Hysteroscopy
- Dr Demetri Panayi, Consultant Obstetrician and Gynaecologist and Subspecialist Urogynaecologist
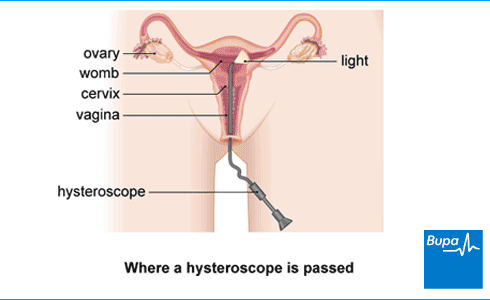
A hysteroscopy is a procedure to look inside your womb (uterus) to check for any problems. It uses a narrow tube containing a camera. This is called a hysteroscope. The hysteroscope is passed into your vagina, through the neck of your womb (cervix) and into your womb.
About hysteroscopy
You may have a hysteroscopy for several different reasons. Your doctor may recommend a hysteroscopy to check for problems with your vagina, your womb, or the lining of your womb. You may be able to have treatment during a hysteroscopy.
Reasons for having a hysteroscopy include the following.
- An ultrasound scan has found that the lining of your womb is thicker than it should be
- To find out what’s causing unusual bleeding from your vagina and/or womb. This can include heavy periods, bleeding between periods and bleeding after the menopause(postmenopausal bleeding).
- To check for growths in your womb such as polyps and fibroid and remove these if necessary.
- To investigate and treat developmental and structural differences in your womb. These differences are called Müllerian anomalies.
- To see any problems that might be making it difficult for you to get pregnant.
- To investigate repeated miscarriages.
- To break up and remove scar tissue in the lining of your womb.
- To take out an intra-uterine system (IUS) or coil that has no visible threads for removal or has moved out of position.
- To take an endometrial biopsy. This is a tissue sample to check for cancer in the lining of your womb (endometrial cancer).
If possible, your doctor or nurse will aim to treat any problems at the same time as the diagnosis. This means you won’t need a separate procedure. You’ll have:
- a diagnostic hysteroscopy if it’s investigating a problem
- an operative hysteroscopy if it involves treatment too
Your doctor will explain why they’re recommending a hysteroscopy. They’ll discuss the benefits and potential risks involved, as well as any alternatives. They should give you some written information to take away.
Preparation for hysteroscopy
You usually have a hysteroscopy as an out-patient procedure in a treatment room at a gynaecology unit. A specialist doctor (a gynaecologist) or specialist nurse carries out an out-patient hysteroscopy. You may be given a local anaesthetic injection to numb your cervix before your procedure. You may also be offered nitrous oxide (‘gas and air’) during the procedure. You won’t usually need a general anaesthetic. This means you’ll be awake for the procedure.
If you’re having your hysteroscopy in a hospital operating theatre, you may be offered:
- a general anaesthetic especially if you’re having a longer or more complicated procedure – this means you’ll be asleep during the operation
- a local anaesthetic to numb your cervix
- a spinal anaesthetic – the lower half of your body is numbed using an injection in your lower back
- sedation to make you feel relaxed
If you would prefer to have your procedure under general anaesthesia, you can discuss this with your gynaecologist. Whether you have a general anaesthetic or not, you’ll usually go home on the same day. But you shouldn’t drive or use public transport after a general anaesthetic, so you’ll need to arrange for someone to take you home.
Contraception and periods
Your doctor or hospital will tell you how to prepare for your hysteroscopy procedure. You won’t be able to have a hysteroscopy if you’re pregnant. If you have periods, it’s important to use contraception or not have sex between your last period and the test. You’ll be offered a pregnancy test on the day of your procedure.
Don’t worry if you’re bleeding on the day of your test. Your hysteroscopy can usually go ahead. But if the bleeding is heavy, your procedure may need to be delayed until your bleeding is lighter or has stopped.
