screening. StatPearls Publishing. www.ncbi.nlm.nih.gov, last updated 8 August 2023
- Guidance. 1. Introduction and programme policy. NHS England. www.gov.uk, updated 27 September 2024
- Cervical cancer and HPV. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised February 2022
- Ceasing and deferring women from the NHS cervical screening programme. NHS England. www.gov.uk, updated 27 September 2024
- Adult screening programme. Cervical cancer. UK National Screening Committee. view-health-screening-recommendations.service.gov.uk, accessed 15 October 2024
- Human papillomavirus (HPV) infection. MSD Manuals. msdmanuals.com, reviewed/revised January 2023
- Immunizations – childhood. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised July 2024
- Management of cases relating to pregnancy, menopause, contraception and hysterectomy. NHS England. www.gov.uk, updated 27 September 2024
- Colposcopy. Cancer Research UK. www.cancerresearchuk.org, last reviewed 15 September 2023
- About cervical screening. Cancer Research UK. www.cancerresearchuk.org, last reviewed 8 September 2023
- Topics 7 and 8: Anatomy, physiology, and taking cervical samples. NHS England. www.gov.uk, updated 10 October 2024
- Cervical screening results. Cancer Research UK. www.cancerresearchuk.org, last reviewed 15 September 2023
- Management and referral guidelines for colposcopy. NHS England. www.gov.uk, updated 27 September 2024
- Cervical screening: having a colposcopy. NHS England. www.gov.uk, updated 23 July 2024
- Treatment if you have abnormal cervical cells. Cancer Research UK. www.cancerresearchuk.org, last reviewed 29 September 2023
- The Pap (Papanicolaou) test. American Cancer Society. www.cancer.org, last revised 27 February 2024
- Rachael Mayfield-Blake, Freelance Health Editor



