Fibroids
- Dr Madhavi Vellayan, Consultant Gynaecologist
Fibroids are benign (non-cancerous) growths that can develop in the walls of your womb (uterus). You can have one or more fibroids and they can vary in size. If you don’t have any symptoms from fibroids, you probably won’t need any treatment. If you do need treatment for fibroids, options include medicines and surgery.
About fibroids
Fibroids are very common – around 8 in every 10 women get them. Fibroids are made up of muscle and fibrous tissue. They usually grow very slowly over years.
When you reach the menopause, fibroids stop growing and start shrinking slowly as your hormones change.
Fibroids don’t usually cause any symptoms or complications.
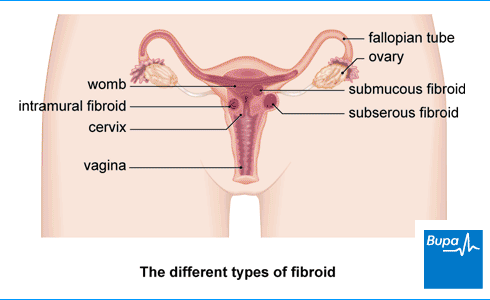
Types of fibroids
There are different types of fibroids, depending on where they grow in your womb.
- Intramural fibroids grow inside the muscle wall of your womb.
- Subserous fibroids grow from the outside wall of your womb into the space in your pelvis.
- Submucous fibroids grow from the inner wall of your womb into the space inside your womb.
Subserous and submucous fibroids can be connected to the wall of your womb by a stalk-like growth, and these are called pedunculated fibroids.
Causes of fibroids
Doctors don’t know for sure what causes fibroids. But it’s thought that certain hormones, such as oestrogen, may encourage them to grow.
You're more likely to get fibroids:
- as you grow older – your risk can increase the closer you are to your forties
- if you’re overweight
- if you’re a black woman; you’re three times more likely to get fibroids than if you’re a white woman
- if you have an unhealthy diet, or drink more than the recommended limits of alcohol
- if you have high blood pressure
Symptoms of fibroids
You might not have any symptoms from fibroids, so may not know you have them. They’re often found during a scan for something else. Whether you have any symptoms from fibroids usually depends on how big the fibroids are, and where they are.
Possible symptoms of fibroids include:
- heavy periods that can last a long time – if this happens, you can become anaemic, which may cause you to feel tired, dizzy and short of breath
- irregular periods
- painful periods (dysmenorrhoea)
- swelling in your tummy
- pain, or a feeling of pressure in your pelvis
- bloating or constipation
- needing to pee more often, or go very urgently
- problems with fertility (difficulty getting pregnant)
Fibroids are likely to cause more symptoms closer to your period. These include discomfort, bloating, pressure, and pain in your lower tummy.
If you think you may have symptoms of fibroids, contact your GP.
Diagnosis of fibroids
You may find out you have fibroids if you have a gynaecological (vaginal) examination or investigations for other problems, such as heavy periods. Or you may have symptoms and go and see a GP.
Your GP will ask about your symptoms and your medical history. They’ll examine your tummy and do a vaginal examination. During this, your GP will put on some gloves and use some lubrication to put their fingers into your vagina to gently feel for anything different in your womb or cervix. At the same time, they’ll use their other hand to press on the lower part of your tummy (abdomen). You can ask to have someone with you during the examination if you wish.
Your GP may suggest you have some tests, such as blood tests or an ultrasound scan. Depending on the results, you may be referred to a gynaecologist (a doctor who specialises in female reproductive health). Your gynaecologist may then offer you some further tests, which may include the following.
- A blood test to check if you have anaemia.
- An ultrasound scan (if you’ve not had one already). You’ll probably have two types of ultrasound scan. One looks at your womb and ovaries through your tummy using a probe. The other is a vaginal scan that uses a device that goes into your vagina. The scan may feel uncomfortable, but it shouldn’t be painful.
- A hysteroscopy. A hysteroscopy is a procedure to look inside your womb using a narrow tube-like telescope with a camera called a hysteroscope. Your doctor can take a small sample or tissue (biopsy) at the same time. And they may be able to remove small fibroids from inside of your womb.
- A magnetic resonance imaging (MRI) scan. An MRI scan can show a lot of detail about your fibroids and can be a useful test to have before surgery. You may also have an MRI scan if your gynaecologist needs more information about your condition.
Treatment of fibroids
There are several treatments for fibroids. The treatment that’s best for you will depend on your symptoms, how much these affect your life, and if you want to have children in the future.