Painkillers
Your hospital will usually recommend you take an over-the-counter painkiller, such as ibuprofen or paracetamol an hour or two before your hysteroscopy procedure. Make sure you have some painkillers at home for after the procedure. It’s also a good idea to have some sanitary pads ready for any bleeding.
Eating and drinking
If you’re having an out-patient hysteroscopy, you can eat and drink as normal before your procedure. If you’re having a hysteroscopy under general anaesthesia, the hospital will tell you when you need to stop eating and drinking before your procedure.
On the day
On the day of your procedure, you’ll meet the doctor or nurse who will be performing your hysteroscopy. They’ll discuss with you what will happen before, during and after your procedure, including any pain you might have. If you’re unsure about anything, don’t be afraid to ask. You’ll be asked to sign a consent form for the procedure to go ahead, so it’s important you feel fully informed.
What happens during a hysteroscopy?
A hysteroscopy procedure may take as little as 10 to 15 minutes, but it can take longer if you’re having treatment at the same time. Before an outpatient procedure, your doctor or nurse will ask you to remove your clothes below your waist. They may give you a gown to wear, or a sheet to cover yourself. You’ll need to lie down on a couch or special chair with your legs bent and resting in supports.
Your doctor or nurse will pass the hysteroscope through your cervix and up into your womb. Sometimes they may put a speculum inside your vagina first, to help them see your cervix. A speculum is the same instrument that’s used when you’re having a cervical smear test. It’s not always needed for a hysteroscopy. They’ll then gently pump a sterile (clean) fluid into your womb so they can see more clearly.
The camera on the hysteroscope sends video images of the inside of your womb to a monitor. Your doctor or nurse will be able to view the images and do any treatment that’s needed.
A hysteroscopy can be uncomfortable and painful. But most people find the pain is quite mild. It’s usually less painful than the worst pain you might get during a menstrual period. If you find it painful, tell your doctor or specialist nurse and they can stop. They may also be able to offer you a local anaesthetic or nitrous oxide (‘gas and air’) to help with pain relief.
What to expect afterwards
If you had an outpatient hysteroscopy and were awake during your procedure, you should be able to go home a short time afterwards. You may need to wait a little longer if you had nitrous oxide (‘gas and air’) to help with pain relief.
If you had a hysteroscopy under general anaesthesia, you’ll need to rest until the effects have worn off. You’ll usually be able to go home on the same day. But you’ll need to wait until you’ve passed urine (peed) and had something to eat and drink. You’ll need someone to take you home and to stay with you for the first 24 hours while the anaesthetic wears off. After a general anaesthetic, you may find you’re not so coordinated or that it’s difficult to think clearly. This should pass within 24 hours. In the meantime, don’t drive, drink alcohol, operate machinery, or make any important decisions.
Your nurse may give you a date for a follow-up appointment. If your doctor took tissue samples during your hysteroscopy, it may take a couple of weeks to get the results. These will usually be sent to the doctor who requested the hysteroscopy. They’ll then contact you and discuss the hysteroscopy results with you.
Recovery for hysteroscopy
If you’ve had a hysteroscopy procedure as an out-patient without a general anaesthetic, you may feel able to go back to your usual activities that same day. But you may want to take a day off work to recover. If you’ve had a general anaesthetic, you may need to rest for a few days before you get back to normal.
It’s normal to have some period-like cramping pains and some spotting or bleeding for a few days after your hysteroscopy. If you need pain relief, you can take over-the-counter painkillers, such as paracetamol or ibuprofen. You can use sanitary pads until the bleeding stops – it’s best not to use tampons. Wait until any bleeding and pain has settled down before doing any exercise or having sex. If the pain or bleeding carries on or gets worse, speak to your doctor.
Side-effects of hysteroscopy
Side-effects are the unwanted but mostly temporary effects that you may get after having the procedure.
Hysteroscopy side-effects include:
- cramping pains for a day or two – these will feel like period pains
- bleeding or light spotting from your vagina for a few days
- feeling or being sick
- feeling faint
Complications of hysteroscopy
Complications are when problems occur during or after your procedure. Hysteroscopy is usually a safe procedure, but possible complications include the following.