Your treatment choice will also depend on where your fibroids are, how big they are and how many you have. If you don't have any symptoms or if your symptoms are mild, you may not need any treatment. But if you have more severe symptoms, there’s a range of treatments that may help. Your doctor will discuss these with you to help you decide the best options for you.
Medicines
Medicines can’t get rid of fibroids, but they can help to ease your symptoms. The following types of medicine may help.
- Over-the-counter painkillers. Non-steroidal anti-inflammatory (NSAID) medicines, such as ibuprofen, can help to ease your pain.
- Medicines that reduce heavy bleeding. These include tranexamic acid, the contraceptive pill, progesterone, and the levonorgestrel-releasing intrauterine system (an IUS or coil). The coil prevents the lining of your womb from growing quickly, which in turn reduces the amount of bleeding during your periods. And the contraceptive pill can help to make your periods lighter and shorter.
- Medicines that shrink your fibroids. Medicines called gonadotropin-releasing hormone analogues (GnRH analogues) can lower your oestrogen levels, which usually shrink fibroids. If you're having an operation to remove your fibroids, your doctor may prescribe these for a few months beforehand. Another type of medicine that can shrink your fibroids is called Relugolix. This is an option if you haven’t been through the menopause yet. You can take this medicine for a short time to ease your symptoms, and while you’re waiting to have surgery. Your gynaecologist will discuss this with you and offer it as an option if it is appropriate for you.
Some of these medicines can cause side-effects. Ask your doctor to explain the risks and benefits to you. Always read the patient information leaflet that comes with your medicine, and if you have any queries, ask your pharmacist or your doctor.
Surgery
There are a number of different operations and procedures that can either treat or remove fibroids. These may be the best option for you if:
- medicines don’t help to control your symptoms of heavy bleeding or pain
- your fibroids are large
- you’re getting symptoms due to pressure of fibroids on the organs around your womb
- you want to increase your chances of getting pregnant and lower your chances of a miscarriage
Operations and procedures for treating fibroids include the following.
Myomectomy
Myomectomy surgery is an operation to remove your fibroids, but which leaves your womb in place. It may be an option for you if you wish to become pregnant in the future. It’s done either through a cut in your tummy, or through keyhole (laparoscopic) surgery. During keyhole surgery, a small cut is made in your tummy and a thin tube with a light and camera is inserted to see inside. New fibroids can grow after this type of surgery.
Hysterectomy
A hysterectomy is an operation to remove your womb so you will no longer be able to get pregnant. It can be done through a cut in your tummy, using keyhole surgery, or through your vagina. A hysterectomy will get rid of all your fibroids, and they won’t grow back.
Transcervical
Transcervical resection is an operation to remove any fibroid that’s growing into the inside of your womb. It’s done using a hysteroscope, which is a narrow telescope with a light and camera at the end. This treatment won’t affect your future chances of getting pregnant.
Endometrial ablation
During endometrial ablation, your surgeon will remove the lining of your womb to reduce heavy bleeding when you have your period. At the same time, your surgeon can do a transcervical resection (see above). You should only have endometrial ablation if you no longer want children.
Uterine artery embolisation (UAE)
During UAE, a specialist in doing scans (an interventional radiologist) will inject small particles into the blood vessels that supply your fibroids. These block the blood supply which causes the fibroid to shrink. The effects of the surgery on your fertility or any pregnancy aren’t certain. So, your doctor may not recommend it if you want to have a baby. If you do go ahead and have this procedure, it’s best not to get pregnant for six months afterwards.
Magnetic resonance imaging-guided ultrasound surgery
During magnetic resonance imaging-guided ultrasound surgery, ultrasound waves are used to remove fibroids. It’s not certain yet how this procedure affects future pregnancies.
Your doctor will explain what your options are and that they involve, including how long it may take you to recover afterwards.
Complications of fibroids
Complications of fibroids can include:
- constipation and problems peeing, if large fibroids press on your bladder or bowel
- anaemia, caused by long-term heavy bleeding
- difficulty getting pregnant (infertility)
- miscarriage
- difficulties when you’re giving birth to a baby, such as your baby being in a breech position
- fibroids that are on stalks can twist and this can be painful – you may need an operation to remove the fibroid
Most people don’t get any symptoms or complications from their fibroids.
Preventing fibroids
Developing fibroids can’t always be helped, but there are things you can do that may reduce your risk. These include:
- maintaining a healthy weight – by eating a balanced diet and exercising regularly
- limiting your alcohol consumption
- taking vitamin D and vitamin A supplements
- eating less red meat – although research shows a weak association
Worried about your gynaecological health?
Get a picture of your current health and potential future health risks with one of our health assessments.
To book or to make an enquiry, call us on 0370 218 8122
After the menopause, the amount of the hormone oestrogen in your body decreases. This will usually cause your fibroids to gradually shrink, and in turn, your symptoms should get better or go away completely.
The main cause of fibroids isn’t known. But the hormone oestrogen may be involved in how they grow. Some things can increase your risk of getting fibroids, such as your age as they’re more common in your forties.
See our section on causes of fibroids above for more information.
Not always. If you don’t have any fibroid symptoms, you probably won’t need any treatment. If they’re large, you may need to have them removed in an operation. This is because large fibroids can press on your bladder or bowel and cause problems, such as constipation and problems peeing.
See our section on treatment of fibroids above for more information.
If you have symptoms from your fibroids which don’t go away after treatment, you can get surgery to remove or shrink them. There are different types of surgery to remove fibroids. Your doctor can advise you on the most suitable options for you.
See our treatment of fibroids section for more information.
You won’t need to treat your fibroids if you don’t have any symptoms. But leaving symptoms untreated for a long time could lead to complications. These may include anaemia (from heavy bleeding), infertility, miscarriage or difficulty giving birth. Most people don’t get any complications from their fibroids, but it’s best to treat your symptoms.
See our complications of fibroids section for more information.
Hysterectomy
Anaemia
Anaemia is caused when you don’t have enough red blood cells (RBCs) or haemoglobin – the part of your RBCs that carries oxygen – to meet your body’s needs.
Endometrial ablation
Heavy periods (menorrhagia)
Over-the-counter painkillers
Hysteroscopy
Painful periods (dysmenorrhoea)
Did our Fibroids information help you?
We’d love to hear what you think.∧ Our short survey takes just a few minutes to complete and helps us to keep improving our health information.
∧ The health information on this page is intended for informational purposes only. We do not endorse any commercial products, or include Bupa's fees for treatments and/or services. For more information about prices visit: www.bupa.co.uk/health/payg
This information was published by Bupa's Health Content Team and is based on reputable sources of medical evidence. It has been reviewed by appropriate medical or clinical professionals and deemed accurate on the date of review. Photos are only for illustrative purposes and do not reflect every presentation of a condition.
Any information about a treatment or procedure is generic, and does not necessarily describe that treatment or procedure as delivered by Bupa or its associated providers.
The information contained on this page and in any third party websites referred to on this page is not intended nor implied to be a substitute for professional medical advice nor is it intended to be for medical diagnosis or treatment. Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. We do not accept advertising on this page.
- Uterine fibroids. BMJ Best Practice. bestpractice.bmj.com, reviewed May 2024
- Fibroids. Patient. patient.info, accessed 3 June 2024
- Fibroids. NICE Clinical Knowledge Summaries. cks.nice.org.uk, last revised December 2018
- Personal communication, Dr Madhavi Vellayan, Consultant Gynaecologist, 17 July 2024
- Anaemia – iron deficiency. NICE Clinical Knowledge Summaries. cks.nice.org.uk, revised September 2023
- Pelvic examination technique. Medscape. emedicine.medscape.com, updated October 2022
- Heavy menstrual bleeding: assessment and management. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, updated May 2021
- Combined pill. NHS inform. nhsinform.scot, published December 2022
- Ulipristal acetate. NICE British National Formulary. bnf.nice.org.uk, accessed June 2024
- Keizer AL, Jacobs BL, Thurkow, et al. The effect of transcervical resection of submucous fibroids on menstrual blood loss: A prospective cohort study. Eur J Obstet Gynecol Reprod Biol 2022; 274:128–35. doi: 10.1016/j.ejogrb.2022.05.019
- Endometrial ablation. Medscape. emedicine.medscape.com, accessed 3 June 2024
- Uterine artery embolisation for fibroids. National Institute for Health and Care Excellence (NICE). www.nice.org.uk, accessed 3 May 2024
- Vafaei S, Ciebiera M, Omran MM, et al. Evidence-based approach for secondary prevention of uterine fibroids (The ESCAPE Approach). Int J Mol Sci 2023; 24(21):15972. Published online 2023 November 4. doi: 10.3390/ijms242115972
- Keyhole (laparoscopy) and open surgery (laparotomy). Ovarian Cancer Action, ovarian.org.uk. accessed 3 June 2024
- Annie Fry, Health Content Editor