- Damage to the wall of your womb. This may be caused by the instruments used to look inside your womb. This usually heals on its own, but sometimes you may need another operation to repair the damage.
- Heavy bleeding during or after your hysteroscopy. If this gets worse or doesn’t stop within a week, contact your hospital or seek urgent medical advice.
- Infection. Signs may include a fever, severe pain in your tummy, and foul-smelling discharge from your vagina. An infection will be treated with antibiotics.
The risk of complications is higher if you have a hysteroscopy under general anaesthesia. You’re also at greater risk of complications if you’ve had treatments, such as the removal of a fibroid (fibroidectomy) or polyp (polypectomy).
Alternatives to hysteroscopy
Depending on your symptoms, there may be other tests available. These include the following.
- Ultrasound. You may have an abdominal ultrasound, which looks at your womb from the outside (through your tummy). Or you may have transvaginal ultrasound, in which an ultrasound probe is inserted into your vagina. But ultrasound can’t diagnose cell changes in the lining of your womb or be used to treat polyps or fibroids.
- Magnetic resonance imaging (MRI) scan. This can be another option for investigating heavy periods or abnormal bleeding.
- Pipelle biopsy. This is another way of taking a sample of the lining of your womb (an endometrial biopsy). Your doctor will put a narrow tube through your cervix and into your womb.
Your doctor will talk to you about the treatment or investigation options for you.
Worried about your gynaecological health?
Get a picture of your current health and potential future health risks with one of our health assessments.
To book or to make an enquiry, call us on 0370 218 8122
Fibroids
Heavy periods (menorrhagia)
Ultrasound
Ultrasound is a type of scan that uses sound waves to produce images of the inside of your body
Did our Hysteroscopy information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Moore JF, Carugno J. Hysteroscopy. StatPearls Publishing. www.ncbi.nlm.nih.gov/books, last updated 10 May 2022
- You and your anaesthetic. Royal College of Anaesthetists, www.rcoa.ac.uk, published February 2020
- Outpatient hysteroscopy. Royal College of Obstetricians & Gynaecologists. www.rcog.org.uk, accessed 8 September 2022
- Preparing for a hysteroscopy. Royal College of Anaesthetists. www.rcoa.ac.uk, published 2018
- Hysteroscopy. Medscape. emedicine.medscape.com, last updated 27 July 2021
- Caring for someone recovering from a general anaesthetic or sedation. Royal College of Anaesthetists, www.rcoa.ac.uk, published November 2021
- Diagnostic hysteroscopy. Medscape. emedicine.medscape.com, updated 22 June 2021
- Operative hysteroscopy. Medscape. emedicine.medscape.com, updated 22 June 2021
- Heavy menstrual bleeding: assessment and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, last updated 24 May 2021
- Mahmud A, Smith P, Clark TJ. Benchmarking services in outpatient hysteroscopy (OPH): A quality improvement project. Eur J Obstet Gynecol Reprod Biol 2021; 259:211–21. doi: 10.1016/j.ejogrb.2021.01.028
- Endometrial cancer. BMJ Best Practice. bestpractice.bmj.com, last reviewed 8 August 2022
- Best practice in outpatient hysteroscopy. Green-top guideline no. 59. RCOG/BSGE joint guideline. www.rcog.org.uk, published March 2011
- Surgery. Preoperative preparation. Oxford handbook of adult nursing. Oxford Academic. academic.oup.com, published June 2018
- Personal communication, Dr Madhavi Vellayan, Consultant Gynaecologist, 2 October 2022
- Biopsy of the womb lining. Cancer Research UK. www.cancerresearchuk.org, last reviewed 23 January 2022
- Abnormal uterine bleeding. BMJ Best Practice. bestpractice.bmj.com, last reviewed 13 August 2022
- Uterine fibroids. BMJ Best Practice. bestpractice.bmj.com, last reviewed 13 August 2022
- Victoria Goldman, Freelance Health Editor



